PRIMARY BONY DISORDERS OF THE TEMPORAL BONE
KEY POINTS
- Computed tomography is the primary tool for the evaluation of temporal bone osteodystrophies, metabolic disease, and reactive changes such as marrow hyperplasia.
- Magnetic resonance imaging may be used rarely for problem solving.
- Magnetic resonance imaging findings may go unnoticed or be confusing in these disease states.
- Imaging sometimes does not specifically explain a functional deficit caused by these conditions.
- These underlying diseases can cause complications that can have more consequences than the underlying disease or add to the morbidity of that disease.
The conditions that primarily effect bones throughout the body can express themselves in isolated form in the temporal bone. More commonly, temporal bone expression is part of a bony condition that involves more than one segment of the skull base and/or facial bones. Temporal bone involvement may also be part of a systemic process. These processes may be generally categorized as developmental/dysplastic, metabolic/dystrophic, and reactive. The unique embryology of the inner ear renders the bony labyrinth vulnerable to disorders distinct from other skull and skeletal lesions—a prime example being otosclerosis, which is discussed in Chapter 118 and dedicated to that unique entity.
Patients may present with a variety of complaints, physical findings, and functional deficits that are common in many other temporal bone pathologic conditions. The causative conditions are discussed here with regard to their specific temporal bone manifestations. Conditions are discussed in general with regard to their pathophysiology, computed tomography (CT) and magnetic resonance (MR) appearance, and treatment in Chapter 43.
IMAGING APPROACH
Techniques and Relevant Aspects
In general, these anomalies are best evaluated with standard, noncontrast, high-resolution temporal bone imaging. Specific protocols by indication appear in Appendix A. Magnetic resonance imaging (MRI) may be used adjunctively in very limited circumstances, such as when there is doubt about the diagnosis and there could be an infiltrating process with dural or other intracranial extension. Occasionally, complicating middle ear disease and cholesteatoma might be evaluated with MRI for reasons discussed in Chapter 111.
Pros and Cons
The pattern of disease and proper diagnosis will be much more apparent on CT. In fact, when diffuse, bilateral, and reasonably symmetric changes are present, even relatively advanced disease can go unnoticed on MRI. Also, more localized disease such as fibrous dysplasia can present very confusing findings, sometimes mimicking a more threatening mass on MRI, while the nature of the disease becomes quite obvious on CT. MRI really needs to be limited to problem solving in these types of disorders, as suggested previously.
RENAL OSTEODYSTROPHY
The dystrophic bony overgrowth that occurs in renal osteodystrophy can affect the facial nerve canal and internal auditory canal (IAC), producing seventh and/or eighth cranial neuropathy1 (Fig. 119.1).1
SICKLE CELL DISEASE AND THALASSEMIA
Predominantly high-frequency sensorineural hearing loss (SNHL) may occur in sickle cell disease, most likely due to impaired blood flow and resulting hypoxia or ischemia to the cochlea as a consequence of sickling and slugging of the blood. A lower incidence of SNHL is seen in thalassemia, which may be the result of IAC narrowing by bone marrow expansion rather than cochlear hypoxia.2,3
Very rare extramedullary hematopoiesis can extend from the marrow space of the petrous apex along air cell tracts to the middle ear and mastoid and cause a conductive hearing loss (CHL)3–6 (Figs. 43.5 and 119.2). If the clinical circumstances are not known, then this pattern of reactive marrow changes can mimic a cholesteatoma3 or an infiltrating malignant tumor or refractory otitis media.
PAGET DISEASE (OSTEITIS DEFORMANS)
The skull and temporal bones are commonly involved with Paget disease in those who have the disease elsewhere.6–8 Temporal bone involvement alters the position, size, and architecture of the external auditory canal (EAC), middle ear and mastoid, otic capsule, and petrous pyramid (Fig. 119.3). Middle ear involvement is more variable than that of the otic capsule.6–8 These changes commonly cause hearing loss and vestibular dysfunction and are mainly due to the typical pagetoid bone with excess osteoid and resulting soft deformed bones and microfractures.
Hearing loss can be mixed, conductive, or sensorineural. Hearing loss, including both the high frequency and degree of CHL, correlates closely with cochlear capsule bone density.7 Labyrinthine involvement is the most likely explanation for vestibular symptoms as well. The actual mechanism responsible for the conductive loss has not been clarified but is more likely related to changes in the cochlea than ossicular pathology.
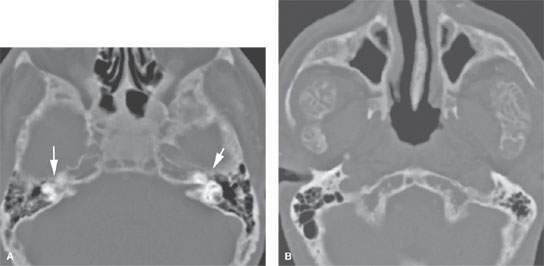
FIGURE 119.1. A, B: Changes in renal osteodystrophy involving the facial bones and skull base, including the temporal bone (arrows in A), with the potential for facial nerve compression (arrows)
Purely conductive or mixed hearing loss with a mild sensorineural component may mimic otosclerosis, prompting surgeons to offer patients middle ear exploration or stapedectomy. It is important that the treating surgeon be aware of the presence of Paget disease, as hearing generally does not improve with surgical intervention. As many surgeons do not routinely obtain radiographic imaging for adult-onset CHL without otoscopic evidence of middle ear pathology, the diagnosis of Paget may be made with radiographic imaging that is performed to evaluate the cause of unsuccessful stapedectomy.
Bisphosphonates may be used to control Paget disease. While these agents have proven efficacy for normalization of biochemical markers and skeletal symptoms such as pain, proof of their efficacy for hearing loss is lacking. There is weak evidence linking bisphosphonates with ototoxicity.
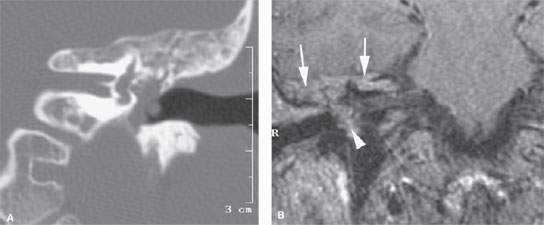
FIGURE 119.2. Temporal bone involvement with extramedullary hematopoiesis (complete case shown in Fig. 43.5). A: Computed tomography study showing abnormal tissue from the involvement of the marrow space at least partially filling the middle ear cavity. This tissue was erosive. Surgery revealed hematopoietic tissue within the middle ear. B: T1-weighted image showing the hematopoietic tissue to be of relatively high signal intensity. The component in the petrous apex and mastoid (arrows) is contiguous with the disease within the middle ear cavity (arrowhead).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








