Primary Brain Neoplasms
Todd M. Blodgett, MD
Alex Ryan, MD
Marios Papachristou, MD
Key Facts
Terminology
Low grade gliomas (LGG), astrocytomas, glioblastoma multiforme (GBM)
Imaging Findings
MR shows variable amounts of enhancement, with most low grade gliomas showing little if any enhancement
High grade tumors with extensive enhancement
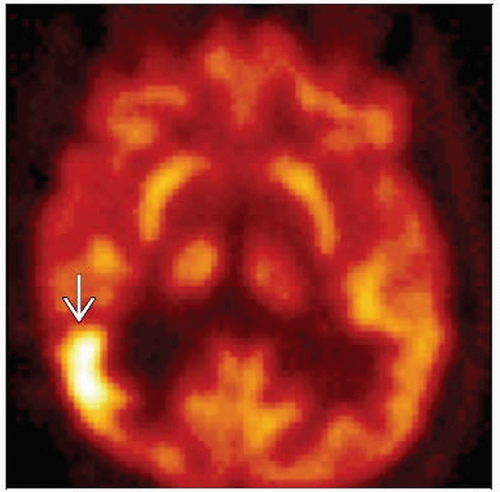
FDG PET shows little activity in low grade gliomas and increasing amounts of FDG uptake in higher grade tumors
MR is first choice to show position and extent of tumor
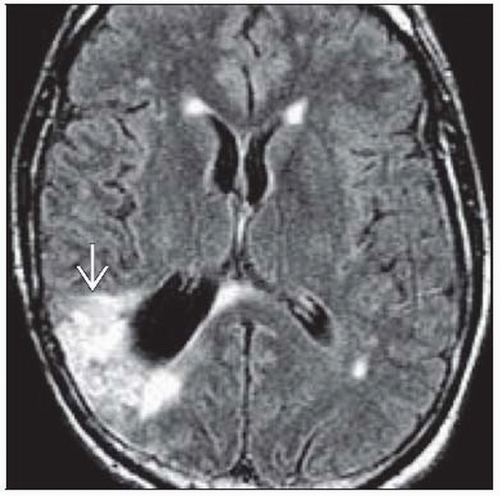
MR: FLAIR images show extent of vasogenic edema
FDG PET: Increased uptake in higher grade gliomas & astrocytomas, pilocytic astrocytomas
GBM will typically enhance and may have necrosis centrally
Low grade gliomas should have no enhancement
CNS lymphoma, high grade glioma, and metastatic tumor show enhancement on MR
Low grade gliomas show mild FDG uptake, generally more than normal white matter, much less than normal cortex
Top Differential Diagnoses
Metastases
Abscess
Infarct
Radiation Necrosis
Diagnostic Checklist
Initial imaging evaluation should include MR with contrast ± FDG PET
TERMINOLOGY
Abbreviations and Synonyms
Low grade gliomas (LGG)
Astrocytomas
Glioblastoma multiforme (GBM)
Other primary brain neoplasms
Definitions
Imaging of neoplasms of glial or astrocyte origin
World Health Organization (WHO) grade I
Most are benign
Example: Pilocytic astrocytoma
WHO grade II
Benign to semi-benign
Example: Astrocytoma and oligoastrocytoma
WHO grade III
Semi-benign to malignant
Example: Astrocytoma
WHO grade IV
Malignant
Example: GBM
Two types
Primary (de novo)
Secondary (degeneration from lower grade tumors)
IMAGING FINDINGS
General Features
Best diagnostic clue
MR shows variable amounts of enhancement
Most low grade gliomas show little if any enhancement
High grade tumors show extensive enhancement
MRS shows abnormal choline-to-creatine (Cho:Cr) ratio and decreased N-acetylaspartate (NAA)
FDG PET shows little activity in low grade gliomas and increasing amounts of FDG uptake in higher grade tumors
Location
Intra-axial
2/3 supratentorial and 1/3 infratentorial for low grade gliomas
Most anaplastic astrocytomas and GBMs are hemispheric
Size
Variable, from a few millimeters to several centimeters
Smaller tumors < 6 mm often not visualized by FDG PET
Morphology
Variably sized intra-axial tumor ± enhancement with surrounding vasogenic edema
Gliomas tend to be diffuse without sharp border, especially WHO grade II tumors
Imaging Recommendations
Best imaging tool
MR is first choice to show location and extent of tumor
MR
Primary tumor usually demonstrates extent of enhancement
Low grade tumors may not show abnormal enhancement
FLAIR images show extent of vasogenic edema
May show mass effect, hemorrhage, necrosis, and signs of increased intracranial pressure
FDG PET
Increased uptake in pilocytic astrocytomas and higher grade gliomas & astrocytomas
Can estimate grade and malignancy of tumor before operation, as well as show tumor extent and heterogeneity
Protocol advice
FDG PET
Minimize auditory and visual stimulation during FDG uptake phase
Dynamic acquisition
Additional nuclear medicine imaging options
SPECT
Other PET tracers for neurooncology (investigational)
C-11 Methionine: Amino acid transport
C-11 Tyrosine: Amino acid transport
C-11 Choline: Membrane synthesis, proliferation
F-18 Fluorothymidine: Proliferation
Correlative imaging features
CT: Variable appearance, difficult to see without contrast unless large
MR: Most primary CNS tumors will show some enhancement, except low grade gliomas (grade I-II); usually accompanied by vasogenic edema
CT Findings
General
NECT
Ill-defined mass occasionally with calcifications (up to 20% in LGG, rare in anaplastic and GBM)
Often mass may not be visible on a noncontrast study
CECT
Low grade gliomas should have no enhancement
GBM will typically enhance and may have necrosis centrally
GBM
NECT
Irregular isodense or hypodense mass with central hypodensity representing necrosis
Marked mass effect and surrounding edema/tumor infiltration
Hemorrhage not uncommon
Calcification rare (related to low grade tumor degeneration)
CECT
95% have strong heterogeneous irregular rim enhancement
Low grade astrocytoma
NECT
Ill-defined homogeneous hypo-/isodense mass
20% calcified; cysts are rare
Calvarial erosion in cortical masses (rare)
CECT
No enhancement or very minimal
Enhancement should raise suspicion of focal malignant degeneration
MR Findings
FLAIR
Typically will show a larger area of involvement representing edema
T1 C+
No enhancement with low grade tumor
Variable amounts of enhancement, mass effect, and central necrosis with GBM
MRS
Elevated Cho:Cr ratio and decreased NAA
CNS lymphoma, high grade glioma, and metastatic tumor show enhancement on MR
Nuclear Medicine Findings
Metabolic activity in primary glial and astrocytic tumors correlates with tumor grade and prognosis
Low grade gliomas show mild FDG uptake
Generally more than normal white matter, much less than normal cortex
Higher grade tumors have increasing FDG activity, with GBM being very FDG avid, as much or more than normal cortex
PET/CT neuronavigation-guided surgery can achieve total tumor resection in 31% of cases vs. 19% in conventional operation
High grade gliomas show significantly higher SUV average and SUV maximum than metastatic tumors
However, considerable overlap between these two tumors exists
FDG accumulation alone is unlikely to be adequate in clinical setting
SUV max of 15 used for cutoff of high grade glioma and lymphoma
Using cutoff SUV of 15, lymphoma can be excluded, and differential can be narrowed to high grade glioma vs. metastatic brain tumor
SUV max most accurate parameter for distinguishing CNS lymphoma from other brain tumors
CNS lymphoma typically has highest uptake of primary brain tumors
SUV in primary brain tumor dependent on variety of factors
Plasma glucose level, steroid treatment, tumor size and heterogeneity, time after injection, and previous irradiation
Steroid treatment may decrease FDG uptake in CNS lymphoma
DIFFERENTIAL DIAGNOSIS
Metastases
Primary cannot be differentiated from a metastatic lesion by imaging
Whole-body FDG PET can help identify primary lesion if outside the brain
Multiple ring-enhancing lesions
History of malignancy makes this diagnosis the most likely
Abscess
Usually cannot be differentiated by imaging
Patients usually have other infectious symptoms such as fever and elevated white blood cell count
Infarct
Little or no FDG uptake
May conform to a vascular distribution
Multiple Sclerosis (MS)
Tumefactive MS can look similar to an intracranial neoplasm
Radiation Necrosis
PET negative in most cases
In contrast, high grade tumors tend to have increased levels of FDG uptake
Vasculitis
Usually multiple smaller areas of involvement
Usually no enhancement
PATHOLOGY
General Features
Genetics: Loss, mutation, or hypermethylation of tumor suppressor gene TP53
Etiology: Variable
Epidemiology
Gliomas
Incidence is 6-8/100,000, with 50% being malignant subtypes
GBM
3-4/100,000; ≈ 50% of all gliomas are GBM
Younger patients tend to have lower grade gliomas with grade increasing in older age groups
Gross Pathologic & Surgical Features
Tumor is difficult to distinguish from normal or edematous brain tissue at operation
Percentage of complete removal by routine surgery is disappointing, leading to poor prognosis
Genuine total removal of glioma probably impossible because of diffuse growth and location
Microscopic Features
Grade depends on
Degree of cellularity
Cellular pleomorphism
Mitotic figures
Necrosis
Vascular proliferation
CLINICAL ISSUES
Presentation
Most common signs/symptoms
Various neurologic symptoms
Headaches
Seizures
Visual disturbances
Other signs/symptoms: Other symptoms related to mass effect or hemorrhage
Demographics
Age
Low grade gliomas typically occur in younger patients
Higher grade tumors typically occur in older patients
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree