Prostate and Seminal Vesicle Ultrasound
The initial enthusiasm for transrectal US (TRUS) imaging of the prostate to screen for and stage prostate cancer has dimmed considerably. Currently, in most practices, TRUS is primarily used to guide prostate biopsy and for a few specific indications, such as evaluation of male infertility and diagnosis and drainage of prostatic abscesses [1,2]. TRUS is an excellent technique for examining the seminal vesicles for diseases associated with infertility, perineal and ejaculatory pain, and hematospermia [3]. Transabdominal US imaging of the prostate through a urine-filled bladder has limited utility, but can be used to estimate prostate size.
Imaging Technique
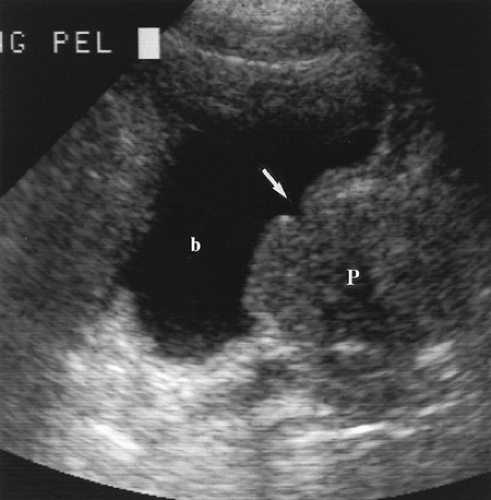
Using a transabdominal approach, the prostate is imaged through the fluid-distended bladder (Fig. 15.1). A 3.5-4.0-MHz sector transducer is positioned on the lower abdomen just above the symphysis pubis with the sound beam directed caudally. The prostate is examined in transverse and longitudinal planes. Prostate size is estimated and abnormalities, such as calcifications, can be demonstrated.
The transrectal approach allows the use of high-frequency 5-10-MHz transducers that provide the most detailed US examination. If transrectal biopsy is planned, the patient is routinely premedicated with antibiotics. No other patient preparation, such as an enema, is usually needed. The patient is placed in left lateral decubitus position with both knees flexed toward his chest and his head comfortably positioned on a pillow. Digital rectal examination is performed to judge the size of the prostate and to detect any palpable abnormalities. The endorectal transducer is coated heavily with US gel and is sheathed in a condom, which is also generously coated with US gel. The probe is gently placed into the rectum with the tip initially directed toward the sacrum to follow the curve of the rectum. Most endorectal transducers are end-fire sector format. Side-fire linear array transducers
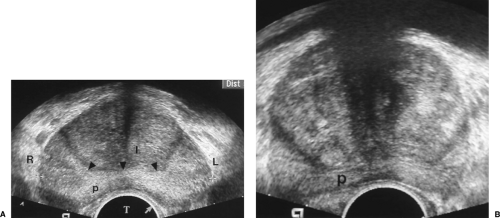
provide excellent images, but cannot be used to direct transrectal biopsy. The prostate, seminal vesicles, and periprostatic tissues are examined in transverse and sagittal planes. Color Doppler may be used to detect the vascular changes associated with prostate cancer and inflammatory conditions [4]. Images are routinely viewed inverted with the transducer
position at the bottom of the image (Fig. 15.2). The patient’s right side is depicted on the left side of the image.
provide excellent images, but cannot be used to direct transrectal biopsy. The prostate, seminal vesicles, and periprostatic tissues are examined in transverse and sagittal planes. Color Doppler may be used to detect the vascular changes associated with prostate cancer and inflammatory conditions [4]. Images are routinely viewed inverted with the transducer
position at the bottom of the image (Fig. 15.2). The patient’s right side is depicted on the left side of the image.
Anatomy
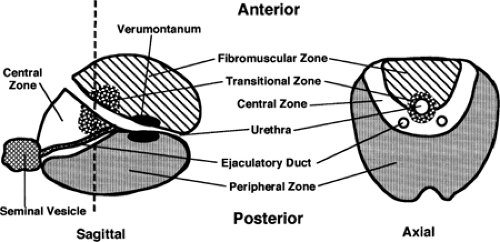
The prostate is shaped like a rounded, inverted pyramid and sits on the urogenital diaphragm, just behind the symphysis pubis (Fig. 15.3). The broader base of the prostate supports the base of the bladder (base to base). The tapered apex rests on the muscular urogenital diaphragm. The seminal vesicles lie in the posterior groove between the bladder and the prostate. The seminal vesicles are convoluted tubes coiled to form a lobulated sac (Fig. 15.4). The terminal ampullary portion of the vas deferens passes medial to and joins the seminal vesicle to form the ejaculatory duct (see Fig. 15.6). The ejaculatory ducts course from superolateral to inferomedial in the upper half of the prostate and empty into the urethra at the verumontanum. The urethra runs through anterior prostate in an arching course from the bladder neck to the prostate apex. In cross-section, the urethra is horseshoe-shaped with a posterior ridge that forms the verumontanum. In the mid-portion of the verumontanum is a 6-mm, blind-ending sac–the utricle. The utricle is the müllerian remnant that forms the uterus and vagina in the female. Prostatic ducts empty into the length of the intraprostatic urethra. The prostate is enveloped by a thin but tough fibrous capsule and is surrounded by fat and a prominent plexus of periprostatic veins.
The prostate gland is divided into three anatomic zones and an anterior non-glandular area (Fig. 15.3). The zones of the prostate can be likened to a catcher’s mitt holding a softball. The “mitt” is posterior and represents the peripheral zone (PZ). The PZ at the base of the prostate is thin, like the finger portion of the catcher’s mitt. The PZ thickens toward the apex like the bottom portion of the catcher’s mitt. The PZ encompasses only the posterolateral rectal surface of the gland, and does not extend circumferentially around the gland. The PZ contains 70% of the glandular tissue. The softball represents the “inner gland,” which consists of the periurethral transitional zone (TZ) and the pyramidal-shaped central zone (CZ). The TZ constitutes only 5% of the total glandular tissue in young men, but is the site of benign prostatic hypertrophy (BPH) and enlarges substantially in most older men. The CZ is largest at the prostate base and tapers toward the apex, constituting 25% of
the total glandular tissue. With BPH, the enlarging TZ compresses the CZ and thins the PZ. The anterior surface of the prostate consists only of fibrous and muscular tissue without acini. It is termed the anterior fibromuscular stroma and is not a site of disease.
the total glandular tissue. With BPH, the enlarging TZ compresses the CZ and thins the PZ. The anterior surface of the prostate consists only of fibrous and muscular tissue without acini. It is termed the anterior fibromuscular stroma and is not a site of disease.
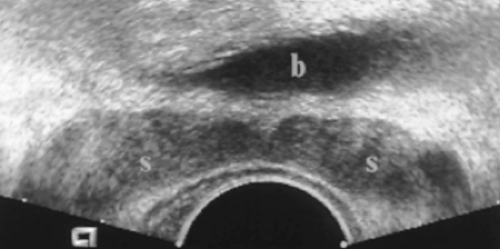 Figure 15.4 Normal Seminal Vesicles. Transverse image shows both seminal vesicles (s) with the normal “bow-tie” appearance. Slight asymmetry in size is a normal variant. b, bladder. |
Most cancer (70%) occurs in the PZ. Approximately 10% arise in the CZ and 20% in the TZ. Transurethral resection of the prostate consists of resection of the periurethral TZ tissue above the verumontanum, leaving a cavity that is continuous with the bladder lumen. Cancer in the TZ is often discovered incidentally in the tissue resected by transurethral resection of the prostate.
TRUS demonstrates the seminal vesicles as oval hypoechoic structures 3-5 cm long and 1-2 cm diameter. In axial plane, the two seminal vesicles have a bow-tie appearance (Fig. 15.4). Mild asymmetry in size is common. Marked asymmetry suggests tumor involvement in patients with prostate cancer. An acute angle between the posterior seminal vesicles and the base of the prostate is invested with echogenic fat. Loss of this acute angle suggests tumor invasion into the seminal vesicles (Fig. 15.5). The thickened ampullary portion of the vas deferens can often be seen separately from the seminal vesicles (Fig. 15.6).
In young men, the PZ is isoechoic with the TZ and CZ. With aging and hypertrophy of the TZ, the inner gland becomes enlarged and heterogeneous. The PZ then appears relatively hyperechoic and distinct. The tissue boundary between the PZ and the inner gland is termed the surgical capsule (Fig. 15.2). The urethra is identified in the midline of the prostate by looking for its V-shaped orifice at the bladder base (Fig. 15.7).
Estimates of prostate weight can be made by digital rectal examination. Measurement of prostate volume by US is easily related to weight because 1 cm3 equals 1 gm. Prostate
volume is calculated by the formula (length × width × height × 0.52 = volume). In young men the normal gland is 20 gm. In older men, the prostate is considered enlarged when it exceeds 40 gm.
volume is calculated by the formula (length × width × height × 0.52 = volume). In young men the normal gland is 20 gm. In older men, the prostate is considered enlarged when it exceeds 40 gm.
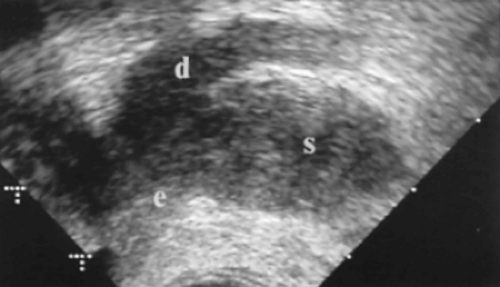 Figure 15.6 Normal Ampullary Portion of the Vas Deferens. Angled coronal image of the left seminal vesicle (s) shows the ampullary portion of the vas deferens (d). The junction of the vas deferens and seminal vesicle is the commencement of the ejaculatory duct (e).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|