Fig. 1
11C-Choline PET/CT showing increased uptake on the left side corresponding to radio-recurrent prostate cancer
4 Surgical Technique of Salvage Prostatectomy
Radical prostatectomy is the local salvage treatment modality with the longest history. Several authors described salvage radical prostatectomy to be a challenging procedure with a high probability of encountering locally advanced disease at surgery and corresponding surgical complications. Carson et al. showed the feasibility of prostatic surgery after radiotherapy with 18 patients who underwent radical prostatectomy as an adjuvant therapy after radiotherapy with acceptable surgical morbidity (Carson et al. 1980). Salvage radical prostatectomy (Fig. 2) is performed with the same technical steps described for anatomic radical prostatectomy (Walsh 1998), despite expected technical difficulties such as unclear plane of dissection and adherences, especially in the posterior aspect of the prostate, where rectal injury is a major concern (Chade et al. 2012). Yet, several authors describe that salvage prostatectomy as currently performed is similar in its degree of difficulty to standard radical prostatectomy and not as challenging as previously reported (Rogers et al. 1995; Zincke 1992; Pontes et al. 1993). However, these surgeons are usually experienced in radical prostatectomy and pelvic surgery, and none has reported an analysis of his or her learning curve with salvage prostatectomy. Moreover, there has been no report specifically addressing and comparing critical aspects of the procedure, allowing a more comprehensible evidence-based guideline (Chade et al. 2012). The feasibility of salvage prostatectomy after EBRT alone is frequently described as the same as primary radical prostatectomy (Rogers et al. 1995). Although there is no evidence to confirm any difference in complications according to the method of radiotherapy (EBRT vs. brachytherapy), authors eventually describe greater difficulty and surgical complexity at salvage prostatectomy after brachytherapy because of increased adhesions (Gotto et al. 2010).
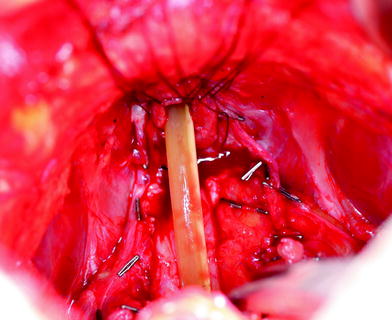
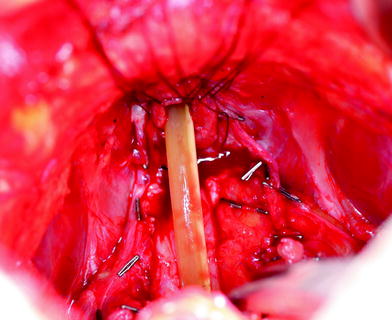
Fig. 2
Intraoperative aspect after salvage radical prostatectomy with a catheter and anastomotic sutures in the urethral stump. On the right side there are brachytherapy seeds in the Denonvilliers fascia. On the left side the neurovascular bundle could partly be preserved
5 Oncologic Outcomes of Salvage Prostatectomy
As salvage radical prostatectomy is technically demanding, experienced surgeons are needed to optimize outcomes. Accordingly, relatively few centers have reported on salvage radical prostatectomy. The study with the largest number of patients is a recently published multi-institutional collaboration project that included high volume referral centers (Chade et al. 2011). In a systematic review of salvage prostatectomy the median follow-up of the reported studies ranged from 18 to 84 months, which may explain the wide variation in findings of oncologic outcomes across those studies with less biochemical control in studies with longer follow-up. Thus critical analyses should be limited to those studies with longer follow-up periods (Chade et al. 2012). None of the published studies on salvage prostatectomy adequately studied potential oncologic differences between salvage prostatectomy after external beam radiotherapy and after brachytherapy or between distinct radiotherapy techniques (three-dimensional conformal radiotherapy, intensity-modulated radiotherapy) or radiotherapy doses (Chade et al. 2012).
Table 1 summarizes the specimen characteristics of some of the largest salvage prostatectomy series. Positive surgical margin rate varied from 11 to 36 %. Pathologic organ confined disease was reported in 25–71 % of studies. Lymph node dissection was reported infrequently in the studies and was not standardized among different institutions. Also, no studies were able to analyze the impact of pelvic lymph node dissection on cancer-specific survival.
Table 1
Specimen characteristics of contemporary open salvage prostatectomy series
Series | Number of patients | PSA (ng/ml) | pT2 (%) | ≥pT3 (%) | pT3b (%) | PSM (%) | Gleason-score | Lymph node metastasis (%) | ||
|---|---|---|---|---|---|---|---|---|---|---|
≤6 | 7 | ≥8 | ||||||||
Multicenter (Chade et al. 2011) | 404 | 4.5 | 45 | 53 | 30 | 25 | 14 | 37 | 24 | 16 |
MSKCC/Baylor (Bianco et al. 2005) | 100 | 5.9 | 35 | 23 | 33 | 21 | 17 | 62 | 13 | 9 |
Mayo Clinic (Ward et al. 2005) | 121 | 8.5 | N/A | 61 | N/A | 21 | 14 | 59 | 27 | N/A |
USC (Sanderson et al. 2006) | 51 | 8.0 | 25 | 59 | N/A | 36 | 20 | 36 | 44 | 16 |
Aachen (Heidenreich et al. 2010) | 45 | 7.8 | 71 | 11 | 18 | 11 | 33 | 47 | 20 | 20 |
Wayne State (Gheiler et al. 1998) | 38 | 14 | 39 | 61 | 29 | 13 | N/A | N/A | N/A | 16 |
Rome (Leonardo et al. 2009) | 32 | 2.3 | 53 | 47 | N/A | 34 | 38 | N/A | N/A | 0 |
The 5-year biochemical recurrence-free survival rates typically range from 50 to 60 % in most salvage prostatectomy series. At 10 years, the biochemical recurrence-free probability ranges from 37 to 47 %. The definition of biochemical-free recurrence after salvage prostatectomy was different in almost each publication. Table 2 summarizes the oncologic outcomes of some of the largest salvage prostatectomy series. Series from single centers reported probabilities of cancer-specific survival from 65 to 77 % at 10 years (Bianco et al. 2005; Ward et al. 2005; Sanderson et al. 2006), while the multi-institutional collaboration study reported an 83 % cancer-specific survival at 10 years (Chade et al. 2011). Overall survival varied from 54 to 89 % at 10 years (Chade et al. 2012).
Table 2
Oncologic outcomes of contemporary open salvage prostatectomy series
Series | Number of patients | Follow-up (years) | PSA > 10 ng/ml (%) | Time to RP (months) | pT2 (%) | Disease-free rate (%) | Cancer-specific survival | ||
|---|---|---|---|---|---|---|---|---|---|
5 years | 10 years | 5 years | 10 years | ||||||
Multicenter (Chade et al. 2011) | 404 | 4.4 | N/A | 41 | 45 | 48 | 37 | 92 | 83 |
MSKCC/Baylor (Bianco et al. 2005) | 100 | 5 | 29 | 40
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||||