Proximal Humerus Fractures and Shoulder Dislocations
Proximal humerus fractures represent up to 5% of all fractures, and they most often occur in an elderly person with osteoporosis as the result of a fall. Their incidence is increasing with the aging of the population. The proximal humerus may also be fractured in younger patients, usually as the result of high-energy trauma. In this circumstance, there is a high incidence of associated injuries, including neurovascular lesions of the injured arm and injuries of the cervical spine and chest. Over the past decade, there has been ongoing controversy about the relative merits of operative versus nonoperative treatment for proximal humeral fractures, as well as uncertainty about whether better results are achieved with internal fixation or hemiarthroplasty.1–4 Improved surgical techniques and implants for both reduction and fixation of proximal humeral fractures and for shoulder hemiarthroplasty after fracture have been developed,5–7 and outcome studies are now being performed that will help dictate treatment of these diverse injuries.8
Dislocations of the glenohumeral joint are also common and affect persons of all ages. The goal of treatment is expedient reduction with recovery of full function. The natural history of shoulder dislocation with respect to the risk of recurrent dislocation continues to be defined.9,10 Young patients with traumatic dislocation are those most likely to develop recurrent instability. Although early surgery is traditionally not considered, arthroscopic evaluation of the recently dislocated shoulder may play a role in defining lesions associated with late instability and may enable early repair, with decreased morbidity from chronic instability.11,12 Elderly patients often have an associated injury to the rotator cuff with both fractures and dislocations; if present, surgical repair should be considered.11,13
Fractures of the Proximal Humerus
The overriding principle in the treatment of proximal humeral fractures is the need to restore a functional range of motion and to permit the activities of daily living that the specific patient performs. Shoulder movement depends on the relative gliding of the humeral head, rotator cuff, bursal tissue, and deltoid muscle. Capsular restriction or loss of these gliding surfaces will render the shoulder stiff and painful and lead to a poor outcome. The importance of early mobilization following even nondisplaced fracture of the proximal humerus has been demonstrated.14 Improved results are seen when active mobilization is allowed before 14 days after injury, compared with delayed mobilization.14 If a fracture of the proximal humerus is either unacceptably displaced or too unstable to allow early motion, then operative intervention should be considered in any patient who needs or wants to regain useful function of the shoulder. Whether this is best done by reduction and fixation of the fracture or by prosthetic replacement of the shoulder depends on the patient′s needs and expectations, the fracture pattern, the bone quality, the implants available, and the experience of the surgeon. Stabilization of the proximal humerus in polytrauma patients by methods that allow early motion and weight bearing on the injured limb continue to be advocated, and devices such as intramedullary nails and locking plates have been developed that may allow this to be done with less invasive techniques.15 However, there are no high-quality comparative studies of these new techniques, either to each other or to nonoperative management, to help guide the surgeon. Thus, when treating a proximal humeral fracture, surgeons cannot rely on demonstrated evidence-based guidelines and must use their experience and judgment to decide upon treatment.
Classification
The management of proximal humeral fractures begins with a thorough assessment of the functional needs and abilities of the patient, the presence of cognitive or physical impairments, the fracture pattern, the bone density, the patient′s expectations, and the ability of the patient to comply with a rehabilitation program. The goal of treatment is to obtain fracture union and maintain function of the shoulder, while avoiding complications. The skills of the surgeon and the resources available must also be considered.
The complex anatomy of the shoulder girdle must be understood in order to successfully treat proximal humerus fractures and shoulder dislocations. Fractures of the proximal humerus occur in typical patterns that are influenced by muscular insertions that cause predictable displacement of each fragment (Fig. 14.1). The muscular and neurovascular anatomy of the proximal humerus also influence treatment and complications.

The classification proposed by Neer16 remains the standard for the evaluation and discussion of these injuries. It considers the presence of displacement or angulation of each of the four major segments of the proximal humerus: the humeral head, the greater tuberosity, the lesser tuberosity, and the shaft. A major drawback of this classification is that a minimally displaced fracture line may not be considered a “part” under the Neer system, but still may require operative attention. The AO/Orthopaedic Trauma Association (OTA) classification system emphasizes the blood supply to the humeral head and has 27 subdivisions that enable a very specific identification of fractures. However, the nomenclature of this fracture is alphanumeric rather than descriptive and is difficult to apply and understand.
Proximal humerus fractures have proven to be very difficult to classify in a reproducible manner, with several studies documenting poor inter- and intraobserver reliability. The reliability is not improved with simplified classification schemes or the additional use of computed tomography (CT).17–20 Four-part fractures are commonly subclassified because the valgus-impacted type appears to have a better prognosis than other types of four-part fractures.7
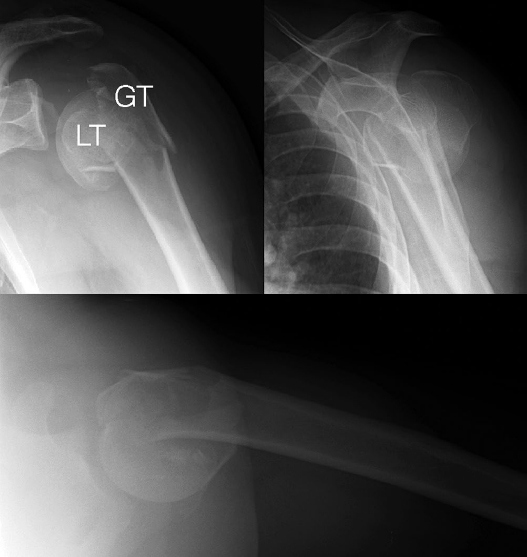
The diagnosis of a fracture of the proximal humerus is straightforward. The patient presents with pain, swelling, and bruising about the shoulder after an injury. The diagnosis is confirmed with imaging. Initially, plain radiographs are obtained, consisting of the well-known shoulder trauma series: true anteroposterior (AP) and lateral X-rays in the plane of the scapula and the axillary lateral view (Fig. 14.2). Although the importance of the axillary view in classifying the fracture has been highlighted,21 one should be aware of the limitations of this view. Patients and technologists are often reluctant to obtain the axillary view because of pain and the need to move the injured arm, and it has been shown that the axillary radiograph does not accurately represent the amount of angulation of the surgical neck that is present.22 An alternative to the axillary view is to take a similar image in the opposite direction, with the arm kept immobilized in a sling, or to utilize the transverse cuts of a CT scan. In either case, the axillary view or axial CT image confirms that the shoulder is reduced, demonstrates debris within the joint, diagnoses glenoid fractures, and reveals the amount and direction of displacement of the tuberosities.

Even though advanced imaging may not improve classification reliability, CT is a useful and sometimes necessary adjunct to the assessment of the proximal humerus for the treatment of a specific fracture.23 It provides valuable information about the degree of comminution, the presence of intra-articular fracture lines, the presence of glenohumeral subluxation or articular impaction, and whether the lesser tuberosity is fractured (Fig. 14.3). With respect to clinical decision making, a key distinction is between the so-called three- and four-part fractures, which influences the viability of the humeral head.23 It may be unclear on plain radiographs whether the lesser tuberosity is a separate fragment or not. When the lesser tuberosity is not fractured and remains attached to the humeral head, some blood supply to the humeral head can be assumed to be intact, and this knowledge may influence decisions regarding treatment. If the lesser tuberosity is displaced in addition to the greater tuberosity, the fracture is classified as a four-part fracture, and the prognosis and treatment are instead determined by the high likelihood of avascular necrosis that follows this injury.23

One particular fracture pattern has been recognized that is worthy of special consideration. In 1991, Jakob et al24 described the four-part valgus impacted fracture of the proximal humerus. This fracture is easily recognized by the “popsicle” appearance of the articular segment that has fallen into the void left by displacement of the greater tuberosity, so that the articular surface faces superiorly (Fig. 14.4). In this circumstance, despite comminution, soft tissue attachments to the articular segment remain intact at the medial periosteal hinge that both facilitate fracture reduction and maintain the viability of the articular segment. In their initial description of this fracture, Jakob et al noted that the rate of osteonecrosis was just 26% in their series of 19 such fractures, lower than typically expected in a series of four-part fractures.

Nonoperative Treatment
For proximal humeral fractures, the lack of consistently successful surgical techniques and the frequent complications associated with traditional techniques of operative management have led to a large number of these patients being treated nonoperatively. The majority of proximal humeral fractures are minimally displaced. These stable fractures may be managed with only brief immobilization in a sling (Fig. 14.5). Functional exercises are begun when pain permits. Koval and coworkers14 have shown that institution of therapy within 14 days leads to improved functional outcomes.

A systematic review of the nonoperative treatment of proximal humeral fracture published in 2011 identified 12 studies reporting 650 patients.25 The rate of radiographic healing was 98% and the complication rate was 13%; varus malunion was the most common complication. Only 13 cases of osteonecrosis were observed. A meta-analysis of the treatment of three- and four-part fractures found that conservatively managed patients had more pain and worse range of motion than those managed by either fixation or arthroplasty.2 Court-Brown et al26 reported a series of 125 valgus-impacted fractures treated nonoperatively. One year after injury, 80% of the primarily elderly patients had a good to excellent outcome, despite residual deficits in strength and range of motion. In further support of non-operative management, Edelson et al27 studied the results of 63 severe proximal humeral fractures that are usually treated operatively, and found that at between 2 and 9 years of follow-up, motion was very limited, but pain was minimal and the patients were satisfied with their level of function.
Indications
Fractures that are treated nonoperatively should be stable enough to allow early functional use and be minimally displaced (Fig. 14.5). At the time of the initial evaluation, the arm should be examined to ensure that the proximal part of the humerus can be moved, with motion occurring at the shoulder joint and not at the fracture site. There should not be significant posterior and/or superior displacement of the greater tuberosity; uncorrected displacement of the tuberosities has adverse effects on rotator cuff function, whereas surgical neck malunion, specifically varus, may affect range of motion. A patient with reasonably high functional demands and a displaced proximal humeral fracture will be better treated with surgery so that early range of motion can be instituted. A recent report found that a lateral neck-shaft angle of less than 55 degrees on the initial or 1-week postinjury X-ray was predictive of poor functional outcomes.28
Reduction/Splinting Techniques
Tuberosity displacement is difficult to reduce nonoperatively. The exception is a tuberosity fracture associated with shoulder dislocation; in this case reduction of the shoulder dislocation may effect reduction of the tuberosity as well.
Displaced surgical neck fractures can sometimes be reduced by applying longitudinal traction to the arm with the arm in an adducted position. Adduction of the humerus neutralizes the deforming force of the pectoralis muscle insertion on the distal fragment. If the fracture can be impacted and remains in a stable position, nonoperative management would be appropriate.
Functional Bracing
Functional bracing per se is not feasible in proximal humeral fractures because of the significant deforming forces of the many muscular insertions on the various fracture fragments. In rare instances, it might be feasible to immobilize the arm in a so-called airplane splint with the shoulder abducted or forward-elevated position. Because such a position is poorly tolerated, there is little indication for this manner of treatment.
Rehabilitation
Early institution of functional range of motion is important in order to achieve the best outcomes. Koval et al14 showed improved outcomes when such exercises were begun within 14 days of injury. Their protocol consisted of the use of a sling for initial pain relief. All patients were seen again within 1 week after the injury, were given instructions for range-of-motion exercises for the arm, and were referred to a physical therapist. The physical therapist supervised active range-of-motion exercises for the elbow, wrist, and hand combined with passive range-of-motion exercises for the shoulder twice a week. The shoulder exercises were begun with the patient in the supine position for forward elevation, external rotation, and internal rotation to the chest. In addition, patients were asked to perform the exercises up to four times daily at home. The sling was continued for 4 to 6 weeks until the fracture had united clinically. Once the sling was discontinued, active range-of-motion exercises were initiated, starting with the patient in the supine position and gradually progressing to a sitting position. Finally, isometric deltoid and rotator-cuff strengthening exercises were added. Once reasonable active motion of the shoulder was achieved, resistive exercises for the deltoid and rotator-cuff muscles were added. Approximately 12 weeks after the fracture, a more vigorous stretching program was begun. More recently, a randomized trial compared early mobilization 3 days after injury to conventional immobilization for 3 weeks in patients with impacted proximal humeral fractures, and found that the early mobilization group had better Constant scores and greater forward elevation, with no difference in complications.29
Surgical Treatment
Indications
In general, the literature does not provide much high-quality evidence comparing the results of nonoperative treatment to those of specific surgical techniques. Although the Neer classification is often used for surgical decision making, a more descriptive approach is followed here, based on an understanding of the fracture lines and displacements. Fractures of the proximal humerus can be thought of as involving the surgical neck and the tuberosities. In turn, fracture displacement affects the biomechanical function of the shoulder and the vascularity of the fracture fragments. Both aspects must be considered for each fracture fragment identified. Another key aspect of decision making is the stability of the fracture; stable fractures are considered to be those that will tolerate early functional motion. In general, surgery is indicated when fracture instability would prevent early functional use, or when the fracture pattern has concerning features as discussed below.
Surgical neck fractures can be nondisplaced or displaced, and simple or comminuted. Displaced surgical neck fractures should be treated with correction of translational displacement and angulation. A variety of useful fixation techniques exist, including plate fixation, percutaneous pins, tension band wires, and intramedullary nailing with either flexible or interlocking devices (Fig. 14.6). Occasionally, hemiarthroplasty or reverse total shoulder replacement is the preferred option; discussion of these techniques is beyond the scope of this chapter. The ideal choice of fixation for a given patient depends on many factors, including the degree of comminution, the bone quality, and the experience of the surgeon. Isolated anatomic neck fractures are exceedingly rare, and may be treated with pin or screw fixation in young patients or hemiarthroplasty in the elderly. More often, so-called anatomic neck fractures are described in association with more complex injuries that also involve the tuberosities and the metaphyseal region (Fig. 14.7). In these injuries, the metaphysis is comminuted and the articular segment remains as a well-defined fragment. Surgical indications in these more complex fractures are more controversial and are discussed later in this section.

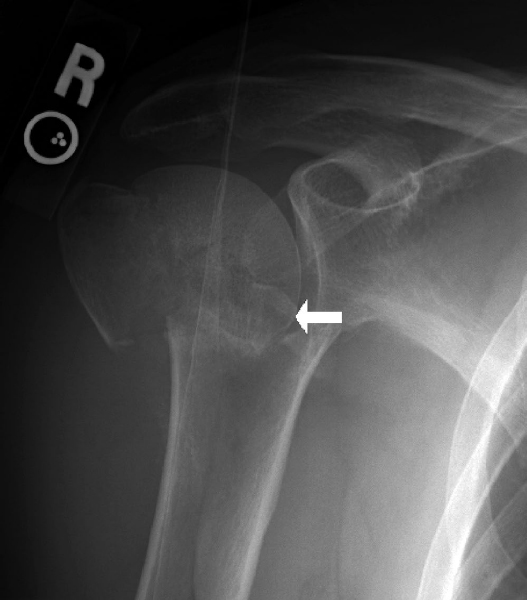
Isolated greater tuberosity fractures are often associated with anterior shoulder dislocation. After fracture, the greater tuberosity fragment typically displaces superiorly and/or posteriorly. Posterior displacement is more difficult to assess on radiographs, and CT scanning may be necessary. Both patterns of displacement are associated with potential impingement against the acromion. Displaced tuberosity fragments should be reduced and fixed (Fig. 14.8). The degree of acceptable displacement is controversial. One study suggested that displacement of as little as 3 mm is associated with impingement symptoms in athletic individuals.30 It is well accepted that more than 5 mm of displacement is an indication for surgery in patients who require overhead function of the arm. Tension-band techniques using wire or heavy suture have excellent results (Fig. 14.9); screw fixation may be considered when comminution is minimal, the fragment is relatively large, and the bone quality good. One should remember that rotator cuff tears are associated with displaced tuberosity fractures, and rotator cuff repair should be performed when such fractures require surgery. Isolated lesser tuberosity fractures are rare and may occur with posterior dislocations. Large fragments of the lesser tuberosity may require open reduction and fixation if they are displaced.


Many proximal humeral fractures consist of various combinations of these more elementary fracture patterns. So-called three-part fractures generally represent the combination of a surgical neck fracture and greater tuberosity fracture (Figs. 14.4 and 14.5). For these injuries, treatment results are related primarily to the degree of residual tuberosity displacement or head and neck angulation.23 Avascular necrosis may occur in up to 27% of three-part fractures, but is often asymptomatic because only a portion of the humeral head is involved (Fig. 14.10).23 Therefore, treatment of three-part fractures of the proximal humerus should be based on the biomechanical consequences of the fracture, rather than on concerns about the vascularity of the humeral head.23 In a patient who requires functional restoration of the injured arm, reduction of displaced tuberosity fragments and correction of malalignment of the humeral head are necessary (Fig. 14.6). Any technique can be utilized for the repair of the surgical neck fracture, combined with tension-band fixation of the greater tuberosity.31

In contrast, avascular necrosis is a more common sequelae of four-part fractures, and typically results in complete involvement of the humeral head and pain and stiffness.23,32 In addition, the poor bone quality and degree of comminution usually associated with these fractures makes open reduction and internal fixation (ORIF) of these injuries prone to failure. Therefore, for displaced four-part fractures, treatment is based on biological principles rather than mechanical principles, and many experts recommend hemiarthroplasty. However, several authors report successful results with open reduction and limited internal fixation for four-part fractures, and this treatment should be considered in more active patients.31 Interestingly, complications after operative repair of valgus-impacted four-part fractures seem to be much less frequent than in other types of four-part fractures, and these fractures are a good indication for internal fixation.7 When a valgus-impacted fracture is identified, one must carefully look for evidence of lateral displacement of the humeral head fragment (Fig. 14.11).7 If this occurs, the medial periosteal vessels that perfuse the articular segment may in fact be ruptured, and avascular necrosis is more likely to result. In the absence of lateral displacement of the humeral head fragment, the humeral head is likely to remain viable. However, a study has shown that the results of nonoperative treatment of valgus-impacted fractures are also satisfactory.26 Randomized clinical trials are necessary to completely define the indications for surgical treatment of valgus-impacted fractures; until such data are available, surgeons must rely on their own judgment and the wishes of the patient. It has been shown that the severity of symptoms associated with avascular necrosis correlate the best with the residual displacement of the fracture fragments. If the humeral head anatomy has been restored following fracture, the clinical results of patients who develop avascular necrosis is comparable to patients without avascular necrosis.32
Indications for shoulder hemiarthroplasty are classically the displaced four-part fracture in an elderly patient, four-part fracture dislocations, “head-splitting” fractures, and fractures with significant articular impaction (Fig. 14.12). Certain displaced three-part fractures in patients with severe osteoporosis have also been considered for arthroplasty, but newer techniques of fixation are changing the indications for these fractures for which osteonecrosis is uncommon. Because of the problems achieving stable fixation of the tuberosities during hemiarthroplasty, reverse shoulder arthroplasty has been recommended by some for proximal humeral fractures in the elderly.33 However, high-quality evidence in support of this approach is lacking, and reverse arthroplasty should be considered an investigational technique at this time.

Surgical Anatomy
There are two main approaches to the surgical reconstruction of proximal humeral fractures: open or percutaneous. Open procedures are mostly done through the utility deltopectoral approach (Fig. 14.13), although the anterolateral acromial “deltoid splitting” approach has gained popularity34,35 (Fig. 14.14).


Surviving the Night
The main concern with the emergent management of proximal humerus fractures or dislocations is ensuring that neurologic or vascular compromise is not occurring due to fracture displacement or joint dislocation. High-energy-mechanism injuries are more prone to neurovascular injury, but this must be ruled out in all patients regardless of mechanism. The brachial artery is located medial to the proximal humerus in the axilla and is relatively tethered at this location, so its patency must be ensured. Radial pulses should be examined for symmetry, and brachial-brachial indices can be performed with a threshold of 0.9 to rule out arterial injury. If these clinical tests are abnormal, emergent vascular surgery consultation should be obtained for immediate exploration and repair prior to any further diagnostic testing. Prophylactic forearm fasciotomy should be performed following vascular reconstruction.
Brachial plexus injury can also occur after proximal humerus fracture. In the setting of neurologic compromise, fracture and joint reduction should be performed immediately to minimize nerve compression time and maximize the chance of functional recovery. This often requires general anesthesia and potentially an open surgical procedure. Brachial plexus exploration is rarely indicated, and should involve a neurologic surgeon colleague.
More controversial is the situation of a fracture-dislocation without evidence of neurologic or vascular injury. General orthopaedic principles dictate acute reduction of all joint dislocations to decompress adjacent soft tissue structures. However, when the glenohumeral joint is dislocated and there is a fracture of the proximal humerus, a closed reduction is rarely possible. If an open procedure is required for reduction, most surgeons would agree that definitive fixation of the fracture should be performed at that time to avoid a second anesthesia. The difficulty is that fracture reduction and fixation, especially with a concomitant dislocation of the humeral head, is often a lengthy, complex, and unforgiving procedure. This is often best done during standard daytime operating hours, when the surgical setting is optimal. For this reason, many of these injuries are treated the following day.
Percutaneous approaches are used for pinning of the proximal humerus and for interlocking screw insertion when intramedullary nails are used. The main concern with percutaneous approaches is the risk of iatrogenic injury to branches of the axillary nerve (Fig. 14.15).36,37 The axillary nerve exits the quadrilateral space and arborizes on the undersurface of the deltoid. In a cadaveric study assessing the risk of percutaneous pinning, the proximal lateral pin was found to be a mean of 3 mm from the axillary nerve.37 Additional anatomic structures at risk of injury from anterior pins include the long head of the biceps tendon (mean 2 mm from the anterior pin; in three of 10 specimens the tendon was impaled) and the cephalic vein (mean distance 11 mm; perforated in one instance). Finally, tuberosity pins were 6 to 7 mm from the axillary nerve and posterior humeral circumflex artery respectively.37 Similar concerns apply to antegrade nails; blunt dissection and the use of drill sleeves will make interlocking screw insertion safer. Despite these theoretical risks, clinically significant neurovascular complications are very rare.

There are few significant risks with the deltopectoral approach (Fig. 14.13). The cephalic vein defines the delto-pectoral interval and should be identified and retracted laterally with the deltoid muscle. During deep dissection, an important landmark for the deltopectoral approach is the coracoid process and its associated strap muscles. The long head of the biceps tendon serves as a reference to identify the lesser (medial to the tendon) and greater tuberosity (lateral to the tendon). During the initial exposure and mobilization of the fracture, one should keep in mind that important vascular contributions to the articular segment are made by the arcuate branch of the anterior humeral circumflex artery that ascends along the bicipital groove, as well as the rotator cuff insertions (Fig. 14.13).
With the anterolateral acromial approach, the deep interval is between the anterior and middle heads of the deltoid. Approximately 6.5 cm from the edge of the acromion, the anterior motor branch of the axillary nerve crosses from posterior to anterior along with the posterior humeral circumflex artery, and these are the main structures at risk with this approach. The incision extends from just posterior to the anterolateral corner of the acromion distally in line with the humeral shaft. When marking the skin incision, the approximate position of the axillary nerve can be marked on the skin at 65 mm distal to the palpable edge of the acromion (Fig. 14.16).34 The subcutaneous layer is dissected to the level of the deltoid fascia, and the deltoid fascia is incised. At this point, the avascular raphe that separates the anterior and middle heads of the deltoid is identified and developed (Fig. 14.17). The two heads of the deltoid are split along the raphe, working proximal to distal while keeping an eye on the skin marking of the nerve to anticipate its position. Deep to the deltoid and proximal to the level of the nerve, the bursal tissue is encountered (Fig. 14.18). The bursa is then incised to expose the lateral fracture line and the footprint of the greater tuberosity for the plate. With valgus injury patterns, the articular surface is often visualized within the wound (Fig. 14.19). In varus injury patterns, the cancellous surface of the humeral head fragment can be accessed for reduction instruments. Deep to the anterior head of the deltoid, the subscapularis tendon can be controlled with sutures if a lesser tuberosity fracture is present. Additional sutures may be placed in the superior and posterior rotator cuff to control the greater tuberosity fragment, or to assist in reduction and stabilization of the humeral head fragment in two-part fractures (Fig. 14.20).





Although fracture patterns are quite variable, the proximal humerus fractures into fairly consistent fragments (Fig. 14.1). Most often, there are fracture lines in the region of the surgical neck and comminution of the greater tuberosity. The articular segment will be displaced in a manner that is dictated by the remaining soft tissue attachments to the humeral head and the type of injury. Careful assessment of the fracture anatomy and the displacement of the humeral head will often lead to a logical plan for the steps needed to reduce the fracture. For example, in a valgus-impacted fracture, the greater tuberosity is displaced and the humeral head “falls” into the resultant void. There is often an intact medial soft tissue attachment between the humeral head and shaft. Reduction of this fracture requires restoration of the normal position of the humeral head by pushing proximal and medially on the lateral aspect of the humeral head, thereby rotating the humeral head on the intact soft tissue hinge. Once the humeral head is reduced, the greater tuberosity may be reduced into its bed, after which it serves to maintain reduction of the humeral head.
Surgical Techniques
General Considerations
Patients undergoing surgery for repair of proximal humeral fractures should receive prophylactic antibiotics within an hour of surgery. Multiply injured patients should have their cervical spines cleared because of issues with positioning of the head during surgery. The fixation of all devices in the proximal humerus is limited by the frequent osteopenia of the humeral head associated with these injuries. In a biomechanical study, the strength of screw fixation was related to screw position within the humeral head.38 Using paired cadaveric specimens, it was found that the pull-out strength was greatest when the screws had subchondral fixation in the center of the humeral head.
Studies of biomechanics have evaluated the relative strength of various methods of fixation of the proximal humerus.5 When plate fixation is performed, the use of a fixed-angle plate appears to be better than a standard buttress plate. Koval et al6 compared 10 fixation techniques for fractures of the proximal humerus, using both fresh-frozen and embalmed cadaver specimens. In the frozen specimens (representing patients with good bone quality), the T-plate provided the strongest fixation. In the embalmed specimens (representing patients with osteoporosis), the Enders nail/tension band technique provided the strongest fixation. In both types of bone, tension band fixation alone provided the least effective fixation.6 In an osteotomy model, the addition of calcium-phosphate cement improved the strength of fixation after pinning or use of either a cloverleaf or blade plate, even in osteoporotic bone.39
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree