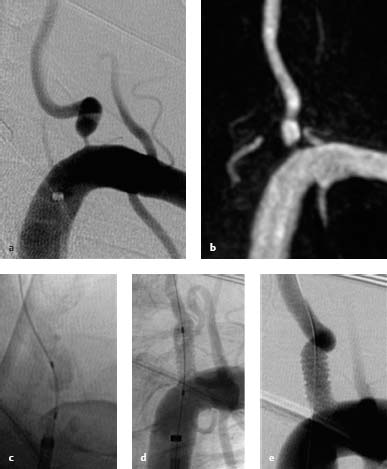
14 Proximal Vertebral Artery Stenosis The vertebral artery can be divided anatomically into four segments (V1-V4). Some authors additionally designate the origin of the vertebral artery from the subclavian artery as V0. • V1 segment: extends from the origin of the vertebral artery from the subclavian artery to the site where the vertebral artery enters the transverse foramen, generally at the level of the C6 vertebra • V2 segment: ascends through the transverse foramina (from C6 to C1) • V3 segment: extends from above the transverse foramen at C1 to the entrance into the dura at the level of the foramen magnum • V4 segment: intradural segment of the vertebral artery extending to its junction with the opposite vertebral artery to form the basilar artery The vertebral artery has an average diameter of 3–5 mm. Asymmetry between the right and left arteries is common. Approximately 50% of the population have a dominant left vertebral artery, 25% have a dominant right vertebral artery, and 25% have arteries of equal diameter. Up to 15% of the population constitutionally have only one vertebral artery. Usually, the vertebral artery is the first branch arising from the proximal subclavian artery. A left vertebral artery arising directly from the aortic arch between the origin of the left common carotid artery and the left subclavian artery is the most common variant (4–5% of the population) (Koenigsberg et al. 2003). Other rare anatomic variations are a direct origin of the vertebral artery from the aortic arch distal to the left subclavian artery, an origin from the subclavian artery distal of the thyrocervical trunk, an origin of the right vertebral artery from the right common carotid artery, or a duplication of the vertebral artery, which may involve any of the arterial segments. Likewise, the localization of the vertebral artery’s origin from the subclavian artery is variable. The vertebral artery arises from the superior aspect of the subclavian artery in approximately half the population and from the posterior aspect in the remaining half. In a small percentage of cases the vertebral artery arises from the inferior aspect of the subclavian artery. The vertebral artery is frequently elongated and tortuous, especially in its V0/V1 segment. Equally to the anterior circulation, this phenomenon correlates with the patient’s age and the presence of arterial hypertension. Atherosclerotic stenoses of the extracranial vertebral artery are common. The incidence in the general population is not exactly known, but in patients with cardiovascular diseases they have been found at autopsy in 25–40% (Wityk et al. 1998). The origin of the vertebral artery (V0/V1) is considered a site of predilection for atherosclerotic stenosis. Plaques often begin in the subclavian artery and extend into the proximal vertebral artery. In correlation to the anterior circulation, histologies of the atherosclerotic lesion in the proximal vertebral artery are diverse (fatty deposits, fibrous plaques, calcified or complicated lesions) (Castaigne et al. 1973). Ulcerations within the atherosclerotic plaques are less common in the proximal vertebral artery than in the intradural vertebral artery or internal carotid artery. Risk factors for atherosclerotic stenosis of the extracranial vertebral artery correspond to the known risk factors for cardiovascular disease such as arterial hypertension, diabetes mellitus, age, and smoking. Here too, males are predominantly affected by a 2:1 ratio (Zaytsev et al. 2006). Other causes of proximal vertebral artery stenosis such as fibromuscular dysplasia, aortoarteritis, radiotherapy, and dissection are rare. An involvement of the V1 segment is evident in 23% of patients with a vertebral artery dissection (Wityk et al. 1998). However, dissections rarely originate at the ostium. Approximately one-fifth of all ischemic cerebral strokes occur in the vertebrobasilar territory. Hemodynamically significant proximal vertebral artery stenosis is found in 20% of patients with vertebrobasilar ischemia. In 9% of patients, no cause other than a proximal vertebral artery stenosis can be found for the ischemic event, although the stenosis should be well tolerated considering the anatomic conditions with possible compensatory collateral flow of the contralateral vertebral. Three possible mechanisms could account for posterior circulation ischemia in patients with a vertebral artery stenosis: • Artery-to-artery embolism (considered the most frequent cause) • Hemodynamic insufficiency • Occlusion of the vertebral artery Contrary to the long-held belief that transient ischemic attacks in the vertebrobasilar territory have a more benign course than in the internal carotid artery (ICA) territory, it has been found that the opposite is true: Transient ischemic attacks and ischemia in the vertebrobasilar system have a poor prognosis with a 5-year risk of stroke of 22–35%, especially in the acute phase (Wehman et al. 2004). The mortality of ischemic events is also markedly higher in the vertebrobasilar territory (20–30%) than in the anterior circulation. Hence, the diagnosis and management of vertebral artery stenosis play an important role in stroke patients. Unlike carotid artery stenosis, valid criteria for the grading of vertebral artery stenosis have not yet been established. Randomized studies have shown that the risk of stroke and benefit of vascular surgery or endovascular therapy depends on the degree of carotid artery stenosis (> 70%). It is still unclear whether there is a similar threshold for proximal vertebral artery stenosis beyond which the risk of stroke rises markedly, and the potential benefit from interventional treatment is evident. Furthermore, the considerably smaller lumen of the vertebral artery compared with the carotid artery makes it more difficult to evaluate the degree of vertebral artery stenosis. For these reasons a simple classification for proximal vertebral artery stenosis is commonly used: either ”present” (50–99%) or ”not present” (< 50%). Occasionally, the stenosis is further classified as ”none” (< 50%), ”moderate” (50–69%), or ”high-grade” (70–99%). Digital subtraction angiography (DSA) is still considered the gold standard for the diagnosis of proximal vertebral artery stenosis despite the ~1% risk of iatrogenic periprocedural stroke. Noninvasive imaging modalities for the diagnosis of proximal vertebral artery stenosis are ultrasound (Doppler and duplex scanning), CT angiography (CTA), and MR angiography (MRA). Due to the smaller vessel lumen and lesion localization, imaging of proximal vertebral artery stenosis is technically more challenging than for carotid stenosis. The above-mentioned imaging modalities offer different logistic advantages and disadvantages. Ultrasound is a noninvasive, cost-effective, widely available modality that has an established track record in the evaluation of vascular stenosis (carotid, renal, femoral arteries). In contrast to the anterior circulation, where the cutoff values are exactly defined in 10% increments for carotid artery stenosis (Widder and Göortler 2004), proximal vertebral artery stenoses are graded on the basis of approximate values. Peak systolic velocity (PSV) is considered the most sensitive parameter. The following cutoff values are used (Hua et al. 2009): • For < 50% stenosis: PSV > 85 cm/s • For 50–69% stenosis: PSV > 140 cm/s • For 70–99% stenosis: PSV > 210 cm/s Evaluation of the proximal vertebral artery using ultrasound is frequently limited by the anatomic conditions and, due to the method, it is operator-dependent. Moderate flow disturbances at the vertebral artery origin are frequent nonpathologic findings, as the vessel usually arises at a right angle. Hence, luminal narrowing can only be directly evaluated when the vessel is normo- or hyperplastic and the vessel walls are clearly delineated. Doppler and duplex sonography thus have lower sensitivity and specificity than CTA and contrast-enhanced MRA. CTA is generally regarded as a valid method for the evaluation of proximal vertebral artery stenosis. As shoulders are located at the same level as the vertebral artery origin, artifacts commonly occur, but can be eliminated by increasing the tube current (210 mA). One advantage of CTA over conventional angiography is that postprocessing allows the vessel to be evaluated in all planes in three-dimensional (3D) renderings. On the other hand, calcified plaques can lead to overestimation of stenosis when plaques are superimposed on the contrast-filled vessel lumen, especially in maximum intensity projection (MIP) reconstructions (Farrés et al. 1996). Furthermore, the technique involves the known disadvantages of CT (radiation exposure and use of iodinated, possibly nephrotoxic, contrast medium). Two different methods are available for MRA of the cervical vessels: noncontrast-enhanced time-of-flight (TOF) MRA and contrast-enhanced MRA. TOF MRA provides a flow-dependent view of vessels and thus yields information on flow characteristics. The proximal vertebral artery is often elongated or tortuous and thus shows decreased signal intensity due to saturation and/or de-phasing of spins. For this reason, TOF MRA is not the method of choice for evaluating vertebral artery stenosis. Contrast-enhanced MRA, on the other hand, has proved to be a valid method, equivalent to CTA, for evaluating proximal vertebral artery stenosis. As in CTA, images can be reconstructed in all planes and rendered in 3D views. Contrast-enhanced MRA can also supply information on the plaques causing the stenosis. Disadvantages are current MRI-associated problems such as cost efficiency, contraindications in patients with metal implants (e.g., cardiac pacemakers), and claustrophobia. Three main options are available for the treatment of proximal vertebral artery stenosis: • Conservative medical therapy • Surgical treatment • Endovascular treatment by percutaneous transluminal angioplasty or stenting The medical treatment options for proximal vertebral artery stenosis consist of antiplatelet and anticoagulant drugs. The goal of medical therapy is to prevent embolism. Drugs cannot improve the decreased blood flow that results from a hemodynamically significant stenosis (Spetzler et al. 1987). The efficacy of antiplatelet drugs in the vertebrobasilar system has not been systematically investigated so far, but a protective effect similar to that in the carotid system can be assumed. The effect of anticoagulant therapy on proximal vertebral artery stenosis has also not been investigated in clinical trials, but it carries a significant additional risk of hemorrhage, especially in patients with underlying atherosclerotic disease (Sandercock et al. 2003). It is very rare for proximal vertebral artery stenosis to be treated surgically, because of the difficulty of surgical access (Crawley et al. 1998). Three vascular surgical techniques are available for vertebral artery reconstruction: • Detaching the vertebral artery distal to the stenosis and reimplanting it in the ipsilateral carotid or subclavian artery • Endarterectomy • Patch grafting Overall perioperative morbidity and mortality are relatively high (—20% of patients; Phatouros et al. 2000). The following complications have been described (Kline and Berguer 1993): Horner syndrome (15% of patients), lymphocele (4%), recurrent laryngeal nerve palsy (2%), thrombosis (1%), chylothorax (0.5%), and death (up to 4%). Secondary patency rates in these (few) patients were 95% at 5 years and 91% at 10 years. The endovascular treatment options for proximal vertebral artery stenosis are balloon dilatation (percutaneous transluminal angioplasty) and/or stent placement. High restenosis rates (10–75%) have been reported with balloon dilatation (Crawley et al. 1998). Therefore, the current endovascular options for proximal vertebral artery stenosis are balloon angioplasty plus stenting or primary stent placement. The latter method employs balloon-mounted stents and coated or uncoated coronary stents. The intervention usually has a high technical success rate and provides good initial clinical results. Again, however, the main limiting factor is a high rate of restenosis of ~30% (0–67%) (Vajda et al. 2009). The indications for treatment of proximal vertebral artery stenosis are still controversial, as data from large randomized studies are lacking. Medical therapy is still considered the first-line treatment. Today the indication for endovascular treatment is acknowledged in symptomatic patients with proximal vertebral artery stenosis refractory to drug therapy, despite the known limitations of endovascular techniques. Factors that also influence patient selection are degree of stenosis, the angiographic morphology of the stenosis (e.g., ulceration), the collateral supply, patient age (Mukherjee and Pineda 2007), and the presence of bilateral vertebral artery stenosis or unilateral stenosis coexisting with contralateral vertebral artery hypoplasia (Brückmann et al. 1986). Asymptomatic patients are almost always managed with drug therapy. Proximal vertebral artery stenosis showing short-term progression may be an indication for endovascular therapy in selected cases even in asymptomatic patients. According to stenting of carotid stenosis (see Treatment, p. 103), vertebral artery stenting should be preceded by dual antiplatelet therapy, e.g., 100 mg aspirin + 4 x 75 mg clopidogrel the day before the intervention and platelet aggregometry (Multiplate) performed on the day of the intervention. Activated clotting time (ACT) should be measured at the start of the intervention to monitor the efficacy of anticoagulation. The patient receives a weight-adjusted bolus of unfractionated heparin (60 U/kg body weight) to achieve a target ACT twice the baseline value or > 250 s. Further ACT determinations are also recommended over time. When the ACT reaches a value of > 250 s, the stenosis can be crossed with the wire. Fig. 14.1a–e Filiform stenosis of the proximal left vertebral artery. a Pretreatment DSA. b Pretreatment MRA. c The stenosis is crossed with a Choice PT wire, then predilated with a 2.5-mm Maverick balloon inflated to 14 atm. A TAXUS 5.0 stent (coated) is deployed and dilated to the nominal pressure of 9 atm. d DSA (without contrast) after stent placement confirms expansion of the proximal vertebral artery stenosis. e Subtracted view after stent placement
Anatomy
Etiology of Stenosis
Diagnosis
Invasive Studies
Digital Subtraction Angiography
Noninvasive Studies
Doppler and Duplex Ultrasound
CT Angiography
MR Angiography
Treatment
Indications
Endovascular Therapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree