and Clarisse Dromain2
(1)
Department of Radiology, San Giovanni Hospital, Roma, Italy
(2)
Department of Radiology, Institut de Cancerologie Gustav Roussy, VilleJuif – Paris, France
Abstract
Rectal adenocarcinoma accounts for about 30 % of colorectal cancers. The most common type of rectal cancer is adenocarcinoma, which is a cancer arising from the mucosa. Because of its specific anatomical location, this cancer poses two specific problems in terms of treatment that are the sphincter preservation and locoregional recurrences. The latter depends mainly on the depth of involvement of the rectal wall and mesorectum and of the lymph node involvement.
Rectal Carcinoma
Rectal adenocarcinoma accounts for about 30 % of colorectal cancers. The most common type of rectal cancer is adenocarcinoma, which is a cancer arising from the mucosa. Because of its specific anatomical location, this cancer poses two specific problems in terms of treatment that are the sphincter preservation and locoregional recurrences. The latter depends mainly on the depth of involvement of the rectal wall and mesorectum and of the lymph node involvement.
Symptoms of rectal carcinoma typically include rectal bleeding and anemia which are sometimes associated with weight loss.
The indication for treatment is based on the initial assessment of imaging including endorectal ultrasonography, thoraco-abdominopelvic CT, and rectal MRI. The aim of imaging is to identify groups of patients with different risk of recurrence and to choose the most appropriate treatment. It must respond more specifically to three questions:
What is the exact location of the tumor and the distal margin between the lower pole of the tumor and the sphincter? Its importance is crucial in reaching the lower rectal tumors to assess the possibilities of conservative treatment and thus the potential to preserve continence. Sphincter preservation is possible if you have a distal margin of at least 1 cm.
What is the stage and the circumferential resection margin? The lateral extension of the tumor is now considered the main risk factor for local recurrence.
What are the tumor N (nodal) and M (metastases) staging?
Rigid sigmoidoscopy, corresponding to the insertion of a rigid optical scope inserted through the anus, is usually performed and allows obtaining biopsy specimen and a more exact measurement of the tumor’s distance from the anus than flexible sigmoidoscopy. Low, middle, and upper rectal tumors are localized between 0 and 5 cm, 5 and 10 cm, and 10 and 15 cm from the anal margin, respectively. The tumor will be also located in relation to the pouch of Douglas. It is also important to specify the location of the tumor in the axial plane and whether the invasion is circumferential or localized.
Endorectal ultrasonography is presently the most accurate imaging modality for visualization of the layers of the rectal wall and for the assessment of tumor ingrowth into rectal wall layers with accuracies for T staging varying between 69 and 97 %. However, its sensitivity was shown to be affected by T stage and is higher for staging of superficial rectal tumors (T1 and T2) than for staging of advanced rectal cancer. Moreover, it has a limited value to visualize the mesorectal fascia and to assess the distance from the tumor to this fascia that is, at present, considered to be the most powerful predictor of local recurrence rate.
MRI has become a complementary tool for the determination of circumferential resection margin particularly useful in the staging of T3 and T4 and to assess the rectal sphincter in tumor of the low rectal cancer. Technically, rectal MRI is based on T2 sequences in the three spatial planes (sagittal, coronal, and oblique axial perpendicular to the long axis of the tumor) without fat saturation to obtain a good contrast between the tumor and the mesorectal fat. Most staging failures with MR imaging occur in the differentiation of T2-stage and borderline T3-stage lesions. Overstaging is often caused by desmoplastic reactions, and it is difficult to distinguish on MR images between spiculation in the perirectal fat caused by fibrosis alone (stage pT2) and spiculation caused by fibrosis that contains tumor cells (stage pT3). Finally for low rectal tumors, it is necessary to evaluate the sphincter complex composed of the levator ani muscle, with a beam ileococcygeal and beam puborectalis, and external and internal sphincters of the anal canal (Fig. 1). This sphincter complex is well depicted using MRI. The levator ani muscle and the external sphincter consist of striated fibers hypointense on T2 sequence, whereas the internal sphincter is a smooth muscle layer following the internal rectal muscularis that strongly enhanced after injection of contrast material.
< div class='tao-gold-member'>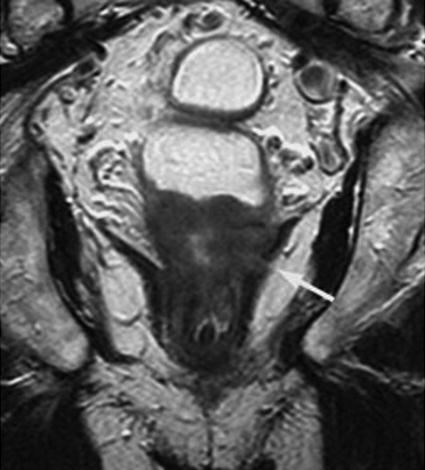 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree