Fig. 6.1
In a 40-year-old woman with clinically severe UC confirmed by sigmoidoscopy, disease distribution up to the hepatic flexure is grossly estimated on supine plain abdominal radiograph (a), with moderately dilated transverse colon. In a 56-year-old man with ASC, upright (b) and supine (c) plain films show extensive involvement of the transverse, descending and rectosigmoid colon by mural thickening with abnormal mucosal pattern, absent haustra and some foreshortening
The classical definition of toxic megacolon (TM) indeed represents the end of the spectrum of ASC, and is defined as a total or segmental non-obstructive dilatation of the colon (>6 cm), associated with systemic toxicity that occurs in approximately 5 % of patients with ASC. In recent decades, earlier diagnoses, improved intensive medical treatment and timely surgery, have dramatically reduced the incidence of TM complicating UC. At imaging, TM may be suggested by extensive, unchanging colonic distension with loss of haustral pattern resulting from transmural ulceration with destruction of the myenteric plexus and apparent mural thickening with frequently appreciable “thumbprinting sign”. The entire colon may be involved, but changes are usually most apparent in the transverse colon which is the least-dependent segment of the colon. Early colectomy is indicated when no improvement is observed within 24 h [3–5].
In a recent study, CT findings did not differ significantly between patients who required surgery and those who were not operated, and had therefore a minor impact on the decision to perform colectomy in patients with ASC [6]. Conversely, our personal experience confirms that MDCT is increasingly requested to further investigate patients with acute presentations of known IBD. Although with the drawback of ionizing radiation and intravenous contrast medium, MDCT quickly provides a comprehensive assessment of the entire abdominal and pelvic organs, peritoneum, intra-abdominal fat and lymph nodes. Furthermore, routine image reconstruction (Fig. 6.2) along coronal and sagittal planes provides a panoramic visualization of intestinal abnormalities, associated mesenteric and extraintestinal changes or complications, with sub-millimetre spatial resolution reproducing the classical orientation of double-contrast barium enema which is familiar to most surgeons.
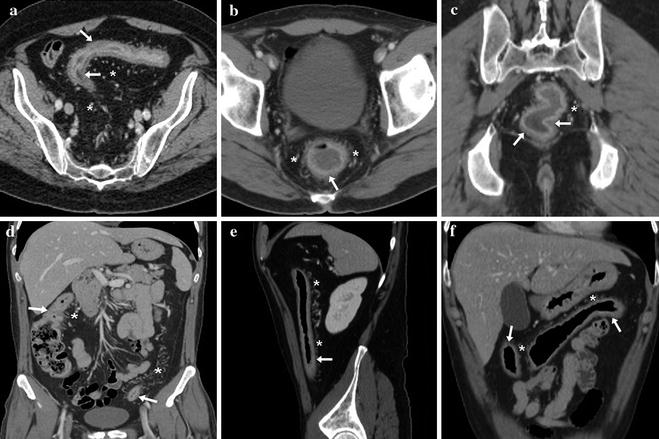
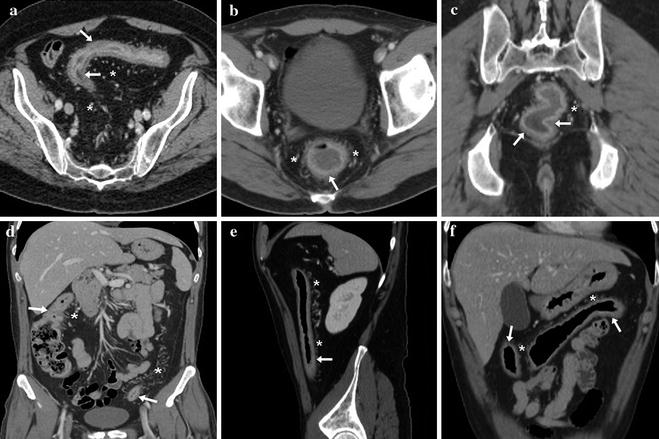
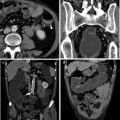
Fig. 6.2
A 75-year-old male with known UC and acute abdominal pain. Urgent contrast-enhanced MDCT (a) is requested to exclude other co-existent intra-abdominal diseases, and allows to effectively stage proctosigmoiditis by showing moderate mural thickening with stratified “water halo” appearance (arrows), associated proliferation and hypervascularization of pericolonic fat (*). In a different patient, a 49-year-old male, similar MDCT changes (b–f) are detected throughout the rectum, sigmoid, descending and transverse colon, up to the transition between hepatic flexure and ascending tract, leading to diagnose pancolitis. In both patients, perforation, peritoneal effusion and abscesses are confidently excluded thus allowing medical treatment
Despite being primarily a mucosal disease, UC is commonly characterized at MDCT by mural colon thickening, which is of moderate entity (6–9 mm), circumferential and symmetric in the majority of cases (Figs. 6.2, 6.3 and 6.4). Wall thickening is positively associated with endoscopic, clinical and histopathological severity [5, 7, 8].
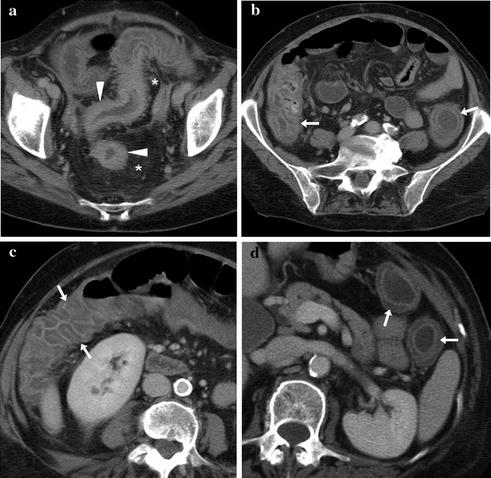
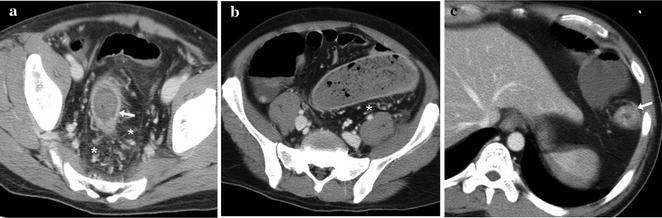
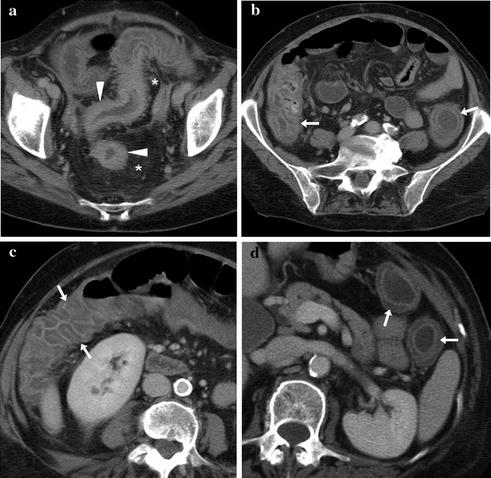
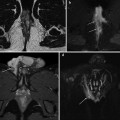
Fig. 6.3
A 65-year-old woman with clinical diagnosis of acute severe UC (ASC). Contrast-enhanced MDCT effectively depicts severe enhancing mural thickening of the rectosigmoid colon (arrowheads in a) and associated perivisceral fat changes (*), plus stratified oedematous mural thickening throughout the descending, transverse and right colon (arrows in b, c, d), allowing diagnosis of severe pancolitis and obviation of endoscopy
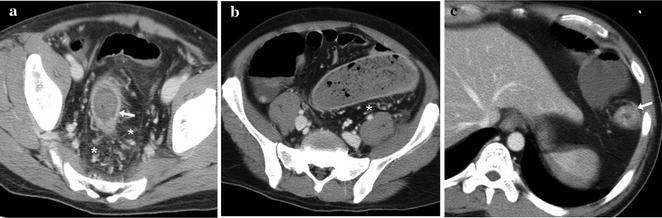
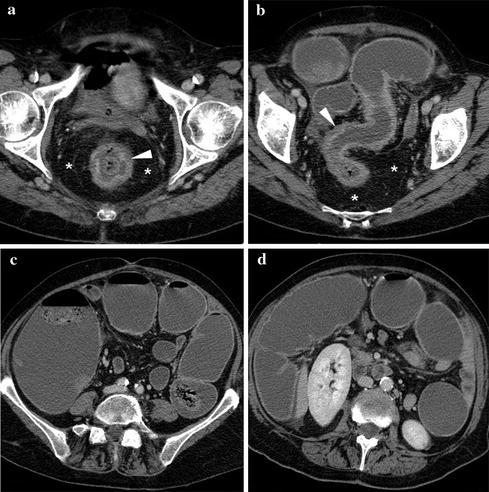
Fig. 6.4
A 42-year-old male with clinical suspicion of ASC. Contrast-enhanced MDCT visualizes moderate colonic mural thickening (arrows) of the rectosigmoid (a)and descending colon, up to the splenic flexure (detail in c), with segmental dilatation of the sigmoid colon (in b) and associated perivisceral fat changes (*). Failure to respond to medical treatment led to perform urgent colectomy
Colonic mural stratification is seen in approximately 70 % of cases. During ASC, the stratified appearance is due to mucosal hyperenhancement (corresponding to endoscopic erosion and ulceration changes) coupled with thickened oedematous submucosa. The resulting “target” or “water halo” sign best seen in transverse planes, characterized by a low-attenuation intermediate ring, represents acute inflammatory disease (Figs. 6.2 and 6.3). Most usually, UC changes show a continuous distribution from the rectum (which is spared in 4 % of cases only) to the left-sided (Fig. 6.2) or the entire colon (Fig. 6.3) [7–10].
Conversely, the “fat halo sign” mural stratification with a fat-density intermediate ring corresponding to widening and adipose infiltration of the colon submucosa that separates the bowel mucosa from the outer soft-tissue muscularis propria and serosa, represents chronic stages of UC [9–11].
Additionally, extraintestinal MDCT changes characteristically observed in UC include proliferation of pericolonic fat with hyperaemia and vascular engorgement, a slightly increased attenuation (10–20 HU) compared to normal abdominal fat due to oedema and inflammation, often containing nodular densities corresponding to enlarged lymph nodes (Figs. 6.2, 6.3, 6.4 and 6.5), most consistently identifiable in the perirectal area [7, 12].
Get Clinical Tree app for offline access
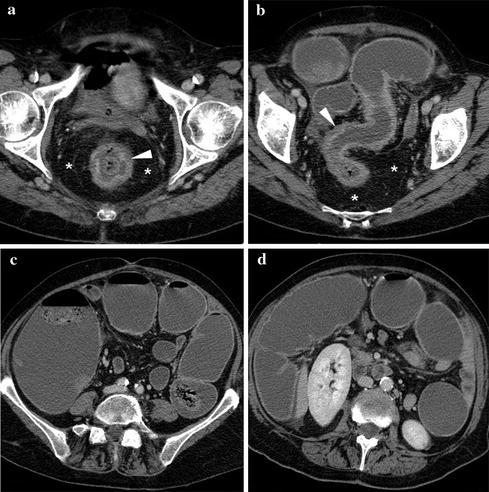
Fig. 6.5
A 69-year-old female with known UC, investigated with WE-MDCT using limited bowel preparation during an acute disease exacerbation. The rectum and sigmoid colon show circumferential mural thickening (arrowheads) with “water halo sign” appearance (a




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree