Interventional Radiology and the Transplant Kidney
Renal transplant complications have traditionally been managed by open surgical techniques. There havebeen many advances in minimally invasive techniques over the last 10-20 years, which include endourology, laparoscopy, and interventional radiology. This chapter will focus on the role and contribution of interventional radiological techniques.
Renal transplants are more challenging than native kidneys in several respects, and transplant patients requiring interventional radiology should be referred to a transplant center where they can benefit from a team approach and the appropriate expertise. A transplant is a precious commodity, and often the most effective management is reached after discussion between the nephrologist, the transplant surgeon, and the interventional radiologist.
 Summary point:
Summary point:
The main interventional radiology techniques for renal transplants are:
- Biopsy
- Drainage and sclerosis
- Renal angioplasty and stenting
- Nephrostomy
- Ureteric dilatation and stenting
- Embolization
Patient Preparation
Informed consent is essential; the risks and benefits should be openly discussed with the patient before embarking on an interventional procedure. Many of the procedures described in this chapter are best performed with the patient under conscious sedation; this will allay the patient’s anxiety and pain and generally make the whole procedure less of an ordeal for all concerned. The present authors’ preferred medication is diamorphine 2-5mg and midazolam 1-10mg given intravenously. It is essential that all patients are appropriately monitored with pulse oximetry, blood pressure measurement, and ECG. It is equally important that a dedicated member of staff in the interventional room is responsible for monitoring these vital signs. This person should not be the radiologist, scrub nurse, or radiographer.1 Drugs which reverse the effect of diamorphine and midazolam, i.e., flumazenil 200-600 μg (Roche, UK) and naloxone 0.8-2 mg (Dupont, UK), must always be available in the room. Any coagulopathy should be corrected to ensure the international normalized ratio (INR) is below 1.5 and the platelet count above 50,000×109/l. Prophylactic antibiotics should be administered for most procedures (excluding biopsy and angioplasty), including the relief of an obstructed urinary tract and drainage of collections, which are often infected or can become infected as a result of catheter manipulation. Fatal septicemia following simple procedures such as nephrostomy have been reported. The present authors prefer a broad-spectrum antibiotic such as cefuroxime 750 mg given intravenously immediately prior to the procedure.
 Summary point:
Summary point:
Preprocedural preparation:
- Informed consent
- Fast for six hours (fluids permitted)
- Check and correct coagulopathy
- Periprocedural antibiotics (except for percutaneous transluminal angioplasty and biopsy)
Requirements for conscious sedation:
- Pulse oximetry
- Pulse and blood pressure monitoring
- ECG monitoring
- Dedicated personnel
- Midazolam 1-10 mg (reversal agent flumenazil)
- Diamorphine 2.5-5 mg (reversal agent naloxone)
- Antibiotic (cefuroxime 750 mg)
Biopsy
Percutaneous biopsy of a renal transplant is normally straightforward as the kidney occupies a relatively superficial anterior position. Ultrasonography should be used to guide the marking of the skin and measure the target depth or, better, to guide needle placement under real-time guidance. The needle should avoid any major vascular structures and the collecting system and provide a suitable core of cortex and medulla. If an uncorrectable coagulopathy is present, a plugged biopsy or transvenous approach should be used.
Complications of Biopsy
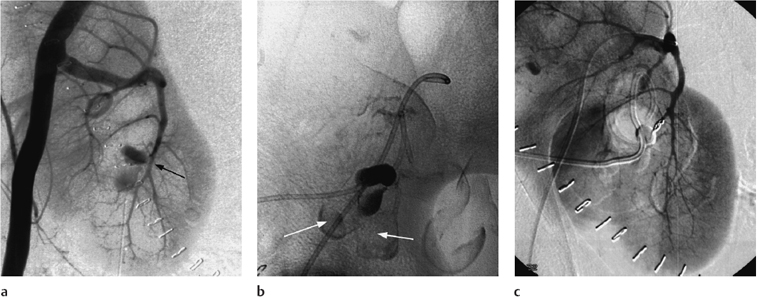
Although percutaneous biopsy is very safe, arteriovenous fistulae, arteriocalyceal fistulae, and pseudoaneurysms are recognized complications. Arteriovenous fistulae (AVFs) are common, occurring in up to 10% of biopsies, butare usually small; the majority close spontaneously. Persistent AVFs are much less common; again, the majority do not cause any adverse clinical sequelae. Treatment is only indicated if an AVF persists and causes complications such as significant hypertension or deteriorating renal function. Transcatheter embolization is a highly effective technique and should be performed as selectively as possible to minimize the loss of normal renal tissue (Fig. 6.1). The useof2-to3-Fr coaxial catheters, such as the Tracker system (Boston Scientific, UK), allows the AVF to be precisely catheterized and 1- to 3-mm microcoils can be placed until the AVF is closed. A microcatheter has the additional advantage of minimizing arterial spasm, which can be problematic and can even prevent successful embolization. A color Doppler ultrasound scan the following day should confirm successful occlusion.
Arteriocalyceal fistulae are less common but are more likely to produce symptoms such as persistent hematuria (Fig. 6.1). Although they can close spontaneously, more urgent interventionmayberequiredifthe hemorrhage is severe.
A pseudoaneurysm caused by biopsy trauma to a peripheral branch of the transplant artery may rupture into the subcapsular or perirenal space and requires urgent embolization.
Calculus Disease
Calculi occur in approximately 1.5% of renal trans-plants.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree