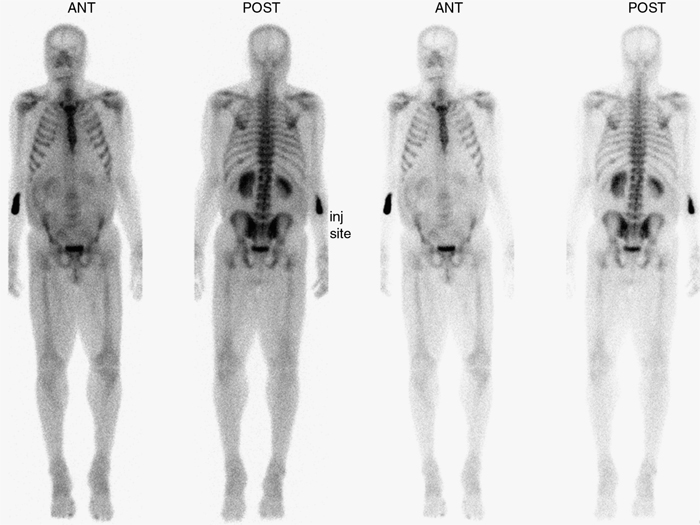
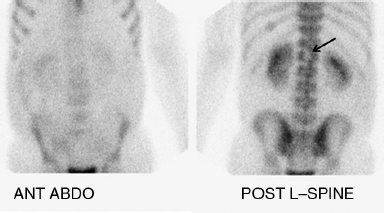
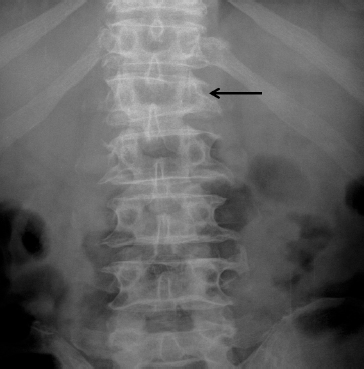
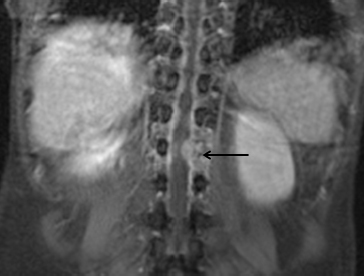
7 Introduction to Radionuclide Imaging A working knowledge of radionuclide imaging is important for success in the FRCR 2B examination and beyond. The 2010 specialty training curriculum of the Royal College of Radiologists has listed “interpretation of normal and abnormal results of commonly performed [radionuclide] investigations across all clinical systems” as a core skill.1 Anecdotal experience suggests that candidates are usually confronted with at least one radionuclide study, either in the long case or in the viva section. Beyond the FRCR 2B examination, radiologists in the United Kingdom are likely to be involved in radionuclide imaging regardless of subspecialty interest, often by being asked to review studies in a multidisciplinary meeting or in making recommendations for further imaging options. Furthermore, a U.K. national survey demonstrated that radiologists have been major providers of the nuclear medicine service in the country.2 Bone scans are the most common general radionuclide examination performed in the United Kingdom, with lung, kidney, thyroid, and cardiac studies constituting the majority of non-positron emission tomography (PET) radionuclide examinations performed.3 PET/computed tomography (CT), specifically with fluorine 18-fluorodeoxyglucose (FDG), is increasingly available and used particularly in oncological application. It is difficult to predict what would be shown in the FRCR 2B examination, but it is likely to reflect the relative “prevalence” of examinations normally reviewed by the radiologist. Other radionuclide examinations may only be presented during discussion of cases (e.g., candidates may be expected to be aware of the use of MIBG studies to complete the staging of neuroblastomas shown on a CT, ultrasound, or MRI sequence), and a limited knowledge pertaining to the significance of the examination may be all that is required of the candidate. Like other cases selected for the examination, the radionuclide cases shown may represent an uncommon presentation of common pathology or a common presentation of unusual diseases. Some cases may demonstrate a constellation of apparently disparate findings that relate to an underlying unifying diagnosis, for example: An in-depth review of the techniques of radionuclide imaging is beyond the scope of this chapter. A brief overview is presented here. • The image often states the agent used and indicates what examination has been performed. • Other nonimaging parameters would carry important information necessary for the interpretation of the case (e.g., renogram curve, “total thyroid uptake,” “split renal function”). • Pay attention to the surface and side markers (e.g., “SSN” in thyroid or parathyroid imaging showing the suprasternal notch). Images with markers are usually acquired over a short time, with low counts and an appearance of noise. Posterior planar views are not “flipped,” and the laterality is reversed to that of conventional radiographic display (e.g., a posterior view of a bone scan; renograms are often imaged with camera head at the patient’s back). Axial SPECT and PET images are displayed as per CT/MRI in this regard. 1. Royal College of Radiologists. Specialty training curriculum for clinical radiology. May 2010. http://www.rcr.ac.uk/content.aspx?PageID=1805 (accessed March 2012) 2. Nuclear medicine and radionuclide imaging, a strategy for provision in the UK: A report of the Intercollegiate Standing Committee on Nuclear Medicine. Jan 2003. http://bookshop.rcplondon.ac.uk/contents/6dbefc58-0f7b-4f16-8341-a307de45e338.pdf (accessed March 2012) 3. Heath Protection Agency. Review of national surveys of population exposure from nuclear medicine examinations in eight European countries. 2008. http://ddmed.eu/_media/background_of_ddm1:dd_report_1_a_.pdf (accessed March 2012) A 76-year-old man presents with back pain. He has previously had a documented left ninth rib fracture, but this is not relevant to the current examination (Fig. 7.1.1). These are whole-body planar images of a bone scan of an adult patient. There is a photopenic area in the L1 vertebral body. No other significant abnormality is present in the rest of the skeleton or soft tissues, apart from a presumed inadvertent subcutaneous injection in the right elbow and the left ninth rib fracture given in the history. The main diagnosis to consider in an elderly patient with back pain and a “cold spot” in the spine is malignancy such as multiple myeloma, plasmacytoma, or a metastatic deposit from either a renal or thyroid cancer. Artefact, avascular necrosis, and osteomyelitis are other considerations. I would review any other imaging studies and recommend further evaluation with MRI of the spine. These are further imaging studies (Figs. 7.1.2–7.1.4). These are dedicated views of the bone scan, plain film, and coronal MR images. The spot views of the bone scan confirm a photopenic area in the left of midline of L1 (Fig. 7.1.2, arrow). The frontal lumbar spine radiograph shows a left-sided lateral wedge deformity of the L1 vertebral body with destruction of the left pedicle (Fig. 7.1.3, arrow), which is replaced by enhancing soft tissues on the coronal MR image (Fig. 7.1.4, arrow), potentially threatening the spinal canal. I would review the rest of the MR images to evaluate for this. The findings would be consistent with my diagnosis of a neoplastic process. The differential diagnosis of a cold spot may include: • These are relatively common—myeloma, renal cell carcinoma, thyroid cancer, chordoma in the spine, Ewing’s sarcoma, and aneurysmal bone cysts. • Coins or keys in trouser pockets (cold spots in the lower pelvis or proximal femur on anterior views) • Pacemaker in the upper chest anteriorly • Belt buckle overlying the lower spine on an anterior view • Joint prosthesis and orthopaedic implant. • Less common, and most often affects the thoracic spine. Brooks ME. The skeletal system. In: Sharp PF, Gemmell HG, Murray AD, eds. Practical Nuclear Medicine. 3rd ed. London: Springer-Verlag;2005:143–161. Sopov V, Liberson A, Gorenberg M, Groshar D. Cold vertebrae on bone scintigraphy. Semin Nucl Med 2001;31(1):82–83 A 50-year-old man presents with melaena and anaemia (Figs. 7.2.1 and 7.2.2). These are images of the abdomen from a radiolabelled red blood cell study, acquired over the first hour and then at 24 hours. There is no abnormal activity in the images over the first hour. On the 24-hour images, there is tracer accumulation in the right abdomen (Fig. 7.2.2, arrows), in an area conforming to the caecum and ascending colon. There is no further abnormal activity elsewhere. The findings are in keeping with a focal area of haemorrhage (bleeding point) proximal to or at the caecum. I would recommend a CT angiogram specifically looking at this to try and identify a cause for the haemorrhage. I would also discuss this with the clinical team in view of the findings, with colonoscopy, a possible useful investigation. • When and where the abnormal activity is first seen? • How the abnormal area “behaves” with time? • Angiodysplasia • Diverticular disease • Tumours • Colitis. The technique of radiolabelled red blood cell study involves labelling the red blood cells of a patient in vitro and subsequently reinjecting these back into the patient’s bloodstream. Normal vascular and blood pool activity is seen in the great vessels, spleen, liver, and kidneys. • The most sensitive modality—it can detect haemorrhage down to a rate of 0.1 mL/min. • Can identify arterial and venous haemorrhage, but cannot differentiate the two. • Imaging over a period of time allows the detection of intermittent haemorrhage. • The procedure is lengthy, not available “out of hours,” and not suitable for acute episodes of brisk haemorrhage. • Does not provide information about the cause of the haemorrhage. Graça BM, Freire PA, Brito JB, Ilharco JM, Carvalheiro VM, Caseiro-Alves F. Gastroenterologic and radiologic approach to obscure gastrointestinal bleeding: how, why, and when? Radiographics 2010;30(1):235–252 Laing CJ, Tobias T, Rosenblum DI, Banker WL, Tseng L, Tamarkin SW. Acute gastrointestinal bleeding: emerging role of multidetector CT angiography and review of current imaging techniques. Radiographics 2007;27(4):1055–1070 A 50-year-old man complains of bilateral ankle pain (Fig. 7.3.1). These are whole-body planar bone scan images of a skeletally mature patient. They show bilateral and symmetrical irregular cortical uptake along the femur and tibia on both sides (Fig. 7.3.1, arrows), where there is an early “double-stripe” appearance near the ankles. The only other abnormality on the remainder of the images is mild lumbar scoliosis with areas of focal uptake compatible with degenerative changes. There is no abnormal extraosseous uptake. The most likely diagnosis is that of hypertrophic osteoarthropathy (HOA). I would like to review any old images and suggest ankle and thoracic radiography if these have not been performed recently. These are the plain X-rays of the ankles (Fig. 7.3.2). These are frontal and lateral radiographs of the left ankle. There is a periosteal reaction seen along the distal tibia and fibula, which confirms the diagnosis of HOA (Fig. 7.3.2, arrow). • Diffuse increased activity in the thorax or hemithorax, pointing to a malignant pleural effusion • Signs of previous thoracotomy, chest wall resection, or sternotomy for lung or breast cancer surgery • “Cold spots” in the kidneys suggestive of renal lesions • Obstructed renal collecting systems from an abdominal or pelvic mass Consider other causes of diffuse cortical hyperostosis: • Venous stasis • Thyroid acropachy • Caffey’s disease • Engelmann’s disease • Hypervitaminosis A Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics 2003;23(2):341–358 A 52-year-old man presents with weight loss, polydipsia, and polyuria (Fig. 7.4.1). These are whole-body planar images of a bone scan showing a “super scan” appearance. The kidneys are not visualised. There is general increased activity in the axial and proximal appendicular skeleton, with random distribution of more focal increased uptake. The findings are those of widespread osteoblastic bony metastases. In a male patient, the primary is likely to be from prostate or lung cancer. In the absence of a known malignancy, I would like to review any previous imaging and recommend further clinical evaluation with a CT chest, abdomen, and pelvis, serum prostate-specific antigen evaluation, and calcium measurement. Commonly implicated malignancies include:
 A bone scan in a teenager with prosthesis or amputation and lung uptake points to treated osteosarcoma with lung metastases.
A bone scan in a teenager with prosthesis or amputation and lung uptake points to treated osteosarcoma with lung metastases.
 A “standing column” in the ureters with hepatic uptake may suggest a pelvic tumour causing outflow obstruction and liver metastases.
A “standing column” in the ureters with hepatic uptake may suggest a pelvic tumour causing outflow obstruction and liver metastases.
Basic Principles of Radionuclide Imaging
 Radionuclide imaging begins with the administration of a radiolabelled tracer. The tracer contains a radioactive isotope bound to a complex or molecule, which determines its kinetics and distribution in the body, and hence the type of physiological process studied. For instance, technetium 99m when bound to MAG3 is used for a renogram, whereas when it is bound to sestamibi, it can be used for cardiac or parathyroid imaging.
Radionuclide imaging begins with the administration of a radiolabelled tracer. The tracer contains a radioactive isotope bound to a complex or molecule, which determines its kinetics and distribution in the body, and hence the type of physiological process studied. For instance, technetium 99m when bound to MAG3 is used for a renogram, whereas when it is bound to sestamibi, it can be used for cardiac or parathyroid imaging.
 Image acquisition is by positioning the patient under a gamma camera or a PET scanner depending on the radioisotope. The radiation emitted from the radioisotope in the patient is captured and analysed to construct an image.
Image acquisition is by positioning the patient under a gamma camera or a PET scanner depending on the radioisotope. The radiation emitted from the radioisotope in the patient is captured and analysed to construct an image.
 Imaging can be dynamic, with the counts over seconds to minutes collated into “frames” and displayed as a cine sequence (e.g., renogram or gastric emptying study) or displayed as a sequence of summed images (e.g., in gastrointestinal bleeding studies). Alternatively, it may be static, with an accumulation or summation of counts over a longer time to form a single image (e.g., a standard bone scan).
Imaging can be dynamic, with the counts over seconds to minutes collated into “frames” and displayed as a cine sequence (e.g., renogram or gastric emptying study) or displayed as a sequence of summed images (e.g., in gastrointestinal bleeding studies). Alternatively, it may be static, with an accumulation or summation of counts over a longer time to form a single image (e.g., a standard bone scan).
 Images acquired at different time points following tracer administration may give different clinically useful information. For example, a three-phase bone scan with dynamic acquisition at the time of injection, followed by static acquisition at 5 minutes and then at 3 to 4 hours, results in vascular, blood pool, and delayed-phase images, which reflect regional blood flow, blood volume (correlates with tissue oedema), and osteoblastic activity, respectively.
Images acquired at different time points following tracer administration may give different clinically useful information. For example, a three-phase bone scan with dynamic acquisition at the time of injection, followed by static acquisition at 5 minutes and then at 3 to 4 hours, results in vascular, blood pool, and delayed-phase images, which reflect regional blood flow, blood volume (correlates with tissue oedema), and osteoblastic activity, respectively.
 The radiation dose to the patient is related to the activity of the administered tracer. Unlike in CT or fluoroscopy, the duration of image acquisition, volume scanned, and number of views obtained does not alter the patient’s radiation burden.
The radiation dose to the patient is related to the activity of the administered tracer. Unlike in CT or fluoroscopy, the duration of image acquisition, volume scanned, and number of views obtained does not alter the patient’s radiation burden.
Specific Examination Technique for the FRCR 2B
 When presented with a radionuclide examination, begin by establishing the type of study shown. Some of the radionuclide examinations have specific or limited indications (as shown by some of the cases later). Awareness of these often focuses the candidate on the abnormalities.
When presented with a radionuclide examination, begin by establishing the type of study shown. Some of the radionuclide examinations have specific or limited indications (as shown by some of the cases later). Awareness of these often focuses the candidate on the abnormalities.
 From the images, try to work out what has been done. Is it a whole-body study? Has dynamic imaging been done, or are they just static views? Has the patient been imaged at multiple phases? What is the distribution of tracer in the body? It is usually apparent if the study shown is a PET, as supposed to a general radionuclide study. PET imaging results in higher spatial resolution, and hence images appear to be of “higher quality.” FDG is a glucose analogue and has a normal blood pool distribution in the brain, liver, and mediastinum, with variable uptake in the heart and bowel.
From the images, try to work out what has been done. Is it a whole-body study? Has dynamic imaging been done, or are they just static views? Has the patient been imaged at multiple phases? What is the distribution of tracer in the body? It is usually apparent if the study shown is a PET, as supposed to a general radionuclide study. PET imaging results in higher spatial resolution, and hence images appear to be of “higher quality.” FDG is a glucose analogue and has a normal blood pool distribution in the brain, liver, and mediastinum, with variable uptake in the heart and bowel.
 There is a large variation in the way images are displayed across centres. It is important to review the labels on the image carefully:
There is a large variation in the way images are displayed across centres. It is important to review the labels on the image carefully:
 Unless stated on the image, it is sensible to state the type of examination rather than the specific tracer; for example, different centres may use HDP or MDP for bone scans, MAG3 or DTPA for renograms, and krypton or aerosols for ventilation scans, which may have subtly different behaviour not apparent to nonspecialists.
Unless stated on the image, it is sensible to state the type of examination rather than the specific tracer; for example, different centres may use HDP or MDP for bone scans, MAG3 or DTPA for renograms, and krypton or aerosols for ventilation scans, which may have subtly different behaviour not apparent to nonspecialists.
 If the diagnosis is still unsure, suggest reviewing the clinical history or other previous imaging. Examiners may offer hints.
If the diagnosis is still unsure, suggest reviewing the clinical history or other previous imaging. Examiners may offer hints.
 Examination technique for the detection of abnormalities, providing a differential diagnosis, formulation, and management plan, should then follow approaches similar to those of the other radiological systems.
Examination technique for the detection of abnormalities, providing a differential diagnosis, formulation, and management plan, should then follow approaches similar to those of the other radiological systems.
References
7.1 Cold Spot
Clinical History
Ideal Summary
Examination Tips
 “Cold spots” are uncommon findings on bone scans, and are often difficult to identify.
“Cold spots” are uncommon findings on bone scans, and are often difficult to identify.
 Check that all the bones are present and “complete” to identify any cold spot.
Check that all the bones are present and “complete” to identify any cold spot.
 Review uptake by the kidneys. If there is also a photopenic area in the kidneys, a potential unifying diagnosis may be metastatic renal cell carcinoma.
Review uptake by the kidneys. If there is also a photopenic area in the kidneys, a potential unifying diagnosis may be metastatic renal cell carcinoma.
Differential Diagnosis
 Neoplastic/metastatic lesions:
Neoplastic/metastatic lesions:
 Metallic artefact at characteristic sites, for example:
Metallic artefact at characteristic sites, for example:
 Haemangioma:
Haemangioma:
 Avascular necrosis
Avascular necrosis
 Osteomyelitis, especially in children
Osteomyelitis, especially in children
Notes
 The traditional bone scan agent (e.g., technetium 99m MDP or HDP) equilibrates with the extravascular space and eventually binds to hydroxyapatite in bones, with excess excreted in the urine.
The traditional bone scan agent (e.g., technetium 99m MDP or HDP) equilibrates with the extravascular space and eventually binds to hydroxyapatite in bones, with excess excreted in the urine.
 Uptake depends on regional blood flow, tissue extraction, and the balance between osteoclastic and osteoblastic activity stimulated by the local pathology.
Uptake depends on regional blood flow, tissue extraction, and the balance between osteoclastic and osteoblastic activity stimulated by the local pathology.
 Predominantly lytic lesions produce photopenic defects, which are difficult to appreciate. Some may incite osteoblastic activity at their leading edge, which improves visualisation.
Predominantly lytic lesions produce photopenic defects, which are difficult to appreciate. Some may incite osteoblastic activity at their leading edge, which improves visualisation.
Bibliography
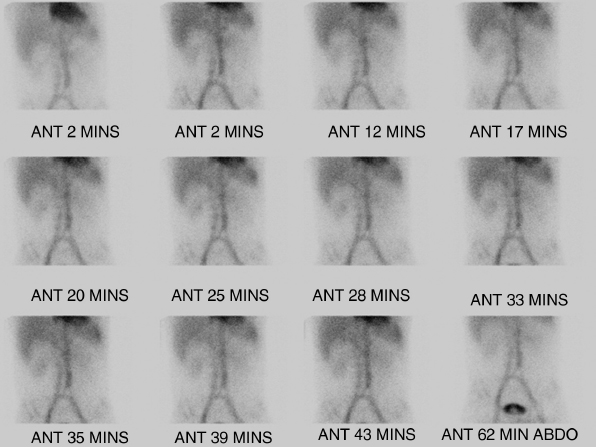
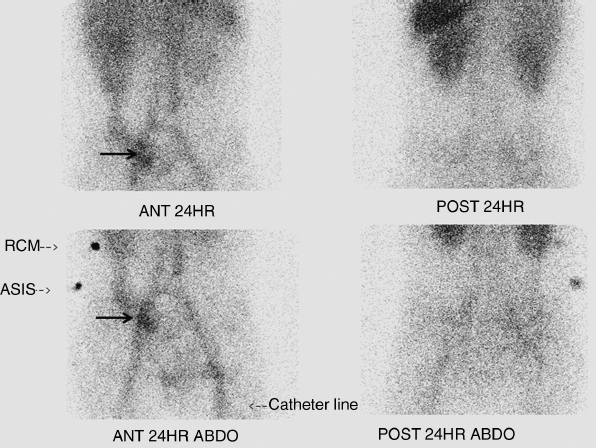
7.2 Gastrointestinal Bleeding
Clinical History
Ideal Summary
Examination Tips
 Intraluminal accumulation of tracer, increasing intensity with time, and movement of the tracer with time in a pattern conforming to the intestinal anatomy are the criteria necessary to identify the site of haemorrhage. Therefore, comment on:
Intraluminal accumulation of tracer, increasing intensity with time, and movement of the tracer with time in a pattern conforming to the intestinal anatomy are the criteria necessary to identify the site of haemorrhage. Therefore, comment on:
 Look carefully for more than one haemorrhage point.
Look carefully for more than one haemorrhage point.
 Subtle abnormality may sometimes be difficult to identify: exact localisation of the site of haemorrhage may be complicated by retrograde transit of extravasated blood within the bowel. If in doubt, offer to review any raw dynamic data in the movie (cine) mode.
Subtle abnormality may sometimes be difficult to identify: exact localisation of the site of haemorrhage may be complicated by retrograde transit of extravasated blood within the bowel. If in doubt, offer to review any raw dynamic data in the movie (cine) mode.
 Delayed images up to 18 to 24 hours may help, as in this case.
Delayed images up to 18 to 24 hours may help, as in this case.
Differential Diagnosis
 Causes of gastrointestinal bleeding from the large bowel include:
Causes of gastrointestinal bleeding from the large bowel include:
 These cannot be distinguished on the basis of the radiolabelled red blood cell study, and would require further imaging or endoscopic evaluation.
These cannot be distinguished on the basis of the radiolabelled red blood cell study, and would require further imaging or endoscopic evaluation.
Notes
 Advantages:
Advantages:
 Disadvantages:
Disadvantages:
Bibliography
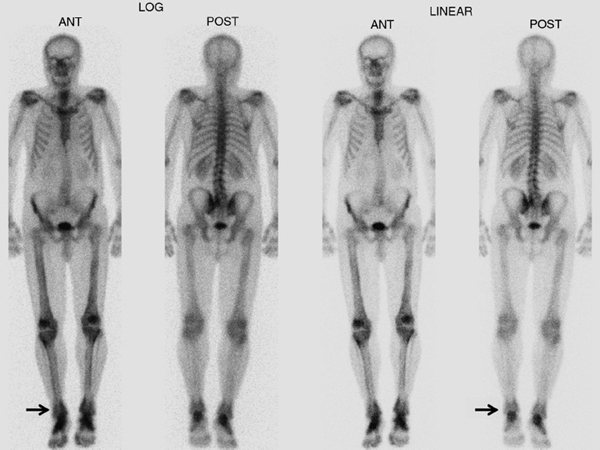
7.3 Hypertrophic Osteoarthropathy
Clinical History
Ideal Summary
Examination Tips
 Look at the long bones and at the periarticular regions for the “double stripe” or “rail track” sign.
Look at the long bones and at the periarticular regions for the “double stripe” or “rail track” sign.
 Look carefully to confirm that the uptake is predominantly at the cortex or periosteum rather than the medullary cavity. If there is abnormal increased uptake in the medullary cavity, consider metastases.
Look carefully to confirm that the uptake is predominantly at the cortex or periosteum rather than the medullary cavity. If there is abnormal increased uptake in the medullary cavity, consider metastases.
 Comment on extraosseous activity. Diagnosis of the underlying disease association is usually not possible from a bone scan. However, possible indicators include:
Comment on extraosseous activity. Diagnosis of the underlying disease association is usually not possible from a bone scan. However, possible indicators include:
Differential Diagnosis
 In adult patients:
In adult patients:
 In younger patients:
In younger patients:
Notes
 Hypertrophic osteoarthropathy is characterised by periostitis and periosteal new bone formation, clinically manifesting with bone and joint pain and digital clubbing. A bone scan is more sensitive in detecting early disease.
Hypertrophic osteoarthropathy is characterised by periostitis and periosteal new bone formation, clinically manifesting with bone and joint pain and digital clubbing. A bone scan is more sensitive in detecting early disease.
 Primary HOA or pachydermoperiostosis is a rare hereditary disease, whereas secondary HOA is much more common.
Primary HOA or pachydermoperiostosis is a rare hereditary disease, whereas secondary HOA is much more common.
 Hypertrophic osteoarthropathy is most commonly associated with bronchogenic carcinoma.
Hypertrophic osteoarthropathy is most commonly associated with bronchogenic carcinoma.
 Other causes of secondary HOA include other benign and malignant intrathoracic tumours, cystic fibrosis, bronchiectasis, lung abscess, Pneumocystis infection, and cyanotic heart disease.
Other causes of secondary HOA include other benign and malignant intrathoracic tumours, cystic fibrosis, bronchiectasis, lung abscess, Pneumocystis infection, and cyanotic heart disease.
 Extrathoracic disease is less often implicated, but includes Hodgkin’s disease, inflammatory bowel disease, cirrhosis, and biliary atresia.
Extrathoracic disease is less often implicated, but includes Hodgkin’s disease, inflammatory bowel disease, cirrhosis, and biliary atresia.
Bibliography
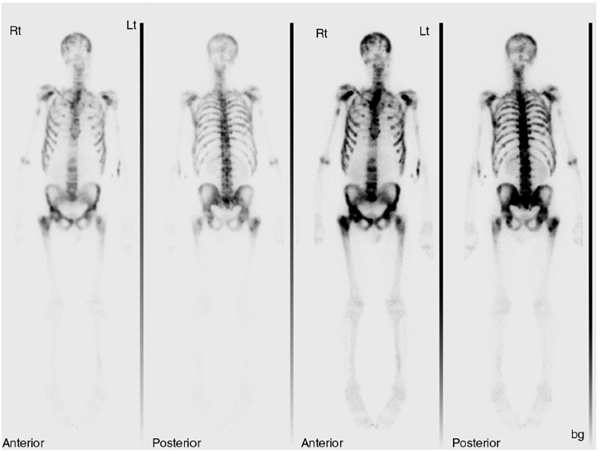
7.4 Malignant “Super Scan”
Clinical History
Ideal Summary
Examination Tips
 Comment on the absence of renal uptake.
Comment on the absence of renal uptake.
 The heterogeneous activity in this case points towards a malignant rather than a metabolic cause of the “super scan.” Metabolic causes are more homogenous on the bone scan.
The heterogeneous activity in this case points towards a malignant rather than a metabolic cause of the “super scan.” Metabolic causes are more homogenous on the bone scan.
Differential Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Planar images may be a “whole-body sweep” or spot views showing a specific anatomical region. Spot views may be done on their own if the clinician is interested in only one particular body part or as additional dedicated views to supplement a whole-body study. Single-photon emission CT (SPECT) and PET imaging captures the radiation emitted from different angles around the patient to reconstruct cross-sectional images, in a fashion similar to CT image formation. The resultant image may be co-registered with CT or MRI scans for enhanced synergistic diagnostic power.
Planar images may be a “whole-body sweep” or spot views showing a specific anatomical region. Spot views may be done on their own if the clinician is interested in only one particular body part or as additional dedicated views to supplement a whole-body study. Single-photon emission CT (SPECT) and PET imaging captures the radiation emitted from different angles around the patient to reconstruct cross-sectional images, in a fashion similar to CT image formation. The resultant image may be co-registered with CT or MRI scans for enhanced synergistic diagnostic power.