CHAPTER 22 Radiopharmaceutical Single Photon Emission Computed Tomography Imaging Agents
* The views expressed in this chapter are those of the author and do not necessarily reflect the official policy or position of the Department of the Navy, Army, Department of Defense, or the U.S. government.
We certify that all individuals who qualify as authors have been listed; each has participated in the conception and design of this work, the analysis of data (when applicable), the writing of the document, and the approval of the submission of this version; that the document represents valid work; that if we used information derived from another source, we obtained all necessary approvals to use it and made appropriate acknowledgments in the document; and that each takes public responsibility for it.
Myocardial perfusion imaging agents have become critical to diagnosis, prognosis, and clinical decision-making in the setting of coronary artery disease. Radiopharmaceuticals have been used to determine regional perfusion since the 1950s, although the imaging techniques have been refined and improved over time. In general, myocardial perfusion radiotracers share many of the following common characteristics:DESCRIPTION OF TECHNICAL REQUIREMENTS
Thallium 201
The Saperstein principle states that a given type of radiopharmaceutical will be distributed in proportion to regional perfusion if its extraction by the organ of interest is high and if its clearance from the blood is rapid.1 This principle led to the development of the potassium analogues, one of the first radiopharmaceuticals used to image myocardial perfusion. These agents are monovalent cations of potassium, cesium, rubidium, and thallium. They enter the myocardium by active channels through the Na+, K+-ATPase pump. Thallium 201 (201Tl) has many of the best physical and biologic characteristics for imaging in humans, making it one of the most popular myocardial perfusion agents used since the 1970s.1 Thallium continues to find significant utility in the diagnosis of coronary artery disease and in the evaluation of prognosis and revascularization in those with ischemic heart disease.
Extraction and Biodistribution
The flow dependence of myocardial tracer uptake limits the sensitivity of a given tracer for the detection of coronary artery disease. In Figure 22-1, the curves of tracer myocardial uptake versus myocardial blood flow flatten as coronary blood flow increases. This implies that at a given level of coronary blood flow, the tracer imaging defect will be much less than the actual coronary blood flow disparity. In Figure 22-1, there is a linear relation of uptake over a wide range of coronary blood flow using a standard of radiolabeled microspheres. At high flow rates (~2.5 mL/min/g), there is a diffusion limitation and a fall in tracer extraction with increased cellular tracer washout, leading to a plateau of myocardial uptake. This phenomenon leads to an underestimation of coronary blood flow at high flow rates and overestimation at very low flow rates when there is increased myocardial extraction relative to blood flow.
In general, 201Tl has an extraction fraction of 87% at normal flow rates. Only viable myocardial cells that maintain a transmembrane potassium gradient will retain 201Tl. In general, a maximum of 4% of the injected dose is taken up in the myocardium (occurring within 10 to 15 minutes of injection), with high concentrations also found in the liver and kidney. 201Tl disappearance from the blood compartment is rapid; more than 90% of blood activity clears with a half-life of 5 minutes, resulting in a decreased blood pool background.2
Redistribution
Myocardial redistribution is one of the most clinically important characteristics of 201Tl. On a practical level, redistribution is manifested as a “filling in” of a myocardial perfusion defect occurring 3 to 5 hours after the injection of 201Tl at peak stress. The myocardial uptake of thallium is not static over time, and redistribution is related to the rate of influx of 201Tl into the myocardium from the blood pool and the rate of clearance or washout of thallium from the myocardium. As described in the previous section, no more than 3% to 5% of tracer is delivered to the myocardium. The amount of washout from the myocardium depends not only on the amount of tracer leaving through blood flow but also on how much is being continuously accumulated by exchange from other compartments.3 Figure 22-2 further illustrates this concept for various levels of myocardial blood flow. All the curves show some level of rapid early myocardial uptake, roughly proportional to myocardial perfusion. Blood levels of tracer fall rapidly as tracer is extracted by the heart and other systemic compartments. After this initial extraction, tracer molecules are slowly released back into the blood from body compartments, maintaining a constant low-level blood concentration of tracer. There is a subsequent exchange of tracer between the blood and myocardial cells until an equilibrium point is reached. This exchange equilibrium is not dependent on blood flow but only on the relative concentration of intravascular and extravascular tracer molecules and the subsequent concentration gradient supported by the membrane potentials or by active membrane transport.4 All tracers must redistribute to some extent, although thallium displays this property to a greater extent because of the ease with which its molecules are transported in and out of the myocardium through active channels. With thallium, a reversible myocardial perfusion defect related to ischemic heart disease will show normalization of 201Tl uptake at 3 to 4 hours after injection at stress because of delayed accumulation into the ischemic segment and a more rapid washout from normal myocardial segments than from hypoperfused segments.1

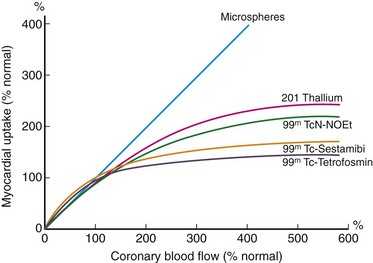
 FIGURE 22-1
FIGURE 22-1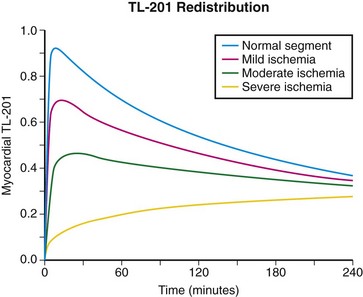
 FIGURE 22-2
FIGURE 22-2

