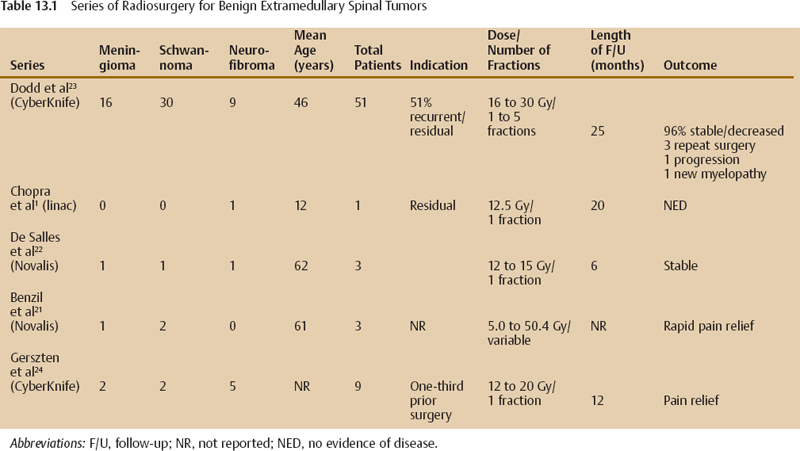
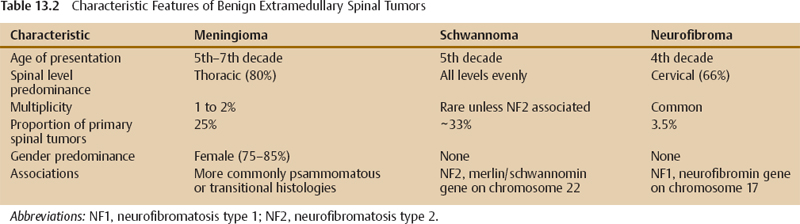
13 Benign extramedullary spinal tumors represent a spectrum of tumors, including meningiomas, schwannomas, and neurofibromas. Although surgery is widely thought to be the treatment of choice for benign extramedullary spinal tumors, small case series support the use of radiation therapy as adjuvant treatment after subtotal resection or for recurrence.1–7 Recently, the delivery of highly conformal radiosurgery of spinal tumors has been made possible by image guidance.8,9 Extrapolating from the effectiveness of radiosurgery for intracranial meningiomas and nerve sheath tumors, where tumor control rates > 90% have been reported, radiosurgery has been explored for benign extramedullary spinal tumors.10–15 Furthermore, the limitations of surgical options for patients with medical comorbidities, recurrent tumors, or familial phakomatoses make radiosurgery an attractive management option. In 2001 Stanford University established the feasibility of image-guided spine radiosurgery for benign tumors when researchers there reported the first clinical experience that included two spinal schwannomas and one spinal menin-gioma.8 Although larger series have reported the efficacy of radiosurgery for metastatic spinal lesions, there is a paucity of reports detailing clinical outcomes of radiosurgery for benign spinal tumors. Evaluation of radiosurgery for these lesions requires longer follow-up to confirm durable safety and efficacy, particularly because, according to surgical reports, recurrences may occur more than 5 years later.8,16–20 Although other commercial radiation systems designed to achieve precision radiosurgery for spinal tumors, such as Synergy (Elekta AB, Stockholm, Sweden) and TomoTherapy (TomoTherapy Inc., Madison, Wisconsin), are in early use, the available data on the clinical outcome of patients with benign extramedullary spinal tumors treated with radiosurgery come from investigators at a small number of institutions using modified linear accelerator (linac) systems, including CyberKnife (Accuray Inc., Sunnyvale, California) and Novalis (BrainLab AG, Feldkirchen, Germany) (Table 13.1).1,21–24 In their brief review of radiation for benign Neurofibromas, Chopra et al reported the results of a 12-year-old child with neurofibromatosis type 1 (NF1) whose tumor was stable at 20 months.1 Collectively, there are only six patients whose outcomes are available after treatment with the Novalis system.21,22 Two other groups report a collective experience of 60 patients treated by CyberKnife. To date, the report by Dodd et al represents the largest single institution series of patients with extended follow-up that may help to ascertain the efficacy of this approach.23 Current clinical indications for benign spine tumors radiosurgery include benign spine tumors located in surgically difficult regions of the spine, recurrent benign spinal tumors after prior surgical resection, and benign spine tumors in patients who have significant medical comorbidities that preclude surgery. Relative contraindications for radiosurgery for benign spine tumors include tumors without well-defined margins, tumors with significant spinal cord compression resulting in acute neurologic symptoms, and tumors that can easily be resected with conventional surgical techniques. Geometrically accurate visualization of the target tumor on imaging is essential for radiosurgery treatment planning. Fortunately, most benign tumors of the spine enhance brightly and have well-defined margins. Magnetic resonance imaging (MRI) is the imaging modality of choice for diagnostic purposes, though issues of spatial distortion need to be considered if MRI is used directly for planning. Because signal intensities of MR images do not reflect a direct relationship with electron densities, unless attenuation coefficients are manually assigned to the regions of interest, spatial distortion limits the accuracy of using MRI directly in radiosurgery planning.25 Because computed tomography (CT) is geometrically accurate, a common solution to improving target visualization is to co-register MRI images with CT images. The currently available commercial radiosurgery systems use CT for treatment planning and delivery. Therefore, the ability to identify tumors on CT together with the probability of generating an adequate image fusion with MRI is key to defining the radiosurgery target. Furthermore, because virtually all extramedullary spinal tumors show some degree of contrast enhancement, postcontrast CT is sometimes used directly to define the target. However, some nerve sheath tumors exhibit heterogeneous enhancement and may be identified by image fusion with MRI. Spinal image fusion of the spine can be much more complex than brain MRI-CT fusion because it is more dependent on the technical aspects of image acquisition. The quality of MR spinal image fusion often requires that the patient’s imaging position closely matches the intended treatment position. By virtue of their origin along the dura and spinal nerve roots, extramedullary spinal tumors can significantly impinge on the spinal cord to cause neurologic symptoms. The goal of radiosurgery is to provide a clinically significant radiation dose to the tumor while observing the dose tolerance to the spinal cord and surrounding soft tissue. The degree of impingement of the tumor on the spinal cord may prevent the generation of a suitable radiosurgery treatment plan. Similar to radiosurgery doses prescribed for intracranial tumors, spine radiosurgery doses generally range from 12 to 20 Gy in a single fraction; doses as high as 30 Gy have been delivered when the treatment was hypofractionated in up to five sessions (Table 13.1). Benzil et al also included patients treated with conventional radiation fraction doses up to 50.4 Gy.21 Meningiomas arise from cells of the meningeal coverings of the central nervous system and occur more frequently within the brain than the spinal cord, with approximately a 5:1 ratio (Table 13.2).26 Spinal meningiomas show a predilection for the thoracic spine and an overwhelming female predominance of 75 to 85%.7,27 Spinal meningiomas, in general, have a more favorable prognosis relative to their intracranial counterparts. In a study of histological and micro-array data of meningiomas, Sayaguès et al determined that spinal meningiomas were most commonly associated with lower proliferative rates and more indolent histologies (psammomatous, transistional variants), and showed characteristic genetic and genomic differences compared with intracranial meningiomas.26 Both histology and age at presentation are important. The Mayo Clinic compared 40 patients under age 50 with spinal meningiomas with a random group of older patients having the same condition and showed that younger patients had higher mortality rates (10%) and recurred more frequently (22% vs 5%) compared with older patients.28 These patients also had a higher number of predisposing risks, such as neurofibromatosis type 2 (NF2), trauma, and radiation exposure. Although radiosurgery for these tumors is an attractive option, longer follow-up will determine the true efficacy. In the Dodd et al series, all of the 15 of 16 meningiomas with radiographic follow-up were controlled, though one patient required surgery and another sustained the only complication reported in the series.23 Clearly, the radiosurgery-treated patients represent a more difficult group to treat, with most being treated after subtotal surgery or recurrence. Still, 70% of the meningiomas treated in this series were symptomatically stable or improved. Figure 13.1 shows the pretreatment sagittal T1-weighted postcontrast MRI (Fig. 13.1A) and the sagittal view of the radiosurgery treatment plan for a 35-year-old man who developed multiple lumbar spinal meningiomas after receiving therapeutic radiation as an adolescent 20 years prior. The CyberKnife radiosurgery treatment plan is shown for the 5.63 cm3 L4 target lesion outlined in red and the prescription isodose reflected in green (Fig. 13.1B
Radiosurgery for Benign Extramedullary Tumors of the Spine
 Technical and Dose Considerations
Technical and Dose Considerations
 Spinal Meningiomas
Spinal Meningiomas
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


