Small melanoma (<6 mm)
Medium/large melanoma (≥6 mm)
Brachytherapy 106 Ru
Eye enucleation
Transpupillary thermotherapy
Cyberknife radiosurgery
Proton beam therapy
Gamma Knife radiosurgery
Brachytherapy 125 iodine
Proton beam, helium ions therapy
All patients need to be evaluated by an ophthalmologist and a specialized radiation oncologist for eligibility of treatment. The following standard outpatient procedure we developed in our centre is recommended:
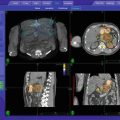
Patients are positioned on the computed tomography (CT) couch and standard retrobulbar anesthesia with goal of complete akinesia of the globe within the orbit is applied. The volume of anesthesia is dependent on the volume of the orbit and is typically between 10 and 15 ml. Suturing of the rectus muscles as described seems not to be needed anymore. A contrast-enhanced CT of the head with 1-mm slice thickness and a 1 mm T2 MRI of the orbit is performed after retrobulbar anesthesia.
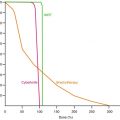
Based on the fused CT and MRI sequences, the target volume is defined by the ophthalmologist and the radiosurgeon, and the treatment plan is generated. In all cases, the tumor is covered completely by the 70 % isodose line. We add a 1 mm margin to the target volume to all directions and 2 mm to the posterior tumor border (Fig. dose plan uvea). This is done to compensate for possible posterior movement of the eye bulb after retrobulbar anesthesia. After the planning procedure, the treatment plan is loaded for treatment delivery. Single-session radiosurgery follows immediately after the plan generation is finalized. Radiation is delivered in a single fraction for all cases using 18–22 Gy to the prescription isodose (70 % in the case of Cyberknife) depending on the size and location of the tumor. After radiosurgery the patient is discharged. Typically there are no significant acute toxicities to be expected. Depending on the size and location of the tumor late side effects can develop several weeks or months after treatment with rubeosis, glaucoma or cataract. A secondary glaucoma is the late toxicity most often encountered. About 25 % of patients will develop a secondary glaucoma 3–60 months (mean 21 months after SRS). These side effects are highly individual and also depend on the individual radiation sensitivity of the patient.
Clinical and imaging follow-up will be performed 3, 6, 12 and 18 months after the treatment using standardized A- and B-scan ultrasound and a 1 mm T2 MRI for evaluation of local control. Tumor control is defined as either continuous regression of the tumor or no further progression.
15.4 Results
We used this method to treat 200 patients with uveal melanoma. The mean follow-up for these patients was 18 months. All patients were treated in one treatment session comprising of retrobulbar anaesthesia, CT and MRI imaging, treatment planning and treatment application within 3 h after start of the anaesthesia. The local control after 1, 2 and 4 years was 97.7, 92.4 and 77.7 %, respectively. Treatment parameters as well as dose to the lens of the affected and contralateral eye and point dose to the optic disc of our first 20 Cyberknife patients are shown in Table 15.2.
Table 15.2
Dose parameters first 20 patients of the Munich series
Patient nr. | Dose | Isodose | Dmax lens affected eye (Gy) | Dmax lens contralateral eye (Gy) | Point dose optic disk affected eye (Gy) |
|---|---|---|---|---|---|
1 | 20 | 75 | 4.8 | 0 | 19.7 |
2 | 18 | 70 | 20.9 | 1.2 | 3.5 |
3 | 20 | 70 | 1.7 | 0.2 | 27.3 |
4 | 20 | 75 | 24.3 | 0 | 18.3 |
5 | 18 | 65 | 20.3 | 0 | 4.7 |
6 | 22 | 70 | 1.7 | 1.7 | 10 |
7 | 19 | 70 | 20.3 | 0 | 6 |
8 | 21 | 70 | 1.2 | 0.3 | 13.1 |
9 | 18 | 60 | 13.8 | 0 | 17.2 |
10 | 17 | 70 | 20.3 | 0.2 | 8.1 |
11 | 19 | 70 | 4.5 | 0.3 | 23.2 |
12 | 18 | 70 | 1.6 | 0.8 | 14.9 |
13 | 18 | 70 | 2.5 | 0.6 | 12.3 |
14 | 18 | 70 | 9.1 | 1.2 | 22.6 |
15 | 20 | 70 | Blind | 0.3 | Blind |
16 | 20 | 70 | 24.5 | 0.4 | 3.3 |
17 | 19 | 70 | 7.8 | 0.4 | 3.7 |
18 | 18 | 70 | 1.9 | 0.6 | 23.4 |
19 | 18 | 70 | 11.3 | 0.2 | 4.3 |
20 | 20 | 70 | 10.1 | 0.6 | 23.6 |
The median maximum apical tumor height according to standardized A-scan ultrasound before treatment was 8 mm (mean 7.9 mm ±2.6 mm) compared to 5 mm (mean 5.4 ±2.1 mm) at the last follow-up examination (p < 0.1) (Figs. 15.1 and 15.2). The visual acuity decreased in most patients over time, typically between 6 and 24 months after radiosurgery. The median reflectivity significantly increased during the follow-up period from 42 to 71 % (p < 0.01). Nineteen patients needed enucleation due to tumor re-growth after radiosurgery (9.5 %). Two patients where successfully retreated by radiosurgery.
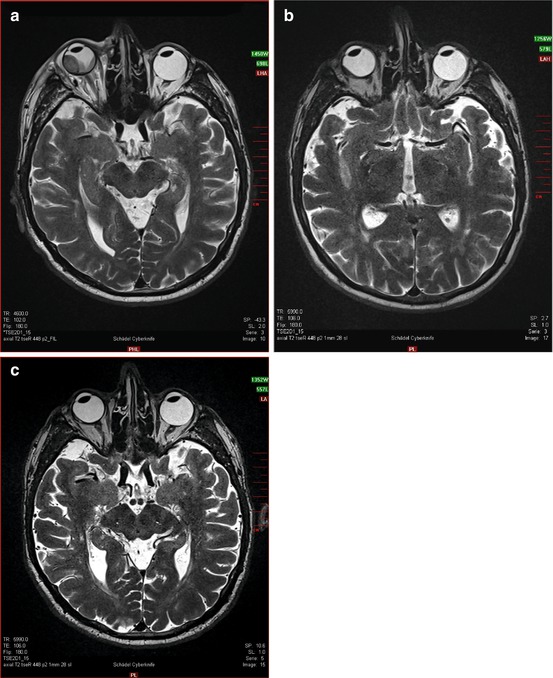
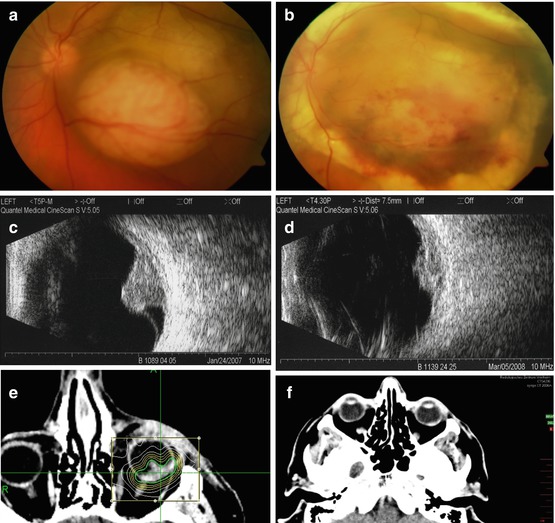
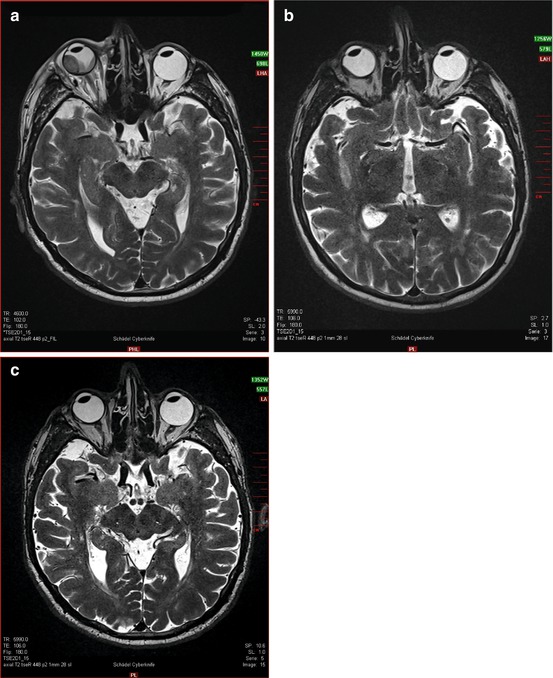
Fig. 15.1
(a) T2 MRI sequence showing large Uveal Melanoma on the temporal right eye with associated retinal detachment. (b) Follow up after 9 months shows significant tumor volume reduction and reversible retinal detachment. (c) Follow up after 18 months displays complete regression of the melanoma
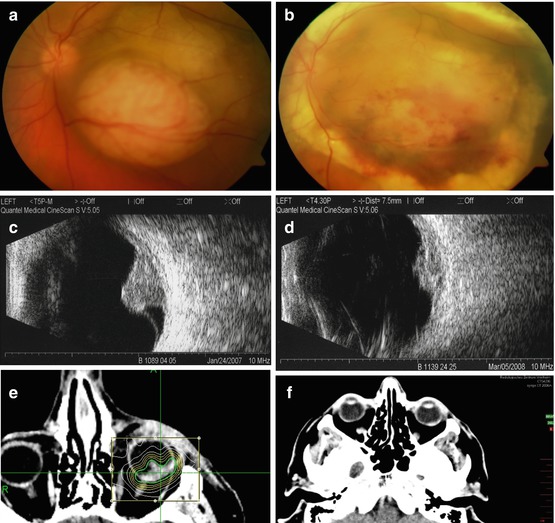
Fig. 15.2




(a, b) Fundoscopy image before (a) and after (b) Cyberknife radiosurgery. (c, d) Ultrasound scan before (c) and after (d) Cyberknife radisurgery. (e) Conformal plan with a steep dose gradient for a typical left-sided uveal melanoma. The isodoses from 10 to 70 % (prescribed isodose, thick line) are shown. The tumor was treated with single-session robotic radiosurgery procedure using a dose of 19 Gy. (f) Treatment result after 18 months. The tumor was significantly reduced in size
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree