Chapter 10 Recognizing the Correct Placement of Lines and Tubes
Critical Care Radiology
 Patients in the critical or intensive care units (ICU) are monitored on a frequent basis with portable chest radiography both to check on the position of their multiple assistive devices and to assess their cardiopulmonary status.
Patients in the critical or intensive care units (ICU) are monitored on a frequent basis with portable chest radiography both to check on the position of their multiple assistive devices and to assess their cardiopulmonary status. In this chapter, you’ll get practical advice for evaluating the successful (or not so successful) insertion and ultimate position of multiple tubes, lines, catheters, and other supportive apparatus used in the ICU.
In this chapter, you’ll get practical advice for evaluating the successful (or not so successful) insertion and ultimate position of multiple tubes, lines, catheters, and other supportive apparatus used in the ICU. Most times, a conventional radiograph is obtained after the insertion or attempted insertion of one of these devices to check on its position and to rule out any unintended complications.
Most times, a conventional radiograph is obtained after the insertion or attempted insertion of one of these devices to check on its position and to rule out any unintended complications.TABLE 10-1 COMMON DISEASES IN CRITICALLY ILL PATIENTS
| Finding or Disease | Discussed in |
|---|---|
| Adult respiratory distress syndrome | Chapter 9 |
| Aspiration | Chapter 7 |
| Atelectasis | Chapter 5 |
| Congestive heart failure (pulmonary edema) | Chapter 9 |
| Pleural effusion | Chapter 6 |
| Pneumomediastinum | Chapter 8 |
| Pneumonia | Chapter 7 |
| Pneumothorax | Chapter 8 |
| Pulmonary thromboembolic disease | Chapter 12 |
Endotracheal and Tracheostomy Tubes
Endotracheal Tubes (ETT)
 Correct placement of an ETT (Box 10-1)
Correct placement of an ETT (Box 10-1)• Endotracheal tubes are usually wide-bore tubes (about 1 cm) with a radioopaque marker stripe and no side holes. The tip is frequently diagonally shaped.
• With the patient’s head in the neutral position (i.e., bottom of mandible is at the level of C5-C6), the tip of ETT should be 3-5 cm from the carina.
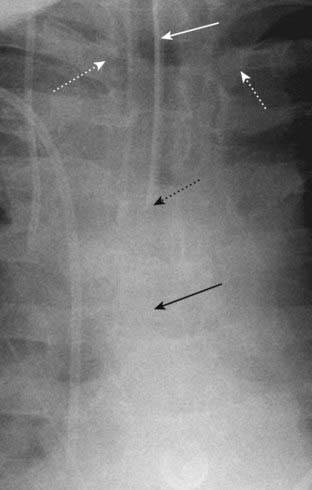
• This is roughly half the distance between the medial ends of clavicles and the carina (Fig. 10-1).
• Ideally the diameter of the ETT should be one half to two thirds the width of the trachea.
• Follow the right or left main bronchus backward until it meets the opposite main bronchus. The carina projects over the T5, T6, or T7 vertebral bodies in 95% of people.
 Incorrect placement and complications of an ETT
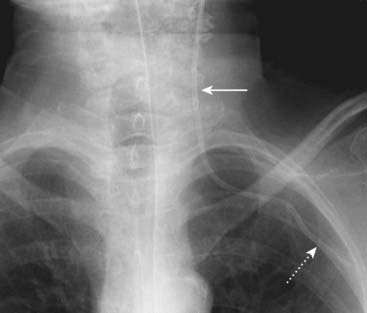
Incorrect placement and complications of an ETT• Most common malposition: because of the shallower angle and wider diameter of the right main bronchus or bronchus intermedius, the tip of the ETT will tend to slide into the right-sided bronchial tree preferentially to the left.
• This can lead to atelectasis (especially of the nonaerated right upper lobe and left lung) (see Fig. 5-13).
Tracheostomy Tubes
 Correct placement of a tracheostomy tube (Box 10-2)
Correct placement of a tracheostomy tube (Box 10-2)• The tip should be about halfway between the stoma in which the tracheostomy tube was inserted and the carina. This is usually around the level of T3 (Fig. 10-4).
• Unlike an ETT, the placement of the tip of a tracheostomy tube is not affected by flexion and extension of the head.
 Incorrect placement and complications of a tracheostomy tube
Incorrect placement and complications of a tracheostomy tube• If the tracheostomy tube is equipped with a cuff, the cuff should generally be inflated to a diameter that fills but does not distend the normal tracheal contour.
Intravascular Catheters
Central Venous Catheters (CVC)
 Why they are used
Why they are used• For venous access to instill chemotherapeutic and hyperosmolar agents not suitable for peripheral venous administration
 Correct placement of CVCs (Box 10-3)
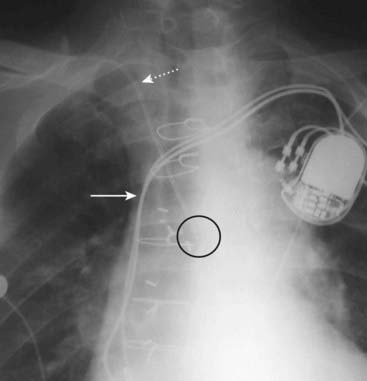
Correct placement of CVCs (Box 10-3)• They are usually inserted either by the subclavian or internal jugular route. The internal jugular veins join the subclavian veins to form the brachiocephalic (innominate) veins, which, in turn, drain into the superior vena cava. The junctions of the subclavian and brachiocephalic veins generally occur posterior to the medial ends of the clavicles.
• A CVC should reach the medial end of clavicle before descending, and its tip should lie medial to the anterior end of the 1st rib.
• The catheter should descend lateral to the spine, and the tip should lie in the superior vena cava (Fig. 10-5).
 Incorrect placement and complications of CVCs
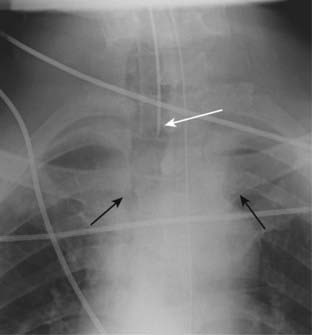
Incorrect placement and complications of CVCs• They are most often malpositioned with their tips in the right atrium or internal jugular vein (if inserted via the subclavian vein) (Fig. 10-6).
• Pneumothorax can occur in up to 5% of CVC insertions, more often with the subclavian approach than the internal jugular route.
• Occasionally CVCs may perforate the vein and lie outside of the blood vessel. Look for sharp bends in the catheter as a clue to a possible perforation.
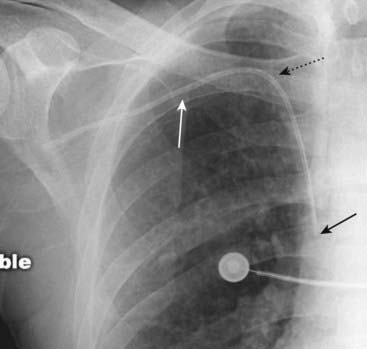
• Sometimes, they may be inadvertently inserted in the subclavian artery rather than the subclavian vein.
• Suspect arterial placement if the flow is pulsatile and the course of the catheter parallels the aortic arch or fails to descend to the right of the spine (Fig. 10-7).




Box 10-3 Central Venous Catheters
Most common malpositions are in the right atrium and internal jugular vein (for subclavian inserted catheters).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree