Chronic Renal Failure and Pretransplantation Assessment
Presentation and Investigation of Renal Failure
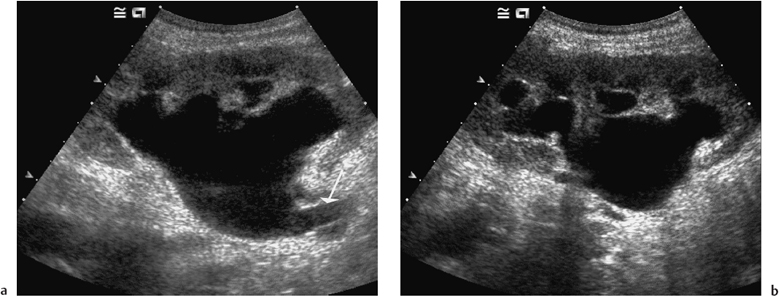
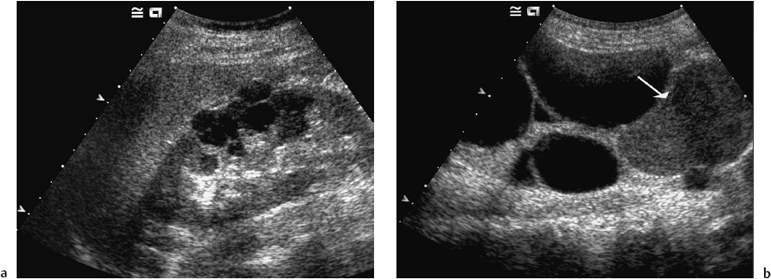
Renal failure is defined as a reduction in the excretion of nitrogenous waste products from the kidney. The measurement of urea and creatinine in a blood sample is a routine investigation carried out in most patients presenting to their doctor with an unknown illness. This is often how underlying renal failure is discovered, and it should be followed by referral to a nephrologist for further assessment. Usually such patients will be seen within a few weeks of referral, but monitoring is advisable during this period to ensure that renal function is not deteriorating further. The cause of the underlying renal disease can often be determined from the patient’s medical history. Physical examination of the urinary tract is usually less rewarding. Thus, the patient who has a creatinine concentration of 200 μmol/l with symptoms of prostatism and an enlarged bladder, or with a family history of polycystic kidney disease and palpable kidneys, who can be referred directly for ultrasound confirmation of the diagnosis is a rare, albeit satisfying case to meet in clinic (Figs. 2.1–2.4). Whilst it is important to exclude obstructive uropathy and polycystic kidneys, most renal diseases lead to loss of renal volume as the kidneys progressively shrink in size due to fibrosis. Cyst formation or acquired cystic disease (Fig. 2.5) is relatively common in patients with long-standing advanced renal failure1, and malignant transformation of such cysts has occasionally been reported.2
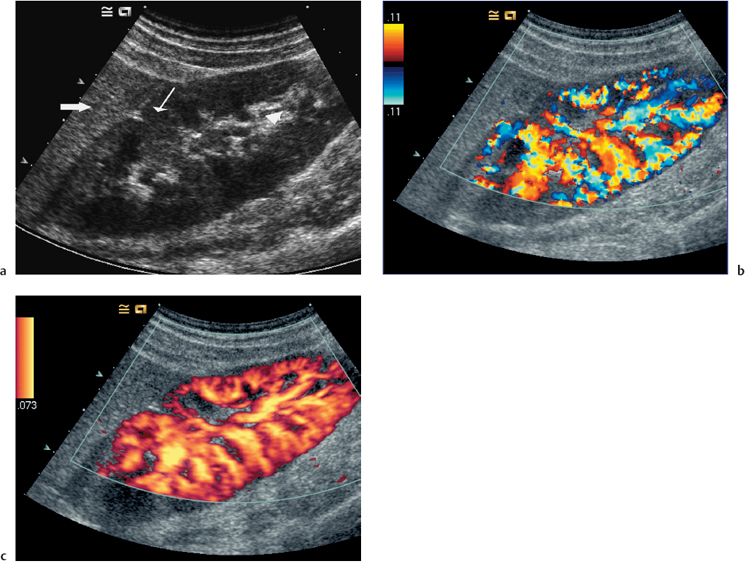
Fig. 2.1 a Scan of a normal right kidney. It is 10.5 cm in length and of normal parenchymal thickness. The renal parenchyma (small arrow) is slightly hypoechoic relative to the liver parenchyma (thick arrow). The renal sinus is bright in comparison with the parenchyma due to its fat content (arrowhead). b Color flow image showing normal intrarenal flow to the cortical margin. c Power Doppler image as in b. There is no directional information using this technique
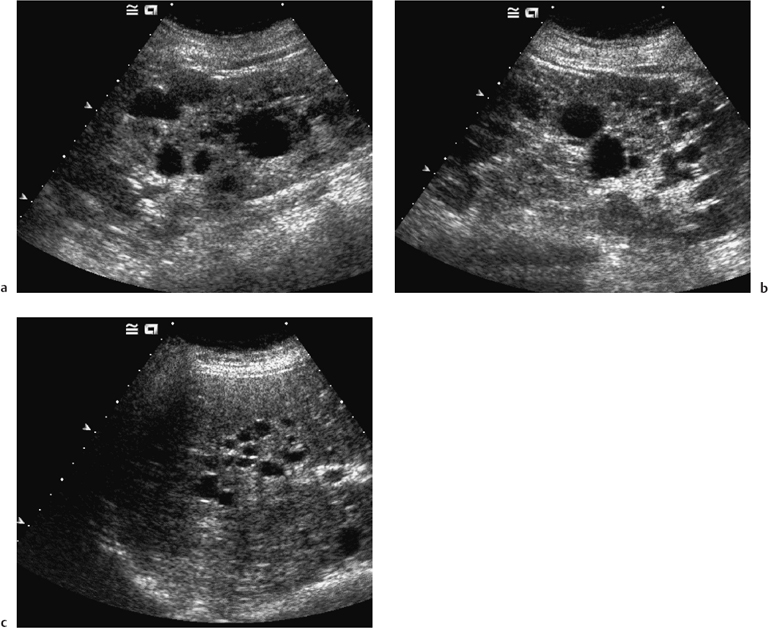
Fig. 2.3 a Right and b left kidneys from a patient with adult polycystic kidney disease (APKD). Both kidneys are markedly enlarged at 15 cm in length; however, both renal outlines are still just discernible. Both kidneys contain cysts of variable size and the above features are pathognomonic of this condition. c A gray-scale image of the liver in the same patient showing multiple small cysts of variable size. The liver may also be affected in this condition, as may the spleen and, rarely, the pancreas
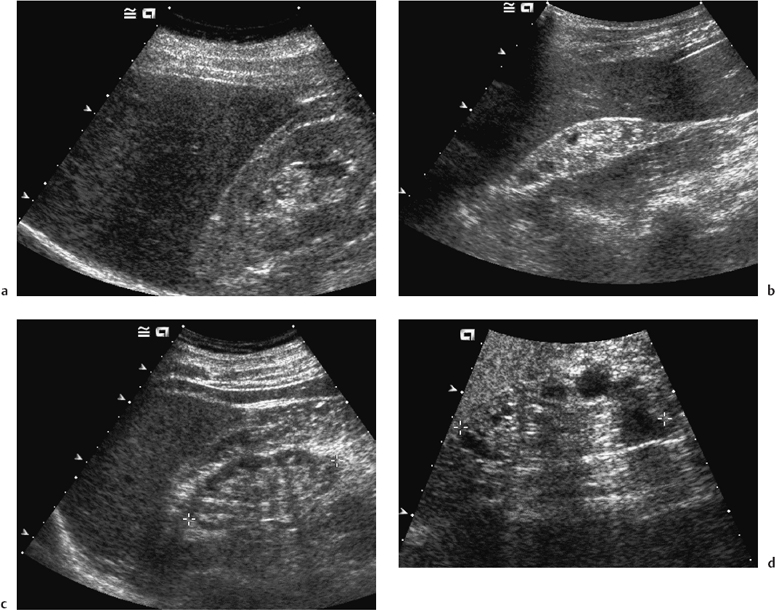
Fig. 2.5 A mixture of kidneys showing the slightly different appearances of small chronically diseased kidneys. All kidneys are below 8 cm in length and have only a very thin rim of tissue remaining. a Small echogenic chronically diseased right kidney (compare with liver). Some parenchymal tissue remains. The left kidney was similar. b An echogenic kidney compared with the liver, with tiny, peripherally situated cysts. Cortical tissue is absent. c A kidney with a similar echogenicity to the liver. No cysts were seen. d Multiple larger, peripherally based cysts are seen in this small chronically diseased kidney
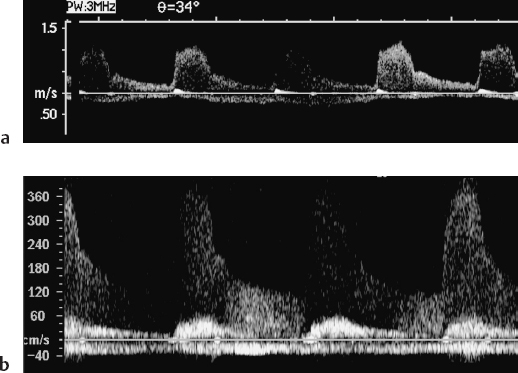
Fig. 2.7 a Normal Doppler waveform from the origin of the right renal artery with a peak systolic velocity of just over 1.0 m/s (normal < 1.8 m/s). b Spectral waveform from the left renal artery with a markedly elevated peak velocity of 3.7 m/s with associated spectral broadening. The appearances are those of renal artery stenosis
Ischemic nephropathy or renovascular disease, either due to a stenosis of the renal artery or to small vessel disease, is increasingly recognized as an important cause of renal failure, particularly in the elderly.3 Such patients often have a history and/or signs of multisystem vascular disease. Where there is proximal renal artery disease, constriction of the postglomerular arte-riole is needed to preserve glomerular filtration, and so the use of angiotensin converting enzyme (ACE) antagonists, which reduce postglomerular arteriolar tone, can precipitate a further deterioration in renal func-tion.4 Other pointers towards renovascular disease as the precipitating cause of renal failure include normal urinalysis results (or minimal proteinuria) and asymmetrically sized kidneys on ultrasonography.
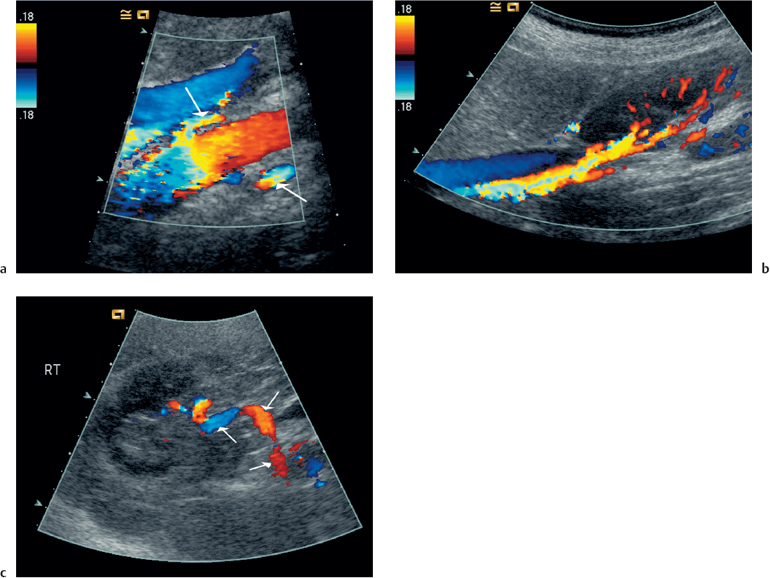
What the best method might be for screening and diagnosis of renovascular disease has been the subject of controversy for many years.5 Whilst Doppler ultra-sonography (Figs. 2.6, 2.7) has the advantage of safety, it is time-consuming and operator-dependent, and it is most likely that magnetic resonance imaging (MRI) techniques will become established as the diagnostic technique of choice in the future. Controversy also surrounds the place of radiological intervention in the treatment of renovascular renal failure, and prospective randomized trials are currently trying to determine whether the advantages of protecting major renal vessels from occlusion with angioplasty and stenting outweigh the side effects of the procedure.6
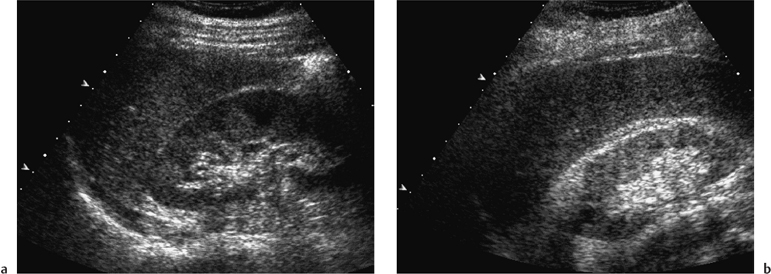
Renal failure in the patient with diabetes most commonly occurs due to microvascular disease, which initially causes glomerular hyperfiltration with microal-buminuria, progressing to frank proteinuria and ultimately glomerulosclerosis. Good diabetic control, treatment of hypertension, and protection against hy-perfiltration injury by ACE inhibitors are the cornerstones of treatment.7 Thus, ultrasound examination of patients with classical diabetic nephropathy often shows normal-sized or enlarged kidneys (Fig. 2.8). Other causes of renal failure in patients with diabetes should be considered, such as coexistent glomerulone-phritis, to which they are more susceptible.8 Ultrasound may be useful in detecting papillary necrosis with obstructive uropathy or renovascular disease if there are asymmetrically sized kidneys.
Chronic pyelonephritis, which is most commonly associated with vesicoureteric reflux, neurogenic bladder, or renal calculi, remains an important cause of renal failure in adults. The place of ultrasound screening alongside isotope renography and micturating cystography to detect reflux in utero or in early childhood is well recognized, and with appropriate surgical treatment and antibiotic prophylaxis progressive renal failure should be preventable.9 Unrecognized cases presenting in adult life are now less common but may be suggested by a history of enuresis or urinary infection in childhood. Ultrasound examination should be an adequate screening test to detect previously undi-agnosed adult cases, which can be confirmed by intravenous urography looking for chronic changes of scarring rather than reflux itself. Renal failure caused by excessive consumption of simple analgesics is also less common. Patients with renal failure associated with the long-term use of nonsteroidal anti-inflammatory drugs are now a much commoner clinical scenario.10
Ultrasound examination should provide adequate screening, especially in the most severe cases, although CT scanning to look for “lumpy, bumpy kidneys” is replacing intravenous urography for confirmatory imaging.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree