Report Turn-Around Time
Jeffrey P. Kanne
LEARNING OBJECTIVES
1. Define report turn-around time and describe its importance in the context of all stakeholders
2. Describe the advantages and disadvantages of voice recognition software in radiology
3. List methods to improve report turn-around time
For many stakeholders, the major work product of a radiology department is the official or final radiology report. Referring health-care providers rely on diagnostic imaging test results to diagnose patients and make treatment decisions,1 and delays in result reporting can lead to dissatisfaction among referring providers and their patients.
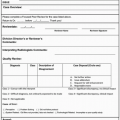
Radiology report turn-around time (TAT) is one metric that is frequently used as marker of radiologist efficiency. The definition of TAT varies and must be viewed in the eyes of the primary stakeholder (Table 4.1). For example, the referring health-care provider may consider TAT as the time from when an order for diagnostic imaging study is placed until the time when results are received. In contrast, the radiologist typically views TAT as the time from when a study is complete and available for interpretation until final signature.
Traditionally, medical transcriptionists typed the dictated report and returned a hardcopy for the radiologist’s signature. Edits were made by hand, and the corrected reports were retyped and then resubmitted for signatures. Signed reports were then delivered, by hand or mail, to referring physicians, who subsequently discussed results with patients in person or by telephone. With the widespread adoption of fax machines in the 1980s, final reports could be delivered more quickly to referring physicians, avoiding the inherent delays in hand delivery and mail. As computer technology evolved, transcribed reports could be entered into computer systems and queued for radiologists to sign electronically. Electronic reports could even be transmitted to some fledgling electronic health records (EHRs).
Table 4.1 DEFINITIONS OF REPORT TURN-AROUND TIME IN THE CONTEXT OF DIFFERENT STAKEHOLDERS. | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Rapid adoption of picture archiving and communication systems (PACS) in the 2000s and improved integration between radiology information systems (RIS) and hospital information systems (HIS) over the past two decades have led to near-universal electronic archiving and transmission of diagnostic imaging studies and their respective reports. Because one of the goals of the EHR is to improve patient safety through effective communication,2 notifications are typically sent to referring health-care providers when imaging or laboratory test results are available so that they can be reviewed and appropriately acted upon. More sophisticated implementations of PACS or EHR include electronic notification applications for critical or urgent results.3
VOICE RECOGNITION TRANSCRIPTION
Voice recognition (VR) software for radiology, first described in 1981,4 also benefited from advancing computer technology and became a core part of the informatics revolution in diagnostic radiology in the 2000s.5 Growth in VR technology was also fueled by increasing demands from patients, referring physicians, and administrators for faster TAT.6
Advantages of VR include decreased radiologist TAT because final reports can be issued immediately following interpretation of the diagnostic examination. In one study performed at a 150-bed community hospital, investigators found a 24-fold decrease in median report TAT following implementation of VR without significant effect on normalized radiologist productivity.7 Other studies have also showed improved report TAT from implementation of VR.8,9,10 At one large urban hospital, implementation of VR not only resulted in decreased radiology report TAT but also increased referring physician satisfaction scores and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores rating patient satisfaction. Furthermore, the practice reduced transcription costs from US$30,000 per month to fewer than US$300 per month.11
The ability to use templates and structured reporting has also been touted as an advantage of VR,12 potentially reducing diagnostic and transcription errors and improving radiologist productivity. Newer software packages allow practices to link specific dictation templates to procedural codes,13 enabling the reporting radiologist to use a standard report format with prepopulated text, the latter of which can be edited to reflect abnormal or additional findings on the examination being interpreted. In one single-institution study investigating the impact of standardized reporting templates, researchers found that the use of prepopulated report templates did not significantly affect dictation time or error rates. Interestingly, the authors did note that radiologists in the study showed a strong preference for using the standardized templates, contradicting previous arguments that standardized reporting goes against the radiologist’s professional autonomy to dictate freely.14
Nevertheless, despite all of the potential advantages of employing VR for diagnostic radiology reporting, some radiologists remain dissatisfied with the technology. One of the major criticisms of VR is real or perceived negative impact on radiologist productivity. Because VR transitions editing tasks from transcriptionist to radiologist, more physician time is spent on tasks other than image interpretation. One study demonstrated a 50% increase in report dictation time despite a 24% decrease in report length.15 Furthermore, the authors also estimated a US$6.10 increase in cost per case using VR as compared with traditional transcription, on the basis of the fact that radiologist time, rather than transcriptionist time, was being used for editing.
Another criticism of VR is high rate of transcription errors in diagnostic radiology reports. One study of two radiologists dictating 100 magnetic resonance imaging (MRI) reports, 50 with VR and 50 with standard transcription, showed that 30% to 42% of the VR reports contained errors in contrast to only 6% to 8% of transcription-generated reports. Furthermore, the authors showed a decline in productivity to 8.6 MRI reports an hour using VR, down from 13.3 MRI reports an hour using transcription.16 Another study showed that 22% of reported imaging studies had potentially confusing transcription errors and, more importantly, that radiologists greatly underestimated the rate of errors in their reports.17 Not only can these errors imply that the radiologist was not paying attention to detail,14 but also the meaning of a report could dramatically change. For example, “There is no pulmonary embolism” could be incorrectly transcribed “There is pulmonary embolism.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree