Reproductive system
Akin, O, Mironov, S, Pandit-Taskar, N, et al. Imaging of uterine cancer. Radiol Clin North Am. 2007; 45(1):167–182.
Barakat, RR, Hricak, H. What do we expect from imaging. Radiol Clin North Am. 2002; 40(3):521–526.
Fütterer, JJ, Heijmink, SW, Spermon, JR. Imaging the male reproductive tract: current trends and future directions. Radiol Clin North Am. 2008; 46(1):133–147.
Hedgire, SS, Pargaonkar, VK, Elmi, A, et al. Male pelvic imaging. Radiol Clin North Am. 2012; 50(6):1015–1226.
Hysterosalpingography
Contrast medium
High osmolar iodinated contrast material (HOCM) or low osmolar iodinated contrast material (LOCM) 270/300 mg I ml–1 10–20 ml.
Equipment
1. Fluoroscopy unit with spot film device
2. Vaginal speculum
3. Vulsellum forceps
4. Hysterosalpingography balloon catheter 5-F to 7-F. In patients with narrow cervix or stenosis of cervical os, Margolin HSG cannula may be used. It has a silicone tip and provides tight occlusion of the cervix for contrast injection.
Patient preparation
1. The patient should abstain from intercourse between booking the appointment and the time of the examination, unless she uses a reliable method of contraception and the appointment is made before day 21, or the examination can be booked between the 4th and 10th days in a patient with a regular 28-day cycle.
2. Apprehensive patients may need premedication.
3. Consent should be obtained.1
Technique
1. The patient lies supine on the table with knees flexed, legs abducted.
2. The vulva can be cleaned with chlorhexidine or saline. A disposable speculum is then placed using sterile jelly and the cervix is exposed.
3. The cervical os is identified using a bright light and the HSG catheter is inserted into the cervical canal. It is usually not necessary to use a Vulsellum forceps to hold the cervix with a forceps, but occasionally this may be necessary. The catheter should be left within the lower cervical canal if cervical incompetence is suspected.
4. Care must be taken to expel all air bubbles from the syringe and cannula, as these would otherwise cause confusion in interpretation. Contrast medium is injected slowly into the uterine cavity under intermittent fluoroscopic observation.
5. Spasm of the uterine cornu may be relieved by intravenous (i.v.) glucagon if there is no tubal spill bilaterally.
N.B. Opiates increase pain by stimulating smooth muscle contraction.
Images
The radiation dose should be kept as low as possible. Intermittent screening should be performed to the minimal requirement. Images should demonstrate:
Aftercare
1. It must be ensured that the patient is in no serious discomfort nor has significant bleeding before she leaves.
2. The patient must be advised that she may have spotting or occasionally bleeding per vagina for 1–2 days and pain which may persist for up to 2 weeks.
3. Prophylactic antibiotics are routinely given in several centres and is good practice.
Complications
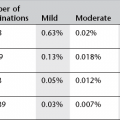
Due to the contrast medium
Allergic phenomena – especially if contrast medium is forced into the circulation.
Due to the technique
1. Pain may occur at the following times:
(a) When using the speculum
(b) During insertion of the cannula or inflation of balloon, some patients may have develop vasovagal syncope – ‘cervical shock’
(c) With tubal distension proximal to a block
(d) With distension of the uterus if there is tubal spasm
(e) With peritoneal irritation during the following day, and up to 2 weeks.
2. Bleeding from trauma to the uterus or cervix
3. Transient nausea, vomiting and headache
4. Intravasation of contrast medium into the venous system of the uterus results in a fine lace-like pattern within the uterine wall. When more extensive, intravasation outlines larger veins. It is of little significance when water-soluble contrast medium is used. Intravasation may be precipitated by: direct trauma to the endometrium, timing of the procedure near to menstruation or curettage, tubal occlusion or congenital abnormalities
5. Infection – which may be delayed. Occurs in up to 2% of patients and is more likely when there is a previous history of pelvic infection.
Ultrasound of the female reproductive system
This can be performed transabdominal (TA) and/or transvaginal (TV).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree