Respiratory system
Computed tomography of the thorax
Indications
1. In the assessment of pulmonary masses, chest wall or pleural disease
2. For the staging and follow-up of malignancy in the chest
3. In the assessment (characterisation, quantification and follow-up) of diffuse lung disease
4. Evaluation of known/suspected thoracic vascular assessment (congenital or acquired – pulmonary embolus, aortic dissection, arteriovenous malformation, etc.)
5. In the assessment of airways disease, bronchiectasis and large airway stenosis.
6. Evaluation for thoracic manifestations of known extrathoracic disease
7. Trauma of the chest
8. Performing CT-guided intervention, e.g. lung, pleura or chest wall mass biopsy, bronchial stent insertion, pleural collection drainage, radiofrequency ablation, etc.
Contraindications
Where i.v. contrast medium is to be administered, the presence of impaired renal function, nephrotoxic drugs, and history of previous reaction to i.v. iodinated contrast media must be evaluated.
Technique
1. Volume scan – usually performed with intravenous contrast enhancement at a rate of 3–5 ml s–1 with a delay of 25–40 s. However, bolus tracking software can be used to trigger the scan more precisely to coincide with optimal contrast enhancement of specific structures, e.g. mediastinum, aorta in suspected aortic dissection or pulmonary artery in suspected pulmonary embolism. (Delayed imaging at 60 s can be useful in cases of large pleural effusion to assess for underlying soft tissue pleural thickening.)
2. High-resolution scan. Non-contrast scan obtained on full inspiration either:
(a) 1 mm slices at 10 to 20 mm intervals or
(b) Volume acquisition through the lungs with reconstruction of contiguous 1 mm slices:
• Spatial resolution should be maximized using the smallest field of view possible.
• Use a high-resolution (high spatial resolution) ‘bone’ algorithm to reconstruct images.
• A volume acquisition with reconstruction of contiguous slices has the benefit of post-processing capabilities, e.g. multiplanar reformatting can help to illustrate the cranio-caudal distribution of lung changes.
• Additional expiratory images can be performed in suspected air-trapping and airways disease.
• Additional prone images are indicated to differentiate reversible-dependent change from early interstitial fibrosis.
Beigelman-Aubry, C, Hill, C, Brillet, P-Y, Grenier, PA. MDCT of the airways: technique and normal results. Radiol Clin North Am. 2009; 47(2):185–201.
Webb, WR, Muller, NL, Naidich, DP. Technical aspects of high-resolution computed tomography of lung disease. In High-Resolution CT of the Lung, 4th ed, Lippincott Williams and Wilkins; 2008:1–41.
Computed tomography-guided lung biopsy
Indications
1. Investigation of a new or progressing pulmonary opacity when other diagnostic techniques such as bronchoscopy have failed to make a diagnosis.
2. Investigation of a new lung/pleural/chest wall lesion in a patient with known malignancy.
3. To obtain material for culture when other techniques have failed to identify the causative organism in a patient with persistent consolidation.
All biopsies should be planned after case discussion at a multi-disciplinary meeting with a respiratory physician, radiologist, surgeon and oncologist where the balance of benefit versus risk can best be assessed. Central lesions are preferably biopsied transbronchially either by standard bronchoscopy (where there is endobronchial disease) or, if extrabronchial, by transbronchial needle aspiration (TBNA) either ‘blind’ or with endoscopic ultrasound guidance (EBUS).
Contraindications
Contraindications are not absolute but should be carefully evaluated by the relevant multi-disciplinary team.
1. Vascular: bleeding diatheses (including conditions that affect platelet function such as chronic renal failure), patient on anticoagulants, significant pulmonary arterial or venous hypertension.
2. Respiratory: contralateral pneumonectomy (unless the lesion is pleurally based and lung tissue will not be traversed), presence of significant emphysema (particularly bullous disease) or significantly impaired respiratory function such that pneumothorax would not be tolerated. (An FEV1 of <1 l or <35% predicted is often used as lower limit cut-off for biopsy.) Air travel should not be undertaken within 6 weeks following the procedure.
3. Suspected hydatid disease.
4. Uncooperative patient (including intractable cough).
Equipment
1. Sampling needle:
• Fine needle aspiration can be performed if there is an on-site cytopathology service. Usually use 20 or 22G needles. Different needles vary by the profile of the needle tip and include Chiba (with a bevelled tip which allows straightforward cytological sample aspiration) and those with modified tips which allow ‘cutting’ to obtain small histological fragments as well as aspiration (suitable for more fibrous lesions), e.g. Franseen® (Cook Medical™) and Westcott® (Becton-Dickinson Medical™).
• Cutting needle biopsy needles are larger gauge (usually 18 or 20G) and obtain a solid core of tissue for histological examination. They usually have adjustable throw of the specimen notch for precise sampling of the lesion. Types include Temno® and Quick-Core® (Cook Medical™). Coaxial needle biopsy systems can be used as these stabilize the cutting needle, allowing resampling without re-puncturing the pleura, aid re-angling of the cutting needle and allow accurate preplanning of depth of passes.
2. Full resuscitation equipment including equipment for pleural aspiration and chest drain insertion.
Staff should be prepared for recognition and treatment of complications of pneumothorax, vasovagal episodes, haemoptysis and (very rarely) air embolus.
Patient preparation
1. Sedative premedication should be avoided if possible as the patient must remain cooperative so that a consistent breathing pattern can be maintained during the procedure.
2. The procedure can routinely be performed on an outpatient basis with observation for 4–6 hours post procedure, but a bed should be available in case of complications. Particularly frail patients, those with frail carers or dependants, or those living alone should be admitted overnight following the procedure.
3. Clotting screen (ideally INR ≤1.4 and platelets > 100 × 109 l–1). There is no clear evidence that aspirin should be discontinued pre-biopsy but consensus suggests clopidogrel should be stopped 5 days prior to procedure.1
4. Pulmonary function tests (spirometry).
Aftercare
1. Close observation post procedure for at least 1 h in a supervised ward or recovery area, with the patient lying in puncture-site-down position (which should be possible for all but anterior approach interventions). (A limited CT at the end of the procedure will have determined if a pneumothorax or parenchymal bleed is present.)
2. Departmental PA chest X-ray at approximately 1–4 h post procedure. If a pneumothorax has developed (or progressed) then the further management will depend on the size of the pneumothorax and clinical condition of the patient. Small pneumothoraces in asymptomatic patients may be observed; larger pneumothoraces in symptomatic patients will require aspiration or chest drain insertion.
3. High-risk and frail patients, particularly those with pre-existing impairment of respiratory function, are best routinely admitted overnight.
Complications2–4
Usually occur early following the procedure:
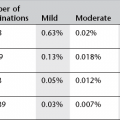
1. Pneumothorax in 20%. However, chest drain insertion is necessary in only a small minority (about 3%). The incidence of pneumothorax is increased if:
• the operator is inexperienced
• a larger gauge needle is used
• there is an increased number of needle passes made
• there is a greater pleura to lesion depth
• smaller lesions are biopsied
• the needle traverses a fissure
• the patient is coughing (precipitated by haemorrhage/haemoptysis).
2. Local pulmonary haemorrhage (10%)
3. Haemoptysis (2–5%)
4. Other complications, such as haemothorax, implantation of malignant cells along the needle track, spread of infection and air embolism, are all extremely rare
5. The current documented death rate is 0.15%.
References
1. Malloy, PC, Grassi, CJ, Kundu, A, et al. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol. 2009; 20(7):240–249.
2. Gohari, A, Haramati, LB. Complications of CT scan-guided lung biopsy: lesion size and depth matter. Chest. 2004; 126(3):666–668.
3. Yeow, K-M, Su, I-HI-Hao, Pan, K-T, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004; 126(3):748–754.
4. Manhire, A, Charig, M, Clelland, C, et al. BTS Guidelines: Guidelines for radiologically guided lung biopsy. Thorax. 2003; 58(11):920–936.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree