Scoliosis is a structural lateral curvature of the spine with a rotatory component. Imaging in scoliosis is important. Most cases of scoliosis are idiopathic, and imaging is used routinely in monitoring the changes of the deformity that take place during growth. Imaging is also crucial in determining the underlying etiology in non-idiopathic cases of scoliosis and is used in pre- and postoperative monitoring.
In the frontal plane, the normal load-bearing spine is straight. Scoliosis is a structural lateral curvature of the spine with a rotatory component. A small deviation (<10°) is sometimes called spinal asymmetry, whereas “true” scoliosis has a deviation of ≥10°. This deviation is accompanied by a rotation that is maximally at the apex of the curve. In the thoracic region, this rotation creates an asymmetry of the thoracic cage that produces the typical chest wall prominence known as the Adams sign.
Imaging in scoliosis is important. Most cases of scoliosis are idiopathic, and imaging is used routinely in monitoring the changes of the deformity that take place during growth. Imaging is also crucial in determining the underlying etiology in non-idiopathic cases of scoliosis and is used in pre- and postoperative monitoring.
Generally, scoliosis is treated by orthopedic surgeons who have special training in spinal and pediatric problems. Patients who have scoliosis may present directly to the radiology department through a primary health care physician or may be referred from the pediatric, neurology, or neurosurgery departments. Many physicians look toward the radiologist as the spinal expert. Therefore, radiologists should know the basics of scoliosis, how to perform the radiologic examination, how to read these films correctly, and how to make a coherent and helpful interpretation.
Classification
Scoliosis can be classified according to etiology, curve location, age at onset, and curve type.
Etiology
Congenital scoliosis
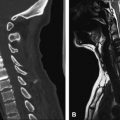
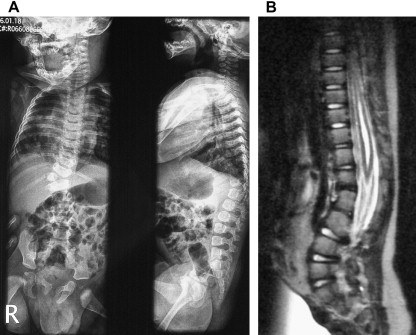
Congenital scoliosis is the most frequent congenital spinal deformity. It is present at birth as the result of embryologic or intrauterine maldevelopment of vertebral elements. The term “congenital” is slightly misleading because it implies that the curvature is apparent at birth, but this is not necessarily so. The vertebral anomalies are present at birth, and the clinical deformity develops with spinal growth and may not become apparent until later childhood . These may be caused by failure of formation or failure of segmentation. They are commonly associated with cardiac or urologic abnormalities that develop during the same period (before 48 days of gestation) ( Fig. 1 ) . Vertebral maldevelopment can be classified as defects of segmentation or defects of formation. Curve progression is strongly related to the type of vertebral abnormality with the poorest prognosis for unilateral unsegmented bars with contralateral hemivertebrae (up to 10°/yr progression), a less severe progression in cases of hemivertebrae or double hemivertebrae (1–2.5° and 2–5°/yr, respectively), and a least severe progression in patients who have block and wedge vertebrae (<1°/yr progression) ( Fig. 2 ). The most common anomaly is hemivertebrae, which is seen in about 40% of cases.


Idiopathic scoliosis
Most frequently, scoliosis is idiopathic (80% of cases). Substantial research efforts have identified several factors contributing to the development of idiopathic scoliosis.
Genetic factors are a potential etiologic component in the development of scoliosis. There is evidence for several different modes of inheritance, including multifactorial, autosomal dominant, and X-linked dominant, with variable phenotypic expression. Several candidate regions have been identified, including on chromosomes 6p, distal 10q, 17p11, 18q, and 19p13 . Family members of affected individuals have an increased incidence of scoliosis. Studies in families with twins have identified 73% to 92% concordance in monozygotic twins and only 36% to 63% concordance in dizygotic twins. The prevalence of scoliosis increases seven times in individuals who have affected siblings and three times in those who have affected parents.
Idiopathic scoliosis is apparently a result of inadequate control of spinal growth. The deformity progresses most rapidly during adolescent growth, and there is evidence that adolescents who have idiopathic scoliosis have an earlier growth spurt , are taller and thinner, and have an increased level of growth hormone.
Vertebral growth anomalies may be related to adolescent idiopathic scoliosis. Differential growth rates between left and right sides of the spine may lead to asymmetry that could be accentuated by the Heuter-Volkmann effect (suppression of growth on the concave side of the curve). When anterior spinal growth outpaces posterior growth in an adolescent patient, hypokyphosis is produced, with subsequent buckling of the vertebral column. Scoliotic spines in girls between 12 and 14 years of age have longer thoracic vertebral bodies, shorter pedicles, and a larger interpedicular distance compared with the spines of normal, aged-matched girls . The differential growth between the anterior and posterior elements is not only significantly different in scoliosis versus normal spines but is also correlated to the severity of scoliosis. This overgrowth in length mainly occurs by enchondral ossification, whereas circumferential growth is slower and happens by membranous ossification.
Scoliosis in generalized diseases and syndromes
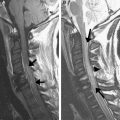
Neural axis abnormalities have a prevalence between 19.5% and 26% among infantile and juvenile scoliosis cases . Several factors have been identified that correlate with a higher incidence in scoliosis, such as equilibrium and vestibular dysfunction, melatonin deficiency, syringomyelia ( Fig. 3 ), Chiari malformation, and spinal tumors. Neuromuscular disorders (eg, cerebral palsy and muscular dystrophy) and some generalized diseases and syndromes (eg, Marfan, neurofibromatosis, rheumatoid disease, or bone dysplasia) are associated with scoliosis. Scoliosis is seen in 8.7% of patients who have Down syndrome .
Traumatic scoliosis
Traumatic scoliosis can be caused by bony lesions (eg, fractures and dislocations) or by soft tissue lesions (eg, burns and postempyema).
Degenerative scoliosis
Degenerative lumbar scoliosis is a lateral deviation of the spine that typically develops after 50 years of age . This is type 1 adult scoliosis, which is primarily degenerative. It is caused most frequently by a disc or facet joint arthritis, affecting those structures asymmetrically. Type 2 adult scoliosis is the progression of adolescent scoliosis in adulthood. Type 3 adult scoliosis is a secondary scoliosis mostly caused by osteoporosis . Although the clinical presentation may vary, degenerative scoliosis is usually associated with loss of lordosis, axial rotation, lateral listhesis, and spondylolisthesis. It is associated with degenerative disk and facet disease and hypertrophy of the ligamenta flava, typically leading to neurogenic claudication and back pain. Rarely, sagittal or coronal imbalance may develop.
Curve location
Curve location is defined by its center, known as the apex, which is the most lateral disc or vertebra of the curve. Usually the apical vertebra is also the most horizontal. Scoliosis can be classified as cervical (apex between C2 and C6), cervicothoracic (C7–T1), thoracic (T2–T11), thoracolumbar (T12–L1), lumbar (L2–L4), or lumbosacral (L5 and below).
Age at onset
Age at onset or diagnosis is used to classify scoliosis as the following types: type 1, infantile (0–3 years); type 2, juvenile (4–10 years, mean age of diagnosis of juvenile scoliosis is around 8 years); type 3, adolescent (11–17 years); and type 4, adult (≥18 years).
Curve types
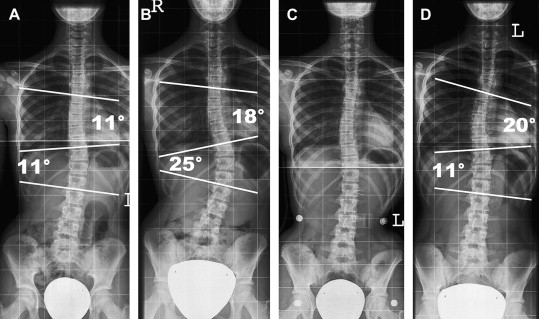
Primary curves are the first to develop. Secondary curves develop as a means to balance the head and trunk over the pelvis, not only in the frontal but also in the sagittal plane. At the time of diagnosis, it is not always possible to differentiate primary curves from secondary curves ( Fig. 4 ). Structural curves (as opposed to nonstructural curves) cannot be corrected with side-bending or traction. Nonstructural curves can be secondary curves or functional curves (postural, secondary to short leg, muscle spasm).
Several classifications according to different curve patterns have been proposed as a preoperative assessment. The use of these classification schemes allows scoliosis practitioners to compare various treatments of similar curve patterns and to recommend selective fusions of the spine when appropriate. The most widely used classification, developed by Moe and reported by King and colleagues (the King-Moe Classification), was designed primarily to help the clinician to decide when to instrument the thoracic curve alone and when to instrument the thoracic and lumbar curves. This classification is not comprehensive, and a more complete and reliable classification was proposed by Lenke and colleagues . The Lenke Classification considers three components: curve type (types 1–6), a lumbar spine modifier (A, B, or C), and a sagittal thoracic modifier (−, N, or +). The six curve types have specific characteristics on frontal and sagittal radiographs that differentiate structural and nonstructural curves in the proximal thoracic (PT), main thoracic (MT), and thoracolumbar/lumbar regions (TL/L). The major curve is the one with the largest Cobb measurement and is included in fusion surgery for idiopathic adolescent scoliosis. The minor curves are all other nonmajor curves. One of the main debates in scoliosis surgery is whether to include those minor curves in the fusion. Thus, six curve types are distinguished in this system based on whether the PT, MT, and TL/L regions are major, minor structural, or nonstructural, including type 1, MT; type 2, double thoracic; type 3, double major; type 4, triple major; Type 5, TL/L; Type 6, TL/L-MT . Many other classification types exist, such as the Scoliosis Research Society Classification for Adult Spinal Deformity, but these usually differ mainly on surgical interpretation points.
Prevalence
The prevalence of scoliosis (≥10°) in the childhood and adolescent population is between 0.5% and 3.0%. Adolescent idiopathic scoliosis is present in 2% to 4% of children between 10 and 16 years of age. Larger curves (>30°) are reported between 0.04% and 0.29%. In childhood scoliosis, 0.5% is reported in the infantile group, 10% in the juvenile group, and the remainder in the adolescent group.
Prevalence
The prevalence of scoliosis (≥10°) in the childhood and adolescent population is between 0.5% and 3.0%. Adolescent idiopathic scoliosis is present in 2% to 4% of children between 10 and 16 years of age. Larger curves (>30°) are reported between 0.04% and 0.29%. In childhood scoliosis, 0.5% is reported in the infantile group, 10% in the juvenile group, and the remainder in the adolescent group.
Clinical features
There is no difference in the prevalence of back pain or mortality between patients who have untreated adolescent idiopathic scoliosis and the general population. Patients who have mild idiopathic scoliosis (<25°) usually have little or no discomfort. Cardiopulmonary complications are almost exclusively seen in early-onset scoliosis (<5 years of age). Patients presenting with severe pain, neurologic symptoms, or rapidly progressing scoliosis require thorough further examination. In adults, degenerative scoliosis may contribute significantly to facet joint degeneration and spinal and foraminal stenosis with subsequent clinical symptomatology.
Infantile idiopathic scoliosis presents as a left thoracic curve in 90% of cases. The male/female ratio is 3:2. In juvenile idiopathic scoliosis, the male/female ratio is 1:2 to 1:4; boys are more affected between 3 and 6 years of age (1:1), and girls are more affected between 6 and 10 years of age (1:8). The number of right and left curves is equal in the younger group (<6 years at presentation), and right curves predominate in the older group (80%).
In North America and Europe, a screening examination in school often leads to a first referral for scoliosis. The goal of school screening programs is to detect childhood scoliosis at a stage where surgical correction can be avoided.
Clinical tests are available to assess scoliosis. The forward-bend test or Adams test is probably the best known. In this test, the patient bends forward with the knees straight and the palms together. During this test, the thoracic and lumbar regions should stay symmetric. An asymmetric rotational hump of 5° to 7° is associated with a scoliosis of 15° to 20°. A referral and imaging is recommended when the angle of trunk rotation is greater than 7°. This is a sensitive, although not a specific, test (2–3% referral).
Natural history
Congenital scoliosis
Congenital scoliosis shows progression in 75% of cases. The poorest prognosis is for thoracic curves and for multiple hemivertebrae and a convex unilateral bar (failure of segmentation) opposite the hemivertebrae. Block and wedge vertebrae show progression <1°/yr, hemivertebrae show a mean progression of 1° to 2.5°/yr, double hemivertebrae increase at a double rate, and unilateral unsegmented bars with contralateral vertebrae may progress up to 10°/yr. The management of congenital scoliosis requires frequent clinical and radiographic follow-up to detect progression. Curve progression or severe vertebral anomalies known to cause curve progression require prompt treatment to prevent deformity and morbidity, such as thoracic insufficiency syndrome .
Infantile idiopathic scoliosis
The vast majority of these curves are self-limiting. The few that progress (usually double structural curves) can be difficult to manage. In cases where the rib vertebral angle difference is larger than 20°, progression is likely. The rib vertebral angle difference is defined as the difference in angulation of the left and right ribs on the apical vertebra as measured on an anteroposterior (AP) radiograph.
Juvenile idiopathic scoliosis
Juvenile idiopathic scoliosis is often progressive (70%). The potential for trunk deformity with cardiac and pulmonary compromise exists especially in scoliosis with onset before 5 years of age. Curves of greater than 30° are almost always progressive, at a rate of 1° to 3°/yr before 10 years of age and at a rate of 4.5° to 11°/yr after 10 years of age. If the scoliosis is in the thoracic region, surgery is required in more than 95% of these cases.
Adolescent idiopathic scoliosis
Roughly 2% of adolescents have a scoliosis (>10°), but only 5% of these have a progression of the curve to greater than 30° ( Fig. 4 ). The progression of scoliosis is dependent on the growth velocity and the magnitude of the curve at the first visit. Progression is most notable with a growth velocity of greater than 2 cm/yr, between 9 and 13 years of age, at bone ages between 9 and 14 years, at Risser signs 0 to 1, and between 0.5 and 2 years before menarche .
The key risk factors for curve progression are the remaining spinal growth (skeletal immaturity) combined with the curve magnitude at a given time and, to a lesser degree, female gender . Skeletal immaturity or remaining skeletal growth is determined by age, menarchal status, and Risser sign (radiologic) or Tanner staging (clinical). The main progression occurs at the time of most rapid skeletal growth. This occurs at 11 to 13 years of age for girls and at 13 to 15 years of age for boys. Determining the peak height velocity (PHV) timing by accurate serial heights measurements is difficult. Usually, patients present without accurate prior height measurements. In these cases, other markers have to be used. The Risser stage is still 0 at the time of PHV, and this phase of accelerated skeletal growth is split into halves by the closure of the triradiate cartilage . Other markers can be used, including digital uncapped phalangeal epiphyses, which are indicative of pre-PHV, and fused epiphyses, which are indicative of post-PHV. Capped but nonfused epiphyses are indeterminant. Tanner stage 1 for breast strongly indicates pre-PHV. Stage 3 for breast and pubic hair occurs at or after the PHV, and stage 4 occurrs after PHV . In the decelerating growth phase, a Risser less than 1 is associated with progression in 60% to 70% of patients, whereas Risser 3 has a risk for progression in less than 10%. Curve pattern has also been identified as an important variable for predicting the probability of progression. Primary thoracic curve scoliosis, especially King types II, III, and V, progress more than primary lumbar curve scoliosis.
Adult idiopathic scoliosis
Curves of less than 30° usually show no progression. Curves measuring 30° to 50° at skeletal maturity progress at an average of 10° to 15° during a normal lifetime. Curves between 50° and 75° show a continuing rate of nearly 1°/yr. In untreated patients, an increased mortality rate due to cardiopulmonary disorders is seen most frequently in scoliosis of greater than 90°.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree