When a child presents with scrotal pain and swelling, the most important determination is between surgical and nonsurgical causes of the symptoms. This often cannot be differentiated with certainty from the physical examination and clinical history. Imaging can, therefore, be crucial to management.
The term acute scrotum refers to sudden-onset scrotal pain, erythema, and/or swelling. The most common causes of acute scrotum are torsion of the spermatic cord, torsion of testicular/epididymal appendages, and epididymitis/epididymo-orchitis. These entities are treated in different ways: surgery for spermatic cord torsion, conservative management for testicular/epididymal appendiceal torsion, and potentially antibiotics for epididymitis. Common causes for the nonacute scrotum include painless scrotal swelling or mass. For nonacute scrotal presentations, imaging can determine the compartment and likely cause of the abnormality, guiding management.
Imaging Techniques
Scrotal ultrasound with Doppler is the first-line imaging technique for evaluating the child with scrotal pain and swelling. It is widely available and inexpensive, offers high sensitivity and specificity, requires no radiation, and is a relatively quick examination, avoiding the need for anesthesia.
In the past, technetium-99m scrotal scintigraphy was used to distinguish ischemia from infection. It was well established and predictable, especially in adults. In practice, it is now rarely used because of longer examination times, decreased availability, radiation exposure, and diminished diagnostic capability in young children, who have small genitalia that are difficult to image.
Advanced imaging with magnetic resonance imaging has limited application, especially acutely, given long examination time and limited availability. It does offer lack of ionizing radiation and occasionally can be helpful as an ancillary study in equivocal cases.
Ultrasound Examination Protocol
The patient should be supine, with a towel between the thighs lifting and supporting the scrotum. A large amount of warm gel is used to minimize pressure on the skin. High-frequency linear-array transducers are recommended (15-8 MHz for neonates; 8-5 MHz in older boys). The asymptomatic side is evaluated first to optimize ultrasound settings and to allow accurate assessment of the symptomatic side. It is also paramount to obtain a midline grayscale and color Doppler image including both testicles, allowing for a side-by-side comparison of the right and left testicular parenchyma, paratesticular tissues, and vascularity, which should be symmetric. In addition, real-time evaluation of the spermatic cord should be performed along its length in the transverse and longitudinal planes.
The testes should be evaluated in at least two planes, with central, medial, and lateral longitudinal images, as well as superior, mid, and inferior transverse images. Each testicle should be measured in three planes, and a volume should also be calculated. Color Doppler images, including spectral Doppler waveforms, allow evaluation of perfusion. Power Doppler can be used to increase sensitivity to blood flow. The epididymides should be evaluated, with the head, body, and tail imaged if possible. Scrotal skin thickness and any palpable abnormality should be directly imaged. Additional maneuvers (Valsalva or upright positioning) can be considered.
What Should I Do If I Cannot Document Flow in the Testicles of a Small Child?
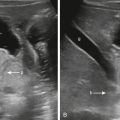
It is often challenging to get flow within the testicles of infants and small children. Often the children are not resting still or comfortably, which causes Doppler artifact. Occasionally the emergency department physicians may need to give medication to make a child more comfortable for the examination to be performed. If initial attempts at documenting vascularity to the testicles are not successful, color Doppler and spectral Doppler waveform analysis can be optimized by using a higher-frequency probe or decreasing color box interrogation dimensions ( Fig. 7.1 ).

Anatomy and Normal Ultrasound Appearance
The scrotum is divided into two halves, each containing a testis, epididymis, and spermatic cord. The testis is surrounded by the tunica albuginea, a strong, fibrous connective tissue layer. A fold of this tunica forms the mediastinum of the testis. The tunica vaginalis covers the tunica albuginea and is composed of an outer parietal and inner visceral layer. A small amount of fluid is normally present within the layers. The epididymis is composed of a head, body, and tail, and it is located at the posterolateral aspect of the testis.
Both testes should have a similar volume and shape on grayscale imaging, with smooth echotexture and medium echogenicity. Blood flow on color Doppler should be symmetric. The testicular mediastinum is seen as hyperechoic linear band along the long axis of the testis ( Fig. 7.2 ). The epididymides should have the same or slightly increased echogenicity as the testes, with a triangular or pyramidal head. The spermatic cords are visualized as slightly hypoechoic tubular structures that course through the inguinal canal ( Fig. 7.3 ).


The ultrasound appearance of the scrotum differs in young children compared with adults. The testicles are slightly more hypoechoic in children, with slight increase in echogenicity as the child approaches puberty. The mediastinum may be less visible. The epididymal body and tail can be difficult to see in young children, with only the epididymal head visible along the upper pole of the testis. Finally, the intratesticular vessels can be difficult to visualize with the use of color Doppler in young children.
Diagnostic Workup
During the imaging workup of scrotal pain and/or swelling, abnormalities can be divided into intratesticular, extratesticular, and nonscrotal ( Table 7.1 ). Intratesticular abnormalities include testicular torsion, trauma, inflammation, masses, and congenital variants. Extratesticular abnormalities include torsion of testicular appendages, epididymitis, epididymal cysts or spermatoceles, hernias, hydroceles, varicoceles, paratesticular masses, and superficial skin lesions. Nonscrotal causative factors for pain include referred pain from renal stones, appendicitis, abdominal or pelvic masses, or neurological issues. These can be considered if the scrotal ultrasound is normal.
| Intratesticular | Extratesticular, Intrascrotal | Nonscrotal |
|---|---|---|
|
Paratesticular mass: rhabdomyosarcoma
|
|
Image Interpretation
When interpreting a scrotal ultrasound, a few critical questions should be posed to guide us to the correct the diagnosis.
Does the Patient Have Pain?
If the answer is yes, then the differential diagnosis for acute scrotum should be considered ( Box 7.1 ).
Although the acute scrotum can be assessed based on scrotal compartment, an alternative diagnostic pathway focuses first on the appearance of the spermatic cord, followed by an assessment of testicular vascularity ( Table 7.2 ). This is to emphasize the importance of spermatic cord assessment in the setting of acute scrotum.
Twisted Spermatic Cord
The sole diagnosis in the setting of a twisted spermatic cord is testicular torsion .
Twisting of the spermatic cord first causes venous and then arterial obstruction. The degree of testicular ischemia is determined by the duration of torsion, as well as the degree of twist, which can range from 180 to 720 degrees.
In the pediatric population, testicular torsion most often occurs in adolescents. Typical presentation in children includes acute-onset scrotal pain, with inguinal and scrotal swelling. One-third of patients will present with nausea and vomiting.
Most cases of testicular torsion arise in patients with an anatomic abnormality known as the “bell-clapper” deformity. Normally, the tunica vaginalis surrounds the anterior and inferior aspect of the testicle. The epididymis and spermatic cord insertion are not covered by the tunica vaginalis, serving as a point of mesenteric fixation. In the bell-clapper deformity, the tunica extends superior to the spermatic cord, enveloping the epididymis and spermatic cord, allowing increased mobility and twisting of the testis within the tunica. Many of these patients with bell-clapper deformities experience recurrent bouts of acute-onset unilateral pain with spontaneous resolution secondary to incomplete or spontaneously resolving torsion ( Box 7.2 ).
Clinical history: recurrent bouts of acute-onset scrotal pain with spontaneous resolution
Spermatic cord abnormality
- ▪
Edematous spermatic cord
- ▪
+/− Whirlpool appearance
- ▪
Testicular vascularity
- ▪
Normal
- ▪
Increased
- ▪
Decreased
- ▪
Scrotal pseudomass located superior to the testicle
Epididymal enlargement and hyperemia
∗Important: Patients with torsion-detorsion sequence can present with imaging findings similar to epididymo-orchitis because of reactive hyperemia. Findings that can distinguish torsion-detorsion from epididymo-orchitis include:
- 1.
Twisted spermatic cord (if present)
- 2.
Pseudomass
- 3.
Resolution of symptoms after detorsion
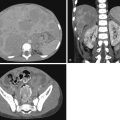
Definitive sonographic evidence of torsion is complete loss of blood flow to the affected testis ( Fig. 7.4A ). However, with partial testicular torsion the cord twists less than 450 degrees with preserved arterial flow, which may be diminished or even normal relative to the contralateral normal side ( Figs. 7.5A and 7.6A ), making this a challenging diagnosis. This underscores the value of real-time spermatic cord assessment. In the setting of complete or partial testicular torsion the spermatic cord can have a target, doughnut, or whirlpool appearance depending on the angle of the transducer relative to the point of the torsion ( Figs. 7.5B–C and 7.6B ). This so-called whirlpool sign is the most sensitive and specific sign for complete and partial testicular torsion. The spermatic cord can also be enlarged and edematous.



Additional imaging features include normal and symmetric volumes and echogenicity in the first 1 to 3 hours of onset of symptoms. Subsequently the testis becomes edematous and hypoechoic, with development of peritesticular hyperemia and edema. There may be an associated hydrocele and scrotal thickening. The affected testis may have an unusual lie, in which the testicle has a transverse configuration in the longitudinal plane ( Fig. 7.4B ) ( Box 7.3 ).
Spermatic cord abnormality
- ▪
Enlargement and edema
- ▪
Target, doughnut, or whirlpool appearance
- ▪
Hypoechoic, hyperechoic, or heterogeneous
- ▪
Asymmetric testicular vascularity
- ▪
Complete loss of blood flow to the affected side
- ▪
Diminished vascularity
- ▪
Testicular size and echogenicity
- ▪
Enlargement
- ▪
Decreased echogenicity
- ▪
Abnormal testicular orientation
Peritesticular hyperemia and edema
Hydrocele
Scrotal skin thickening
In torsion-detorsion sequence or intermittent testicular torsion, testicular blood flow may be decreased, normal, or increased (post-ischemic hyperemia) ( Fig. 7.7A–B ). Additional findings that support the diagnosis of torsion-detorsion include a boggy, edematous spermatic cord and a pseudomass located superior to the testicle ( Fig. 7.7C ). A whirlpool sign or twist of the cord may be present if complete detorsion has not occurred. The epididymis may also be enlarged and hyperemic ( Fig. 7.7C ).