Scrotal Ultrasound
US is the imaging method of first choice for most diseases of the scrotum because of its high accuracy, general availability, and low cost. Indications include acute scrotal pain and scrotal mass [1]. Since most extratesticular masses are benign and most solid intratesticular masses are malignant, making this differentiation is a critical goal and advantage of US imaging.
Imaging Technique
The patient is asked to undress and lie supine on the examination table with his legs together. A folded towel is placed across both legs and beneath the scrotum to support the testes during the examination. The penis is placed on the abdomen and covered with a towel so only the scrotum is exposed. A copious amount of warm gel is placed on the scrotum and examination is performed with a linear array 7.5-10 MHz transducer. Images are obtained of each testis in transverse and longitudinal planes. The epididymides and inguinal canal regions are included in every examination. Color flow imaging and spectral Doppler are used to assess vascularity [2]. At least one image showing both testes on the same image is obtained to compare overall testicular echogenicity (see Fig. 8.16). The use of multiple transmit or focal zones usually improves image quality.
Anatomy
Normal testes are oval globes approximately equal in size with average dimensions of 3-5 cm in length and 2-4 cm in diameter [3]. The echogenicity of the two testes is identical to each other. Normal echogenicity is medium in intensity with a moderately grainy texture (Fig. 8.1). The tunica albuginea is the tough fibrous capsule of the testis, seen as a discrete structure only when a hydrocele is present. The mediastinum (Fig. 8.2) is an infolding of the tunica albuginea that marks the entry and exit portal for the testicular arteries, veins, and ducts. The mediastinum appears as a linear bright echo in the long plane of the testes. Normal vascular clefts are seen as linear hypoechoic bands (Fig. 8.3). Their vascular nature is readily confirmed with color flow US. The epididymis forms at the mediastinum from anastomosis of the efferent ductules [4]. The head of the epididymis (globus major) projects cephalad as a moderately echogenic nodule 10-12 mm in size. The markedly convoluted
tube that makes up the body of the epididymis courses inferiorly along the posterior aspect of the testis to the lower pole where it turns abruptly cephalad and becomes the ductus deferens. The tail of the epididymis (globus minor) is seen as a small nodular structure at this abrupt turn in the course of the epididymal tube. The epididymis appears on US to be coarser and more heterogeneous than the testis. The ductus deferens is markedly convoluted near its origin but straightens into a thick fibrous tube as it courses superiorly to the spermatic cord. The appendix epididymis is a blind-ended efferent tubule sometimes seen as a small tubular or nodular structure near the head of the epididymis. The appendix testis is a Müllerian remnant sometimes seen as another small nodule (1-3 mm size) under the epididymal head. These appendages are isoechoic to the epididymis and are usually seen only when a hydrocele is present. Torsion of these appendages clinically mimics torsion of the testis.
tube that makes up the body of the epididymis courses inferiorly along the posterior aspect of the testis to the lower pole where it turns abruptly cephalad and becomes the ductus deferens. The tail of the epididymis (globus minor) is seen as a small nodular structure at this abrupt turn in the course of the epididymal tube. The epididymis appears on US to be coarser and more heterogeneous than the testis. The ductus deferens is markedly convoluted near its origin but straightens into a thick fibrous tube as it courses superiorly to the spermatic cord. The appendix epididymis is a blind-ended efferent tubule sometimes seen as a small tubular or nodular structure near the head of the epididymis. The appendix testis is a Müllerian remnant sometimes seen as another small nodule (1-3 mm size) under the epididymal head. These appendages are isoechoic to the epididymis and are usually seen only when a hydrocele is present. Torsion of these appendages clinically mimics torsion of the testis.
 Figure 8.1 Normal Testis. The normal testis has a homogeneous, moderately grainy, echotexture. A portion of the mediastinum (arrow) is seen on this transverse image. |
Most of the testis and epididymis is covered by the tunica vaginalis, a membrane identical to peritoneum that lines the scrotal sac. The tunica vaginalis envelops the head of the epididymis and forms a sinus between the body of the epididymis and testes. The fluid of
a hydrocele outlines the epididymal head and fills the epididymal sinus. A “bare area” of the testis is formed posteriorly where the visceral tunica vaginalis reflects to the internal surface of the scrotum isolating the ductus deferens, part of the epididymis and the blood vessels coursing to the mediastinum from the fluid of a hydrocele.
a hydrocele outlines the epididymal head and fills the epididymal sinus. A “bare area” of the testis is formed posteriorly where the visceral tunica vaginalis reflects to the internal surface of the scrotum isolating the ductus deferens, part of the epididymis and the blood vessels coursing to the mediastinum from the fluid of a hydrocele.
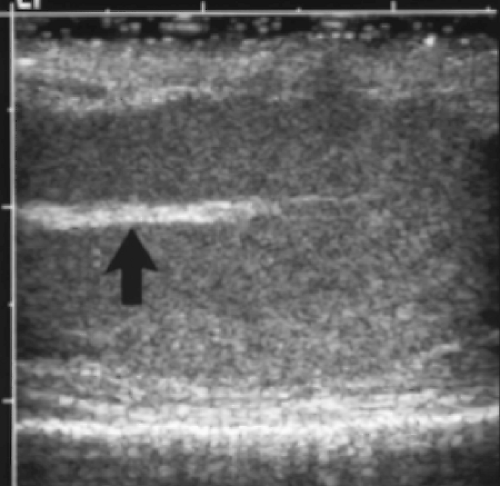 Figure 8.2 Normal Mediastinum Testis. The mediastinal portal (arrow) to the testis is linear and brightly echogenic on this longitudinal image. |
Color flow and spectral Doppler US demonstrate the blood supply of the testis [5, 6]. The spermatic cord is composed of the testicular artery, the cremasteric artery, and the artery of the ductus deferens; the testicular veins that make up the convoluted pampiniform plexus; the ductus deferens (vas deferens); and accompanying lymphatics, nerves, and connective tissue. The testicular artery enters the testes at the mediastinum and arborizes in a subcapsular layer. Redundant branches course through the testes perpendicular to the capsule. The intratesticular arteries normally have a low-resistance spectral waveform with high velocities maintained throughout diastole. The cremasteric and deferential arteries have high-resistance spectral waveforms.
Acute Scrotal Pain
Acute painful swelling of the scrotum is a common indication for scrotal US. Torsion, infection, or trauma may cause acute pain. Real-time gray scale and Doppler US are needed for complete evaluation [2]. All studies compare the symptomatic side to the asymptomatic side. The asymptomatic side is usually scanned first to provide a baseline for comparison with the symptomatic side. In children, testicular torsion is the most common diagnosis, whereas in adults, infection is most common.
Testicular Torsion
Torsion must be identified and treated within a few hours to prevent infarction of the testis. Patients prone to torsion lack the normal attachment of the testis and epididymis to the posterior scrotal wall. This congenital abnormality is called the bell-clapper deformity. The risk of infarction varies with the degree of torsion. Torsion of 90 degrees produces lymphatic and venous obstruction and may not cause infarction for days. Torsion of 720 degrees obstructs arterial flow and may cause infarction within 2 hours.
Swelling of the testis, epididymis, and spermatic cord below the site of torsion is caused by lymphatic and venous obstruction.
Echogenicity is decreased with edema, but is heterogeneously increased with superimposed hemorrhage.
Venous thrombus may be visible in the spermatic cord as enlarged, clot-filled, occluded veins of the pampiniform plexus.
Doppler demonstrates absent or decreased flow in the symptomatic testis compared to the opposite testis (Fig. 8.4) [2, 7].
If flow is present, peak systolic velocity is abnormally low.
With spontaneous detorsion, Doppler findings may be normal or demonstrate reactive hyperemia. The major clue to detorsion is the spontaneous and rapid improvement in pain.
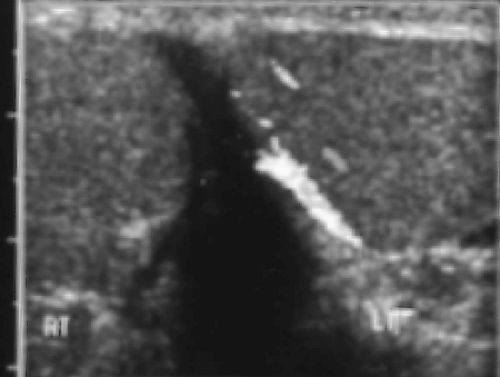 Figure 8.4 Testicular Torsion. Color Doppler image demonstrates normal flow to the left testis (LT) and no flow to the painful right testis (RT) (see Color Figure 8.4). |
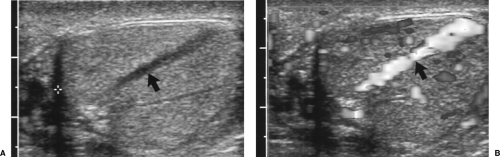
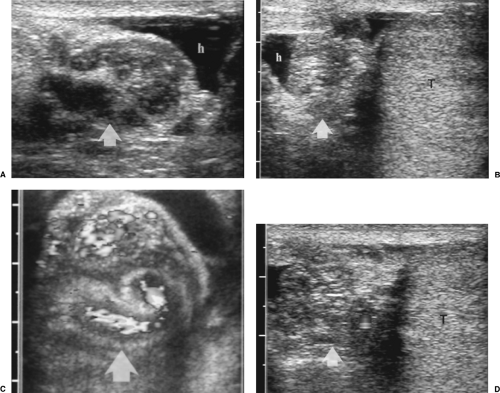 Figure 8.5 Acute Epididymitis. The painful right (A) epididymis (arrow) is enlarged and hypoechoic compared to the asymptomatic left (B) epididymis (arrow). Small hydroceles (h) are present on both sides. Color Doppler images show a marked increase in vascularity in the right (C) epididymis (arrow) compared to the left (D) epididymis (arrow). T, left testis. (See Color Figures 8.5C, D.) |
Acute Epididymo-Orchitis
Infection ascends in orderly fashion from the prostate or urinary tract through the ductus deferens to the epididymal tail, body, head, and finally into the testis. Patients present with pain and swelling at any time in this progression. Adolescents and adults are most commonly affected. Findings include [8, 9]:
Doppler demonstrates asymmetric hypervascularity of the affected epididymis reflecting arterial and venous dilatation (Fig. 8.5C, D). Spectral Doppler shows increased peak systolic and end-diastolic velocities (low-resistance waveform).
Scrotal skin is often thickened.
Testicular swelling, heterogeneous decreased echogenicity, and hypervascularity are signs of coexisting orchitis (Fig. 8.6). To exclude the possibility of testicular tumor masquerading as orchitis, all patients with altered testicular echogenicity should be reexamined when symptoms abate.
Scrotal Abscess
Untreated infection can result in abscess formation in the epididymis, testis, or scrotal wall. These abscesses can rupture into the cavity of the tunica vaginalis and cause pyocele.
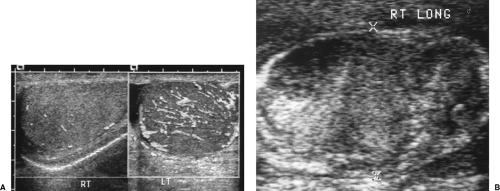 Figure 8.6 Acute Orchitis. A. Color flow images of both testes in a patient with a painful left testis demonstrate marked hypervascularity on the left (LT) compared to the right (RT). B. Severe orchitis in another patient markedly alters the echotexture of the testes (between cursors, x). Differentiation from testicular tumor is difficult (compare to Figure 8.18). Follow-up US examination to ensure complete resolution of orchitis is mandatory (see Color Figure 8.6A). |
Focal areas of complex echogenicity in epididymis (Fig. 8.7) or testis (Fig. 8.8) suggest abscess formation.
Surrounding hyperemia on color flow US indicates inflammation. No flow is seen within the complex fluid of the abscess cavity.
Pyocele appears as echogenic fluid, layering debris, and septations within the cavity of the tunica vaginalis.
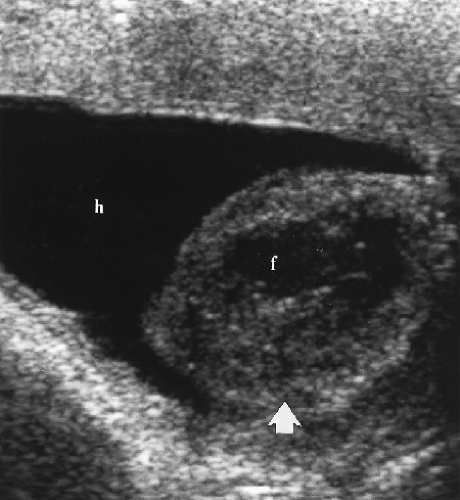
Torsion of Testicular Appendages
Torsion of the appendix testes or appendix epididymis is a common cause of acute scrotal pain in children, mimicking torsion of the testis. In distinction to urgent surgery needed for testicular torsion, torsion of the testicular appendages is self-limited and is treated conservatively with pain management [10, 11].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree