10 Hepatocellular Carcinoma: LI-RADS and OPTN
10.1 Template
Clinical information:
Etiology of cirrhosis: [toxic or metabolic, including EtOH/chronic hepatitis B/congenital hepatic fibrosis
(LI-RADS v2018 does not apply)/vascular (LI-RADS v2018 does not apply)/other: ]
Most recent AFP: [ ] ng/mL [date]
Highest AFP: [ ] ng/mL [date]
Treatment summary:
Targeted ablation:
[date]: [segment], [preablation size] [preablation LI-RADS category]
Local-regional:
[date]: [treatment] [targeted segments or lobes]
Systemic:
[start date] – [end date] [regimen]
Liver:
The liver is [cirrhotic/not cirrhotic]. The background liver parenchyma is [homogeneous/heterogeneous but not nodular/extensively nodular].[Hepatic arterial anatomy.][Portal vein assessment.]
Untreated observations:
Observation #: [1/2/3/4/5]
Location: segment [I/II/III/IVa/IVb/V/VI/VII/VIII/other (describe)]
Size: [ ] × [ ] [mm/cm] (image # [ ], series [ ])
Tumor in vein: [no/yes (describe the involved vessels)]
LR-M features: [none/list all that apply]
Nonrim APHE: [yes/no]
Threshold growth: [yes/no/not applicable]
Nonperipheral washout appearance: [yes/no]
Enhancing capsule appearance: [yes/no]
Ancillary features:
Favoring benignity: [none/list all that apply]
Favoring malignancy: [none/list all that apply]
LI-RADS v2018 category: [LR-NC/LR-1/LR-2/LR-3/LR-4/LR-5/LR-TIV/LR-M]
Treated observations:
Observation #: [1/2/3/4/5]
Location: segment [I/II/III/IVa/IVb/V/VI/VII/VIII/other (describe)] (image # [ ], series [ ])
Treatment modality: [ ]
Treatment date: [ ]
Pretreatment category: [ ]
Pretreatment size: [ ] [mm/cm]
Enhancement in a nodular, masslike, or thick irregular pattern: [yes/no/equivocal]
Size of enhancing component: [ ] [[mm/cm]/N/A]
Enhancement characteristics:
Arterial phase hyperenhancement: [yes/no/equivocal/N/A]
Washout appearance: [yes/no/equivocal/N/A]
Other: [enhancement similar to pretreatment/N/A]
Category: LR-TR [nonviable/equivocal/viable] [size] [mm/cm] (pretreatment [LR1/2/3/4/5/M/TIV/path-proven, [size] [mm/cm])
Remainder of the abdomen:
There is [no] extrahepatic malignancy
10.2 Stakeholders
Liver transplant surgeons and program coordinators, hepatobiliary surgeons, hepatologists, interventional radiologists, diagnostic radiologists, and oncologists.
10.3 Pearls
Hepatocellular carcinoma (HCC) is unique in that high-quality standardized imaging is diagnostic of the disease, usually obviating the need for biopsy. The radiologist’s description of the tumor directly affects patient eligibility for organ transplantation.
Liver Imaging Reporting and Data System (LI-RADS) v2018 applies only in adult patients at high risk for HCC due to cirrhosis, chronic hepatitis B, or current or prior HCC.
LI-RADS v2018 does not apply in patients less than 18 years old, patients of any age with cirrhosis due to congenital hepatic fibrosis, or patients of any age with vascular causes of cirrhosis such as hereditary hemorrhagic telangiectasia, Budd–Chiari syndrome, chronic portal vein occlusion, cardiac congestion, or diffuse nodular regenerative hyperplasia.
Organ Procurement and Transplantation Network (OPTN) classification applies to all liver transplant candidates.
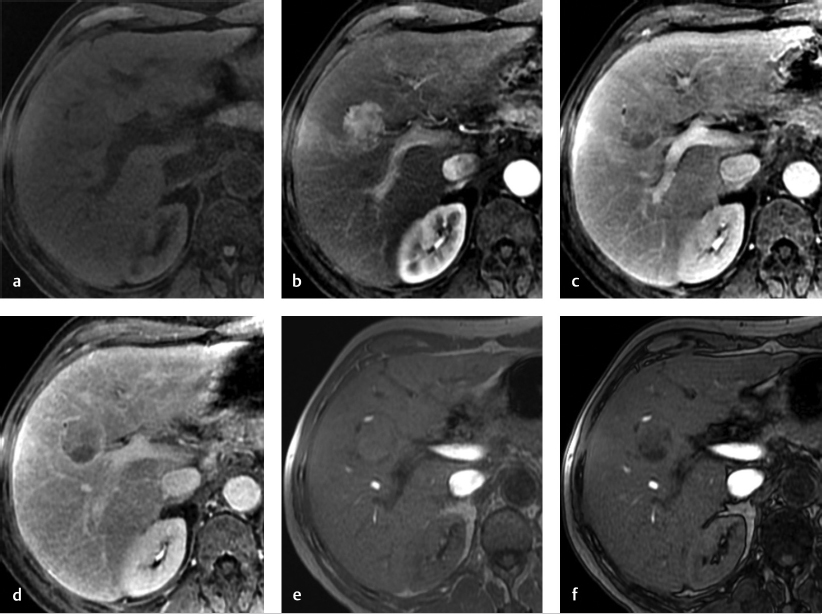
OPTN and LI-RADS criteria for definite HCC (OPTN 5/LR-5) are identical except for 10 to 19 mm observations with nonrim arterial phase hyperenhancement (APHE) and nonperipheral “washout” but no enhancing capsule or threshold growth. Such a lesion is:
Categorized as LR-5 (definite HCC) in computed tomography/magnetic resonance imaging (CT/MRI) LI-RADS v2018.
Does not meet criteria for OPTN class 5.
CT or MRI (▶ Fig. 10.1) scans used for model for end-stage liver disease (MELD) or pediatric end-stage liver disease (PELD) score exception requests must be interpreted by a radiologist at a transplant center.
Report up to five individual observations with the highest LI-RADS categories. In patients with number of observations greater than five, the observations may be reported in aggregate to maintain report clarity.
Assignment of the observation number should remain consistent across all examinations (i.e., observation designated as #1 should be labeled as #1 on all subsequent studies).
Untreated lesion size is the single longest dimension, measured in any plane, including the enhancing “capsule” in the measurement, if present. Avoid size measurement on the arterial phase (AP) and diffusion-weighted imaging (DWI) if the observation is visible on other sequences/phases, due to perilesional enhancement on AP and potential distortion on DWI, which can affect the accuracy of the measurement.
Viable tumor size after treatment should be measured as the longest dimension of the enhancing area of the treated lesion that does not traverse nonenhancing tissue, measured on the late arterial or portal venous phase.
Threshold growth requires CT or MRI examinations performed no more than 6 months apart. If two exams are greater than 6 months apart, then growth of any magnitude is subthreshold. This includes new lesions on the current exam where previously there were none.
Application of the ancillary features (AF) is optional but encouraged. If applied, the LI-RADS category can be upgraded by one if ≥ 1 AF of malignancy is/are present, and downgraded by one if ≥ 1 AF of benignity is/are present. The category should not be adjusted if AFs of both malignancy and benignity are present.
If unsure between two LI-RADS diagnostic categories, choose the category reflecting lower certainty of the diagnosis:
If unsure between LR-1 and LR-2, choose LR-2 because that indicates a lower certainty of benignity.
If unsure between LR-4 and LR-3, choose LR-3 because that indicates a lower certainty of malignancy.
If unsure between LR-5 and LR-M, choose LR-M because that indicates a lower certainty of hepatocellular origin.
Biopsy may be indicated for certain observations, either because of patient history, specific observation characteristics that lead to less confident diagnosis (i.e., LR-4 or LR-M lesions), or physician preference.
If a specific lesion has a known pathology diagnosis, that diagnosis should be provided, and that specific lesion should no longer receive LIRADS categorization. The exception to this rule is whether the pathology reports a hepatocellular lesion known to be a precursor of HCC (e.g., high-grade dysplastic nodule). In such cases, change in imaging characteristics and LIRADS category should be reported as they can signal progression to a frankly malignant lesion (▶ Table 10.1).
LR-1 and LR-2 observations can be reported in aggregate—they need not be individually described. They should be reported in the impression only if they were a suspicious nodule on an antecedent ultrasound or if they are being downgraded from a prior LR-4, LR-5, or LR-M categories, in which case explicit rationale for downgrade should be provided.
LR-3 observations should be reported in the impression if there are no higher category observations, or if they are being downgraded from a prior higher category.
LR-NC (noncategorizable) or LR-TR nonevaluable categories must be reported in the Findings and Impression. The technical reasons for such categorization (e.g., omission of a required imaging phase) should be reported, and a recommendation for further work-up (e.g., repeat imaging with a different modality) should be provided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree