Sedation and monitoring
Sedation
Sedation is the use of a drug or drugs to produce a state of depression of the central nervous system that enables interventional procedures or treatment to be carried out. Sedative drugs may be combined with drugs used for pain relief (analgesia). Sedation is only part of a ‘package’ of care comprising pre-assessment, properly informed consent, adequate facilities, good techniques and risk avoidance.1
Over recent years the number and complexity of diagnostic imaging and image-guided interventional procedures in radiology departments has increased; often these patients are frail, medically unfit, unable to cooperate or lie still. The relief of anxiety, discomfort and pain allows patients to tolerate these procedures. Some drugs, such as benzodiazepines, have purely sedative effects but others, such as opioids, have combined sedative and analgesic effects. Although sedative and analgesic agents are generally safe, catastrophic complications related to their use can occur, often as a result of incorrect drug administration or inadequate patient monitoring.2 The incidence of adverse outcomes is reduced by improved understanding of the pharmacology of drugs used, appropriate monitoring of sedated patients and by recognizing those at increased risk of adverse event.
There is a continuum between the main types of sedation (Fig. 18.1) defined as:
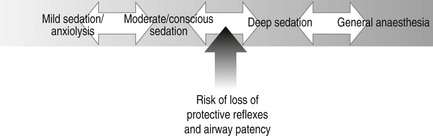
Figure 18.1 The continuum of patient conscious level from mild sedation to general anaesthesia.
1. Anxiolysis: the patient is alert and calm
2. Conscious sedation: a state of depression of the central nervous system that enables diagnostic and therapeutic procedures to be carried out, but during which the patient remains conscious, retains protective reflexes and is able to understand and respond to verbal commands
3. Deep sedation: in which these criteria are not fulfilled and airway or ventilation intervention may be required. Deep sedation requires the presence of an anaesthetist
4. General anaesthesia.
The joint Royal College of Radiologists/Royal College of Anaesthetists Working Party on Sedation and Anaesthesia in Radiology recommended establishment of local guidelines for sedation in radiology.3 These should include:
1. Each patient must have a pre-procedure evaluation to assess their suitability for sedation
2. The operator must not supervise the sedation
3. Nurses and technicians should not administer drugs without medical supervision
4. All staff carrying out sedation should have undertaken training in sedation and resuscitation, and should have knowledge and experience of the sedative drugs, monitoring and resuscitation equipment
5. There should be periodic retraining and assessment of staff
6. There should be an appropriate recovery area
7. Resuscitation equipment and appropriate reversal drugs must be immediately available.
Preparation
Sympathetic patient management with an explanation of the procedure may reduce anxiety and remove the need for any medication. Sedation should be explained and consent obtained. Patients who are to be given intravenous (i.v.) sedation should undergo a period of fasting before the procedure; 6 h fasting for solid food and 2 h for clear liquids.
Resuscitation and monitoring equipment and oxygen delivery devices should be checked and venous access established.
Equipment
1. Appropriate drugs, including reversal agents
Drugs
As part of a sedation protocol the following may be used:
1. Combination of a sedative drug and an analgesic drug (e.g. i.v. midazolam and i.v. opiate). Intravenous analgesic and sedative drugs have a synergistic sedative effect and the dose of each drug must be reduced by up to 70% when administered together. It is best to give the i.v. analgesic first and then titrate the dose of i.v. sedative
2. Analgesic drug alone (e.g. i.v. opiate)
3. Sedative drug alone (e.g. i.v. midazolam).
Analgesic drugs
Analgesic drugs are used for pain control and improve patient comfort. For some procedures local anaesthesia or oral analgesia (using paracetamol 1 g or ibuprofen 400 mg taken 1–2 h before the procedure) will be appropriate. For more invasive interventional radiology procedures the use of intravenous analgesia may be required.
Local anaesthesia
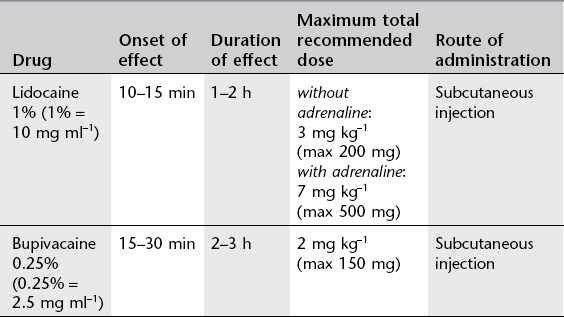
For recommended doses see Table 18.1.
Commonly used local anaesthetics for subcutaneous infiltration are:
1. Lidocaine 1%. Lidocaine may be used in combination with adrenaline (epinephrine) and is supplied in pre-mixed ampoules for this purpose. Adrenaline causes local vasoconstriction, decreases drug absorption and will increase the intensity and duration of action of lidocaine. Lidocaine is also available as a 2% solution.
2. Bupivacaine 0.25%. Has slower onset but longer duration of action than lidocaine. The effect of adrenaline is much less pronounced in combination with bupivacaine. Bupivacaine is also available as a 0.5% solution.
Inhalational analgesia
A mixture of 50% nitrous oxide and 50% oxygen (Entonox®) may be used. This has both analgesic and sedative properties.
Intravenous analgesia
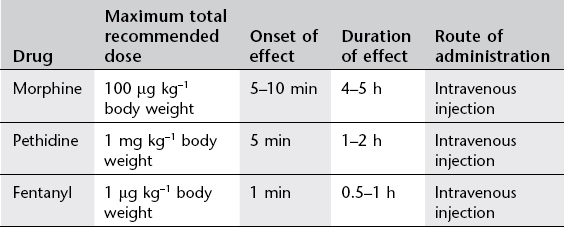
These drugs are used for pain control but also have a dose-dependent sedative effect. Most commonly used are the opioid drugs morphine, pethidine and fentanyl. These drugs must be given in small, divided doses and dose-titrated to the patient’s need. It is extremely important to titrate the dosage to effect rather than assume a fixed dose based on body weight. The maximum recommended dose must not be exceeded because of the risk of adverse events, particularly respiratory depression. For recommended dosage see Table 18.2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree