Neurovascular
Ischemic stroke
Hemorrhage (traumatic or non-traumatic)
Subarachnoid
Intracerebral (hemorrhagic stroke, contusion)
Subdural
Arteriovenous malformation
Cortical vein thrombosis
Dural venous sinus thrombosis
Posterior reversible encephalopathy syndrome (PRES)
Hypoxic ischemic encephalopathy
Infection
Meningitis
Encephalitis
Brain abscess
Ventriculitis
Tumors
Primary brain tumors (especially cortically-based)
Metastases
Autoimmune and inflammatory
Antibody-mediated encephalitis
Acute disseminated encephalomyelitis (ADEM)
Multiple sclerosis
Vasculitis
Other
Primary epilepsy
Seizures post neurosurgical procedures
In patients admitted to ICU with no previous history of neurological disease the majority of seizures are secondary to systemic or metabolic factors associated with critical illness or its treatment. Precipitating factors include hypoxia, hypoglycemia, sepsis, fever, drug toxicity (bronchodilators, antibiotics, antidepressants or antipsychotics), substance abuse (amphetamine, cocaine) or drug withdrawal (alcohol, opioids, benzodiazepines), as well as electrolyte imbalance (such as hyponatremia, hypocalcemia, hypophosphatemia, or acidosis). With few exceptions, these conditions do not have specific imaging appearances and are diagnosed and managed based on history, clinical and biochemical findings. However, neuroimaging may be required to exclude intracranial complications arising de novo, most often of neurovascular origin.
Lastly, prolonged seizure activity causes profound metabolic stress to the brain. That may exacerbate an existing injury, and imaging may be required to assess for consequences such as cerebral edema or encephalopathy.
Imaging Techniques
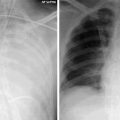
Owing to its speed and availability unenhanced computed tomography (CT) is the mainstay of acute neuroimaging in ICU. The main advantage of unenhanced CT is in the detection of acute hemorrhage, hemorrhagic transformation of an ischemic infarct, or a new intraaxial or extraaxial hemorrhage. Even inexperienced observers readily appreciate a large bleed. Small intracerebral hemorrhages in the posterior fossa and adjacent to the skull may be difficult to detect because of partial volume averaging and beam-hardening artifacts from adjacent bone.
In addition to the detection of hemorrhage, CT allows the assessment of the ventricles and extraaxial fluid spaces, as well as of the effacement of cortical sulci and basal cisterns suggestive of diffuse cerebral edema and increased intracranial pressure. Although non-specific, prominence of extraaxial fluid spaces and ventricles in disproportion to the patient’s age, as well as cerebellar atrophy, may provide clues of possible chronic alcohol abuse as a seizure precipitant. CT allows assessment of vasogenic edema accompanying intracranial lesions, of the degree of exerted mass effect and midline shift or of uncal herniation. The usefulness of CT in the detection of acute cerebral ischemia presenting as subtle hypoattenuation and loss of grey-white matter differentiation is limited and is strongly dependent on the observer’s experience. Established ischemia is easier to appreciate but care should be taken not to misinterpret this as edema if the grey matter is spared. CT can depict advanced global hypoxic ischemic brain injury leading to effacement of cortical sulci and loss of grey-white matter differentiation.
Contrast-enhanced CT may be helpful in the monitoring of intracerebral abscesses, ventriculitis, or intracranial infection. CT angiography is useful in evaluating the patency of intracranial arteries, cerebral ischemia and vasospasm. CT venography has a role to play in the assessment of the patency of the dural venous sinuses.
Due to the practical limitations (see Chap. 4) Magnetic Resonance Imaging of ICU patients is usually reserved for cases in which CT fails to detect the cause of seizures, or if further characterization of abnormal CT findings is needed. The main advantages of MRI stem from its unsurpassed ability to detect changes in brain parenchyma, and to partially categorize them. MRI is more sensitive than CT in the detection of posterior fossa and pituitary abnormalities, as well as pachymeningeal and leptomeningeal enhancement. MR angiography and venography have similar sensitivity to their CT counterparts but are less practical for obvious reasons.
Cortical Vein Thrombosis and Dural Venous Sinus Thrombosis
Cortical vein thrombosis is an uncommon condition presenting with seizures followed by a focal cortical deficit, secondary to cortical venous infarction. The isolated form of this condition (ICVT) is rare, although its frequency is probably underestimated due to the inherent difficulty in establishing the diagnosis. More often, cortical vein thrombosis occurs in combination (CCVT) with superior sagittal sinus thrombosis due to retrograde thrombus propagation and is accompanied by clinical features such as headache, increased intracranial pressure and papilledema. Predisposing factors include hypercoagulable states, head trauma, parameningeal or meningeal infections, pregnancy and the puerperium, dehydration, nephrotic syndrome, and malignancy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree