11 Sentinel Lymph Node Mapping and Dissection The prognosis of mammary carcinoma depends on both local tumor control and adequate adjuvant systemic therapy. Chemo-therapy, hormone therapy, and antibody therapy are used individually and in a targeted way. Selection of the systemic treatment approach depends on the likely effectiveness of different substances (predictive factors, such as estrogen and progesterone receptor status, HER2 status) and on the urgency of therapy (prognostic factors). In clinical practice, the nodal status is the most important prognostic factor, substantially influencing the adjuvant treatment decision. Axillary lymphadenectomy. For many decades, axillary lymph node dissection (ALND) has been an integral component of primary surgical therapy of mammary carcinoma. The objective has been to determine the pathologic nodal (pN) status for designing the adjuvant therapy plan and to secure local tumor control if lymph nodes are positive. ALND therefore represented both a diagnostic and a preventative therapeutic measure. Numerous studies, however, have demonstrated that ALND is associated with high morbidity in the shoulder–arm region and considerably affects the patient’s quality of life (Kuehn et al, 2000; Keramopoulos et al, 1993). Research has therefore focused on how to identify patients with negative nodal status to save them from radical axillary dissection. Imaging procedures. The imaging procedures available for evaluating the nodal status are ultrasound (US), magnetic resonance imaging (MRI), and positron emission tomography (PET). It has not been possible to obtain acceptable diagnostic accuracy for any of these procedures (Fehr et al, 2004; Rajesh et al, 2002; Rieber et al, 2002; Schirrmeister et al, 2001; Yoshimura et al, 1999). Alternative surgical procedures. As an alternative to open axillary dissection, an endoscopic method for ALND was developed some years ago. Lymph nodes were removed through the endoscopic access following liposuction and dilatation of the axilla with CO2 gas. Because of high equipment costs, long surgery times, and comparatively low reduction in morbidity, this procedure did not find its way into routine clinical practice (Kuehn et al, 2001). Lymphatic mapping and sentinel lymph node dissection. Sentinel lymph node dissection (SLND) is based on the orderly lymph drainage of solid tumors (Table 11.1). Accordingly, lymphogenic metastasis first occurs through one or more defined and reproducibly located lymph nodes called sentinel lymph nodes (SLNs) (Fig. 11.1). The pathway of tumor metastasis can be mapped by lymphography. Here, a dye or radioactive substance is injected near the tumor for visualization of lymph drainage. The tracers used are phagocytized by cells in the SLNs, and the SLNs are then detected either visually (dyes), by imaging (lymphoscintigraphy), and/or with a gamma probe (radioactive tracer). If no tumor cells are detected in the SLNs, it may be assumed that the other lymph nodes (nonsentinel lymph nodes [NSLNs]) are tumor-free as well, thus making their removal unnecessary. If the SLNs are histologically positive, it cannot be ruled out that subsequent lymph nodes are also affected; complete axillary lymph node dissection with the removal of 10 lymph nodes from levels I and II is therefore required.
Evaluating the Nodal Status
Term | Definition |
Sentinel lymph node (SLN) | SLNs are the first lymph nodes found in the lymphatic drainage of mammary carcinoma and thus have the highest probability of containing metastases. SLNs are mapped using radioactive tracers and/or dyes (lymphography). All lymph nodes identified by an afferent lymphatic pathway or the uptake of dye, radionuclide, or both tracers are called SLNs. |
Sentinel lymph node dissection (SLND) | SLND is the removal of all lymph nodes that meet the definition of a SLN. Only marked lymph nodes are removed. |
Lymphatic mapping | Lymphatic mapping is the functional imaging of lymphatic drainage from the breast or from a tumor area. |
Nonsentinel lymph node (NSLN) | NSLNs are axillary lymph nodes that do not take up any tracer. |
Fig. 11.1 Axillary and mediastinal lymph nodes. Diagram of axillary and media-stinal lymph nodes showing sentinel nodes and levels I–III.
Clinical Value of Sentinel Lymph Node Dissection
SLND is a targeted means of staging to establish the nodal status in patients with mammary carcinoma. The aim is to reduce the morbidity of the standard procedure (complete ALND), without loss of staging accuracy (Kuehn et al, 2005).
False-negative rate. Numerous validation studies have shown that SLND has a false-negative rate (FNR) of 5 to 29% (Kim et al, 2006; Kuehn et al, 2004). In a meta-analysis by Kim and coworkers covering 69 studies and involving over 8000 patients, a mean sensitivity of 92.6% was found (FNR of 7.4%). When calculating the FNR, the number of false-negative cases does not refer to the entire collective, but only to the number of patients with positive nodal status; hence, the rate of women with incorrectly classified nodal status and thus receiving systemic undertreatment is very low.
Due to considerable interinstitutional variability of the FNR (an FNR of up to 60% was found in individual studies), it is essential to pay close attention to clear and standardized procedural instructions to achieve widely reproducible results at a high level (see below).
Relapse rate. Data on the local relapse rate following SLND are now available from numerous studies on several thousand patients (Palesty et al, 2006; Smidt et al, 2005). They all show that the rate lies far below 1% in patients who develop clinically apparent axillary lymph node (ALN) metastasis after SLND.
Postoperative morbidity. Several randomized studies on postoperative morbidity are available; they clearly document the considerable advantage of SLND as compared with standard axillary dissection (Fleissig et al, 2006; Veronesi et al, 2003).
SLN biopsy has therefore become the standard of care to determine the pN-status in patients with early breast cancer.
Anatomy and Physiology of Lymphatic Drainage of the Breast
The introduction of lymphatic mapping has led to renewed interest in the network of lymph vessels and the functional anatomy of the lymphatic drainage from various regions of the breast. An understanding of the lymphatic system is of utmost importance for choosing the tracer and the injection techniques to be used. Although not all aspects of physiology and pathophysiology of the lymphatic drainage from the breast are fully understood, the current view may be summarized as follows (Romrell and Bland, 1998):
Blind-ended lymph capillaries transport the lymph from the parenchymal tissue of the breast through a system of communicating vessels. There are three main directions of drainage:
 lymph vessels draining directly through the parenchymal tissue to the lymph nodes
lymph vessels draining directly through the parenchymal tissue to the lymph nodes
 lymph vessels draining along the mammary ducts through the subareolar plexus to the axillary lymph nodes
lymph vessels draining along the mammary ducts through the subareolar plexus to the axillary lymph nodes
 lymph nodes draining a deep plexus at the base of the breast and through the transpectoral pathway into the axillary and internal lymph nodes
lymph nodes draining a deep plexus at the base of the breast and through the transpectoral pathway into the axillary and internal lymph nodes
Mapping and imaging of the lymphatic flow by means of tracers has greatly extended our knowledge on the lymphatic drainage of the breast. Currently, the following ideas greatly influence the tracer injection techniques used for SLND.
The entire breast and the overlying skin drain into one or more axillary SLNs. Only regions near the thoracic wall may have additional drainage through the mediastinal lymph node chain. Dermal, subdermal, and periareolar injection can only map the axillary SLNs; deep injection near the tumor or into the tumor also maps the mediastinal SLNs in up to 29% of cases (Borgstein et al, 2000; Nathanson et al, 2001; Roumen et al, 1999; Tanis et al, 2001). Hence, the question of mediastinal lymph drainage depends less on the quadrant than on the proximity of a tumor to the thoracic wall.
Sentinel Lymph Node Mapping
SLNs are mapped by using either dyes or radioactive tracers. The use of radionuclides has been established in clinical practice as a standard procedure because of higher detection rates, better reproducibility, and less tissue trauma. The dye method is considered as an optional supplement to make it easier for the surgeon to find the SLN under image guidance.
Dye Method
In Germany, patent blue V (Guerbet Laboratories, Birmingham, UK) is usually used for SLN dye mapping. Immediately before surgery (following skin disinfection and sterile coverage), approx. 3 mL of a diluted solution (1: 1 with physiological saline) are injected near the tumor (Fig. 11.2a). It is important to ensure that skin tattooing is avoided (no injection near the skin, avoidance of multiple injections, withdrawal of the syringe plunger when retracting the needle). The axillary incision should be performed 5 minutes after injection of the dye and not before. However, this time interval should not exceed 15 minutes because if the intervals are too long the rate of detection is reduced (Kuehn et al, 1999) (Fig. 11.2b,c).
Fig. 11.2a–c Dye method. Injection of dye in the periphery of the tumor (a). Exposed sentinel lymph node, dye-stained (b, c).
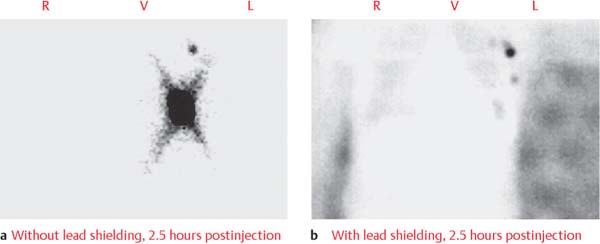
Fig. 11.3a,b Lymphoscintigraphy. Tracer injected in the periphery of the tumor, nuclear medicine imaging of axillary tumor site; (a) without lead shielding, 2.5 hours postinjection, (b) with lead shielding, 2.5 hours postinjection.
Lymphoscintigraphy
Lymphoscintigraphic mapping still is the standard procedure for imaging the SLNs (Fig. 11.3). The mapping may be performed using a 1-day or 2-day protocol.
Radiotracer and activity. The radiopharmaceuticals used are 99 mTc-labeled colloids with a particle size of 20–100 nm. Based on the current understanding of lymphatic drainage from the breast (see above), the injection is performed in such a way that SLN removal is as little hampered by blooming artifacts as possible. Periareolar intradermal injection of small volumes (0.1–0.2 mL) of radiotracer is therefore increasingly used.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree