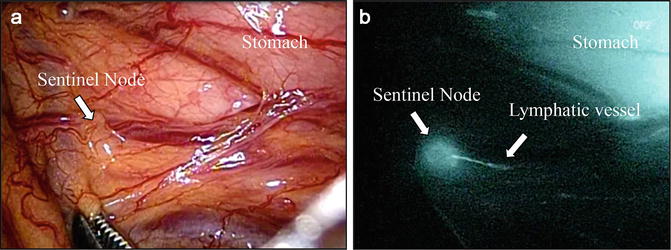
Fig. 24.1
Double tracers are recommended for SN detection of early gastric cancer. Navigator GPS is very useful for detection of SNs with RI
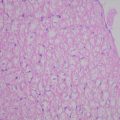
We examined the value of SN navigation surgery, including estimation of nodal micrometastasis, in early gastric cancer patients [4]. The day before surgery, approximately 3 mCi 99mTc-radiolabeled tin colloid (Nihon Medi-Physics, Nishinomiya, Japan) was injected endoscopically into the gastric submucosa at four sites (0.5 ml each) near the tumor using a 23-gauge needle. During surgery, radioisotope uptake in each lymph node was measured using a Navigator GPS™ instrument (Dilon Diagnostics, USA). After laparotomy, SN excision was performed, followed by gastrectomy with lymphadenectomy. After resection, the absence of residual nodes with radioactivity in the abdomen was confirmed intraoperatively using the Navigator GPS. RI uptake in all dissected lymph nodes was again measured after surgery. All dissected lymph nodes including SNs were examined by hematoxylin and eosin (HE) staining, immunohistochemical (IHC) staining using AE1/AE2, and reverse transcription polymerase chain reaction (RT-PCR) using markers for CEA (Fig. 24.2) [5].
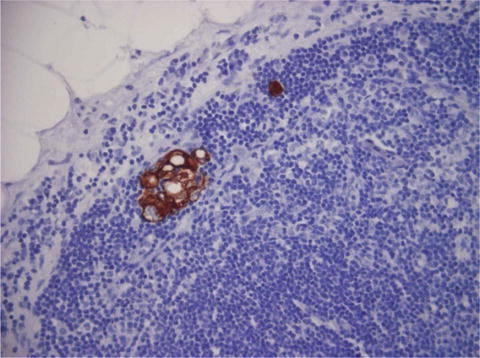
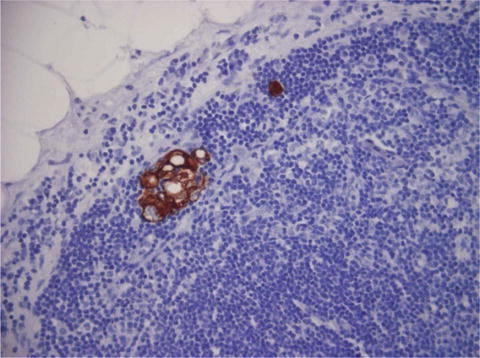
Fig. 24.2
Lymph node micrometastasis is detected by immunohistochemistry using AE1/AE3
Feasibility study was performed in 201 patients with clinical T1N0 gastric cancer. Detection rate of SNs is 98 % (197/201), and the average number of SNs is 4.0. Metastasis was found in 9.1 %, and micrometastasis was found in 9.1 % by IHC and 10.1 % by RT-PCR, respectively. A total of 56 patients had lymph node metastasis including micrometastasis. The sensitivity and accuracy of SN mapping in HE staining were 94.4 % and 99.5 %, respectively. The sensitivity and accuracy of SN mapping in IHC staining were 97.2 % and 99.5 %, respectively. Both sensitivity and accuracy of SN mapping by RT-PCR were 100 %. These results of feasibility study were thought to be promising for clinical application.
In 2013, the results of a prospective multicenter trial were reported from Japanese group for SN navigation surgery [6]. Three hundred ninety-seven patients were enrolled in this study. Detection rate, sensitivity, and accuracy were 97.5 %, 93 %, and 99 %, respectively, and the number of false negative cases was only four. In these cases, two had advanced tumors and lymph node metastases were included within the same lymphatic basin in three. Accordingly, we guess that SNNS by lymphatic basin dissection is feasible.
Infrared Imaging with ICG for SN Detection in Early Gastric Cancer
SN detection using infrared imaging with ICG has been clinically applied to melanoma and breast cancer. Infrared imaging may greatly contribute to the development of further SN detection in patients with gastric cancer. Lymphazurin and patent blue have been used for dye method in many facilities, but these are unauthorized for a drug of the lymph node identification in Japan. On the other hand, ICG is commonly and safely used for liver function test. The dye method is simple and easy, but there are some observation limitations due to the small size of the dye particles. RI method was used in our feasibility study, because of the difficulty in identifying blue nodes in a stomach with much fat and connective tissue.
Regarding infrared imaging for SN detection in gastric cancer, Nimura et al. reported the utility of infrared ray electronic endoscopy (IREE) combined with ICG in 2004 [7]. In this report, lymphatic vessel and SNs which took in ICG are found in absorbance imaging by IREE, but these are not found in white light. All of the 84 patients were detected SNs by IREE, and both sensitivity and accuracy are 100 %.
Clinical Application Based on SN Concept Using Infrared Red Imaging
Recently, IRI system was made by Olympus. Fluorescence imaging is clearer than absorbance imaging. This system is easily switchable in absorbance and fluorescence view, and we find lymphatics clearly, and SNs are confirmed easily (Fig. 24.3). Recently, we used this system for SN detection in early gastric cancer. Technetium tin colloid and ICG are injected 1 day before surgery. ICG is used for 0.25 mg/ml in diluted form. There are some reports regarding intraoperative ICG injection. Since both lymphatic vessels and blood vessels are visualized in this procedure, it is difficult to discriminate between lymphatic and blood vessels. Therefore, we inject it 1 day before surgery. Fluorescence nodes (FNs) are identified using IRI system and marked by surgical clip during surgery (Fig. 24.4). A lot of FNs are identified in back table, due to the manipulation of stomach and omentum. The number of SNs has a limit for the pathological diagnosis during operation. Thus, it is important to confirm FNs carefully and mark it by surgical clip before the manipulation of gastric wall and omentum. FNs and hot nodes with RI were confirmed in back table, and SNs were examined by HE staining and RT-PCR during surgery [8]. The presence or absence of SN micrometastasis is an important issue, although the clinical significance of lymph node micrometastasis is controversial in gastric cancer [9]. Laparoscopic partial resection or segmental resection is applied to patients without metastasis in SNs determined by pathological examination and RT-PCR assay (Fig. 24.5).