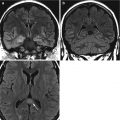
Fig. 24.1
Silhouette sign: Left panel is a normal chest radiograph demonstrating the “silhouette” sign. The mediastinum, heart and diaphragm are sharply delineated against the aerated lung. Frontal (middle) radiograph in a different patient shows obscuration of the right heart border due to consolidation (white arrow) in the immediately adjacent lung (right middle lobe). On the lateral film (right panel) the consolidation (white arrow) has a straight margin as it abuts the fissure
Lobar Pneumonia
This is the most common manifestation of a community-acquired pneumonia and typically results from a pneumococcal (Streptococcus pneumoniae) infection after airborne transmission. The localized inflammatory reaction causes the exudate to spill into the adjacent alveoli. This process spreads from the distal air spaces via the pores of Kohn, and may progress to occupying a whole lobe. As the central airspaces are patent despite the distal ones being compromised, the typical radiographic appearance is an air bronchogram without significant volume loss. In patients with a potential malignancy, a central obstructing lesion needs to be considered as being suspicious (Fig. 24.2).


Fig. 24.2
Lobar pneumonia. Homogeneous consolidation involving left upper lobe with multiple air bronchograms and no volume loss
Bronchopneumonia
This is the result of the inflammatory exudate localizing around inflamed airways but respecting septal boundaries. Some acini are involved while others are spared. The exudates initially originate around the terminal and respiratory bronchioles rather than the distal airspaces in lobar pneumonia. Several foci of infection usually develop resulting in the radiographic appearance of multifocal nodular or patchy consolidation. Air bronchograms and volume loss are usually absent. Numerous organisms can result in bronchopneumonic patterns (Fig. 24.3).


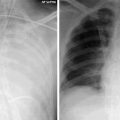
Fig. 24.3
Bronchopneumonia. There are ill-defined nodular opacities with patchy inhomogeneous consolidation involving several lobes
Interstitial Pneumonia
This predominantly involves the supporting interstitium between the airspaces/alveoli. Bronchial and bronchiolar walls become infiltrated and edematous with further extension from the peribronchial tissues into the interlobular septa. The inflammatory process can also progress into the terminal air spaces and alveoli. The usual radiographic appearance is a reticulonodular pattern reflecting the compromised peribronchial and interstitial tissue. The infective organisms tend to be viral or Mycoplasma pneumoniae (Fig. 24.4).
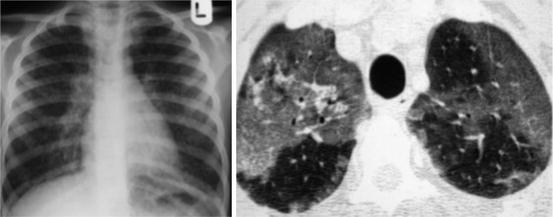
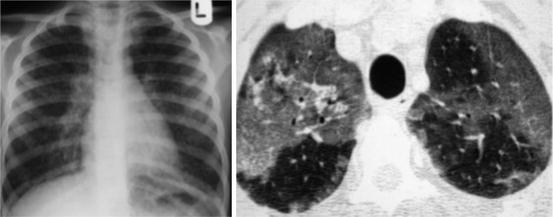
Fig. 24.4
Interstitial pneumonia. CXR shows subtle ground glass and fine reticular pattern. These features are more readily appreciable on the HRCT where there are patchy bilateral centrilobular opacities
Cavitating Pneumonia
This often rapidly spreading, destructive process is usually caused by Staphylococcus aureus, gram-negative bacteria, fungal infections or Mycobacterium tuberculosis. Pneumatoceles may mimic cavitations and are defined as air cysts more than 1 cm in size and a wall thickness of less than 4 mm (Fig. 24.5a, b). If there is co-existing emphysema with bullae, consolidated lung can give a similar appearance to cavitation.
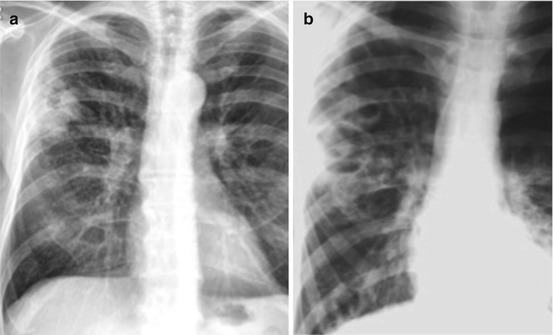
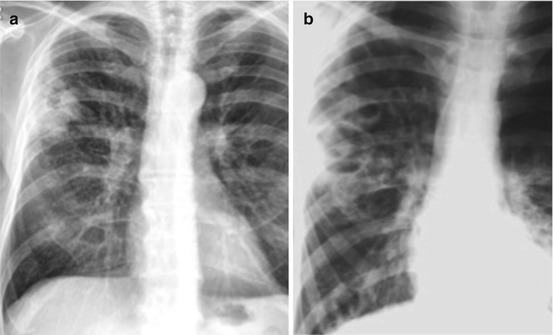
Fig. 24.5
(a). Left image is from a 52 years old male with history of alcohol excess, presenting with pyrexia. There is a thick walled cavitating lesion in the right upper lobe due to Staphylococcus aureus pneumonia. (b) Pneumatocle, approximately 4 weeks after the initial film
Ventilator-Associated Pneumonia (VAP)
VAP is the most common healthcare associated infection in ICU and may account for up to half the antibiotic use. It occurs in up to 30 % of ventilated patients, its incidence is quoted as 5 cases per 1,000 ventilator days. It carries a mortality of 9 %.
In the absence of a consensus definition it is generally accepted that VAP is a clinical diagnosis. Table 24.1 details the criteria for diagnosis as proposed by the Centre for Disease Control and Prevention.
Table 24.1
CDC criteria for diagnosis of VAP
Radiological signs | 2 or more serial chest X-ray with at least 1 of |
New or progressive and persistent infiltrate | |
Consolidation | |
Cavitation | |
Microbiological criteria | At least 1 of |
Positive blood culture not related to any other source of infection | |
Positive sputum culture from lavage or protected specimen brushing | |
>5 % of cells with intracellular bacteria on direct microscopy of gram-stained lavage fluid | |
Histopathological evidence of pneumonia | |
Clinical signs | At least 1 of |
Temperature >38 °C | |
White cells >12,000 or <4,000 | |
Altered mental status in patients >70 years without any other recognized cause | |
Other signs | At least 2 of |
New onset of purulent sputum or change in character of sputum | |
Increased respiratory secretions | |
New onset of cough, dyspnea or tachypnea | |
Rales or bronchial sounds
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|