Fig. 12.1
a TC 3D pre-op. CT 3D Reconstruction in plurifragmented and displaced fracture of the neck and greater tuberosity of the humerus. b X-ray post-op. X-ray antero-posterior in extrarotation and intrarotation with prosthesis
The surgical steps for this prosthesis are as follows:
1.
Place the patient under anaesthesia (general or block) in the beach-chair position.
2.
A classical Larghi skin incision is made to visualize the fracture in the operating field.
3.
Definitive fibre wires (2 or 5) are passed around the greater tuberosity and 2 temporary ones around the lesser tuberosity (for a total of 6).
4.
The head is removed and measured. Should the size fall in between sizes, then the smaller size is selected.
5.
The medullary canal is prepared by hand with cylindrical reamers of increasing diameter and an Aequalis fracture stem (Tornier, St. Ismier, France) of the correct diameter is selected.
6.
The correct head and stem are put together.
7.
The two diaphysis holes are prepared and two other fibre wires (2 or 5) are passed through, ready for final tensioning of the tuberosity.
8.
The cement is placed into the canal.
9.
The stem is cemented to the predetermined depth and rotation, in slight valgus, taking care to ensure that the distance between the top of the head and the upper margin of the pectoralis major is 5.6 ± 0.5 cm [14].
10.
A cancellous bone graft wedge is placed in the “window” of the fracture prosthesis, under the greater tuberosity and the medial edge of the prosthetic head.
11.
The last step is to fix and tighten the tuberosity around the prosthesis with the 6 suture configuration technique, described by Boileau (Fig. 12.2 e 3)
Fig. 12.2
a X-Ray pre-op 1. X-ray antero-posterior view in extrarotation: plurifragmented and displaced fracture of the neck of the humerus. b X-ray pre-op 2. X-ray transthoracic view: plurifragmented and displaced fracture of the neck of the humerus. c X-ray pre-op 3. X-ray antero-posterior oblique view: plurifragmented and displaced fracture of the neck of the humerus. d X-ray post-op 1. X-ray antero-posterior view in extrarotation treated with inverse prothesis: plurifragmented and displaced fracture of the neck of the humerus. e X-ray post-op 2. X-ray antero-posterior view in intrarotation treated with inverse prosthesis: plurifragmented and displaced fracture of the neck of the humerus
12.
The shoulder should be passed through a full range of motion to ensure that there is no micromotion of the tuberosity fragments. There should be a passive intraoperative range of motion of at least 160º of elevation, 40º of external rotation and 70º of internal rotation. With the arm in 20º to 30º of external rotation, the rotator interval or surgical rotator cuff split is closed and the biceps is tenodesed within the intertubercular groove/rotator interval to soft tissue.
13.
Post-operative care requires a sling and passive motion for the first six post-operative weeks.
International literature reports that the functional results of hemiarthroplasty are unpredictable with either a very good or very bad outcome, when anterior active elevation, active external rotation, active internal rotation and pain are taken into consideration, as can be seen in adjusted constant score [15].
Therefore, as it gives more constant results and the outcome depends on the tuberosity healing, reverse shoulder arthroplasty (RSA) has been suggested as an alternative (Fig. 12.2). However, although the results of RSA are good and more predictable, they are not so good as in cuff tear arthropathy (CTA). Results with the traditional RSA were not always very encouraging [16]. Therefore, prosthesis manufactures improved on the design and surgeons worked on their techniques. Indeed, the use of the reverse shoulder prosthesis simplifies post-operative care and provides quicker recovery, more predictable results, better fixation of the greater tuberosity and better healing of acute fractures. This is particularly true in patients over 75, women with osteopenia and in cuff tears as well as poor compliance with rehabilitation. It is also very useful for greater tuberosity comminution, thin cortical bone, combined fractures of the glenoid and humerus and severe fatty infiltration of the rotator cuff muscles [17]. RSA restores active elevation despite cuff deficiency and improves shoulder function after failed HA for fracture. As aforementioned, the tuberosity healing is also important in the RSA, the technique and/or the design of the reverse prosthesis for fractures with a specific technique for tuberosity fixation has been improved, permitting the tuberosity healing and attachment, so as to restore the active external rotation (AER) [18].
12.2.2 Modular Prosthesis
The first modular shoulder prosthesis came onto the market at the end of the 1980s. An identical head and glenoid radius were no longer used, but rather the mismatched glenoid, i.e., a different radius between humerus and glenoid [19]. While the third generation imitates the 3D bony anatomical parameters of the shoulder and recreates the gleno-humeral joint according to patient anatomy [20], the system modularity free sets the basic parameters, like the humeral head diameter, retroversion angle, implant height, eccentricity and offsets (posterior and medial) of the head [21, 22] (Figs. 12.3, 12.4). These prostheses have a stem, which may be cemented or uncemented (Fig. 12.5). Likewise, the glenoid component may be all in polyethylene or with a metal back. Typically, shoulder replacement with a modular prosthesis is performed in patients with advanced cartilage degeneration due to wear, disease, bone loss, osteonecrosis or trauma. Occasionally, a tumour makes a shoulder prosthesis necessary [23]. There are various models on the market: Acumed, Biomet, Cofield (Smith and Nephew), DePuy, Encore, Exactech, Neer, Stryker Solar, Tornier, and Zimmer.
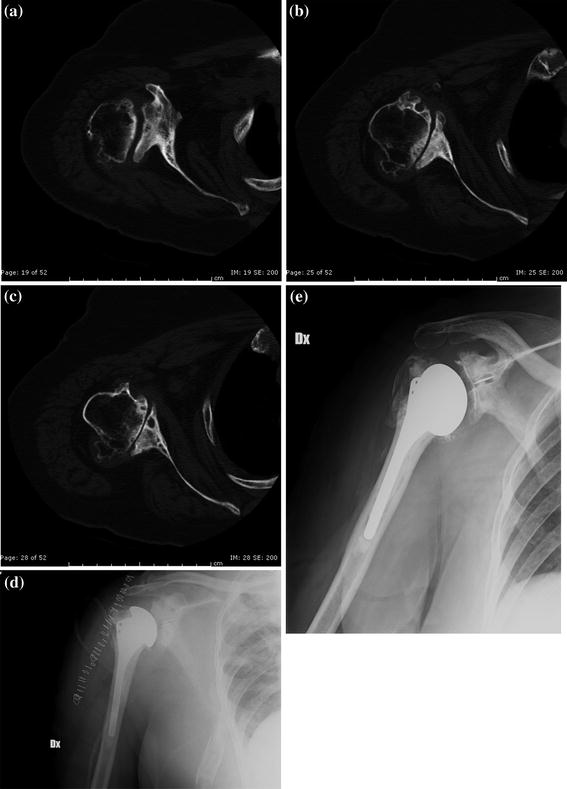
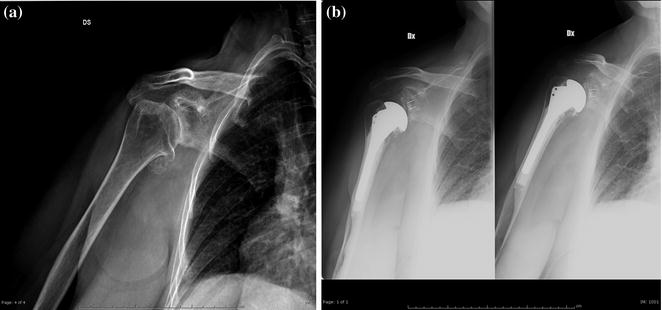
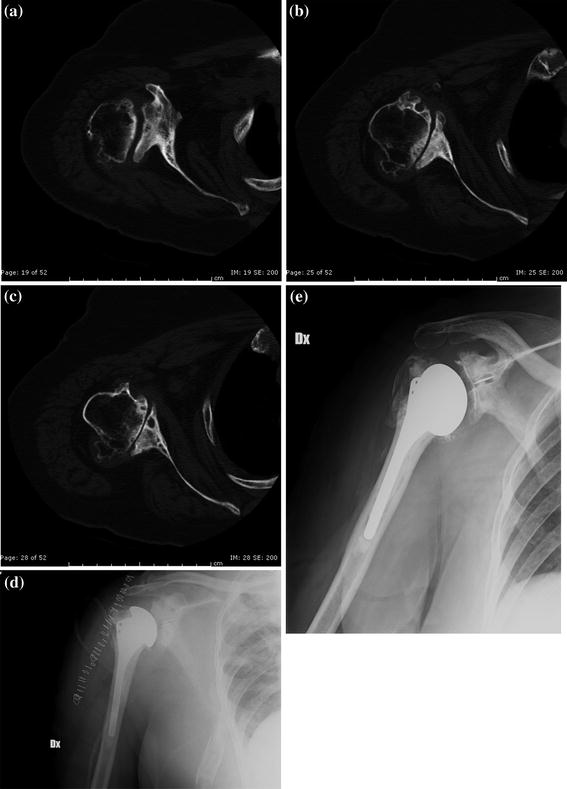
Fig. 12.3
a pre-op TC 1. TC axial view in severe gleno-humeral arthrosis. b pre-op TC 2. TC axial view in severe gleno-humeral arthrosis. c pre-op TC 3. TC axial view in severe gleno-humeral arthrosis. d PO 1. X-ray antero-posterior view in extrarotation treated with anathomic prothesis: severe gleno-humeral arthrosis. e PO 3. X-ray antero-posterior view in intrarotation treated with anathomic prosthesis: severe gleno-humeral arthrosis
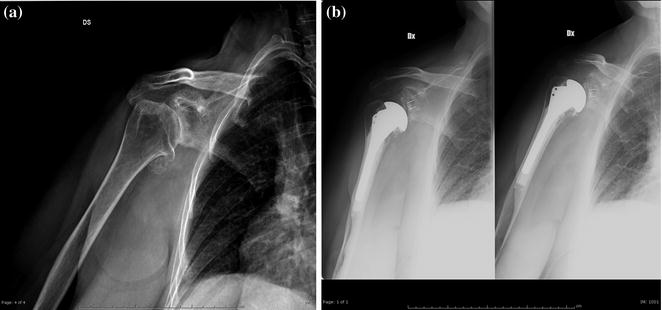
Fig. 12.4
a A4 pre-op. X-ray antero-posterior view in extrarotation: severe gleno-humeral arthritis. b A4 post-op. X-ray antero-posterior view in extrarotation and intrarotation treated with anatomical prosthesis: severe scapular-humeral arthrosis
Fig. 12.5
a Ascend pre-op. X-ray antero-posterior in intrarotation and extratotation view: severe gleno-humeral arthritis. b Ascend post-op 1. X-ray antero-posterior in intrarotation view: severe gleno-humeral arthritis treated with “ascend” prosthesis. c Ascend post-op 2. X-ray antero-posterior in intrarotation and extrarotation view: severe gleno-humeral arthritis treated with “ascend” prosthesis
The technique of total shoulder arthroplasty foresees the following:
1.
placing the patient in the beach-chair position with the torso flexed between 30° and 45° and knees flexed to 30°; the patient must have the shoulder lying far enough off the side of table so that it can be fully extended, externally rotated to avoid interference, space for some adduction should also be allowed;
2.
the extended deltopectoral approach is used;
3.
the arm is placed in adduction and external rotation may reduce the risk to the axillary and musculocutaneous nerves;
4.
the axillary nerve is identified;
5.
the subscapularis is mobilized (360° release) and detached from its insertion on the lesser tuberosity and is incised together with the underlying anterior aspect of the capsule. Alternatively, an osteotomy of the small tuberosity may be performed to restore the bone to bone relationship;
6.
check for any loose bodies and remove them;
7.
prepare the humerus and component insertion;
8.
prepare the glenoid and component insertion:
9.
wound closure: it is essential to obtain a tight closure of the subscapularis tendon, whether it be bone to bone, tendon to tendon or bone to tendon, since avulsion of the tendon at the repair site often leads to anterior instability.
12.2.3 Resurfacing Prosthesis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree