Shoulder Girdle Injuries
Acromioclavicular Joint Dislocation
Acromioclavicular (AC) dislocation is a common injury due to the prominence of the AC joint at the superolateral aspect of the shoulder. The bony anatomy of the shoulder girdle makes the AC joint vulnerable to direct force with any blow to the shoulder, such as during a fall onto the shoulder or lateral impact in a motor vehicle accident.
The AC joint is a synovial joint that contains a round meniscus composed of fibrocartilage. The lateral clavicle is connected to the upper extremity by the coracoclavicular (CC) and coracoacromial (CA) ligaments and AC joint capsule. The AC joint capsule is strongest at its superior and posterior margin.1 AC joint dislocation occurs when there is at least partial disruption of these structures. Proper diagnosis of shoulder separation and careful selection of patients for surgical intervention following AC joint injury are required to minimize arthrosis, instability, and dysfunction.
The AC joint plays an important role in suspension of the upper extremity to the axial skeleton. This articulation may allow for up to 20 degrees of rotation2 and is further affected by the weight of the upper extremity as well as large muscular forces that act across a small surface area. These factors help to explain why internal fixation failures are common, and why there are so many described techniques to repair fractures and dislocations of this joint, because most have been associated with a high failure rate.
Distal clavicle fractures are discussed at the end of this chapter; however, much of the same discussion regarding the diagnosis and treatment of AC dislocations is relevant to the displaced or intra-articular distal clavicle fracture as well.
Classification
Both Tossy et al3 and Allman4 developed classification systems for AC dislocations based on the degree of ligament injury and radiographic evidence of displacement (see text box).
The joint may sustain a nondisplaced sprain referred to as type I. The type II injury is incompletely displaced and thought to be associated with complete tearing of the AC ligaments, but relatively sparing of the CC ligaments. The type III dislocation represents complete disruption of the CC ligament and AC joint capsule with superior displacement. Rockwood et al5 later described three additional types of more severe injury (types IV through VI) based on the direction as well as the amount of dislocation. Rock-wood′s type IV AC dislocation is complete, and the clavicle is displaced posteriorly. The type V injury is an extreme variation of type III, where the clavicle buttonholes through the trapezius into the subcutaneous tissue, whereas the type VI dislocation is dislocated inferiorly.
Combined Tossy and Allman Classification of Acromioclavicular Joint Separation
Type I
Partial tear of ligaments, minimal pain, point tenderness over the AC joint, and no laxity of the AC joint; normal plain films
Type II
Rupture of the capsule and AC ligament. Intact CC ligaments; pain and point tenderness over the AC joint; deformity may be present; plain films reveal an elevated clavicle extending less than the diameter of the clavicle
Type III
Rupture of both AC and CC ligaments; pain and point tenderness are noted over the AC joint and distal third of the clavicle; marked deformity is present; plain films reveal a wide separation between the clavicle and coracoid process
Clinical Assessment
Patients usually report a direct blow to the shoulder with a swollen and painful AC joint. A visual or palpable step-off or a distal clavicle that feels unstable is an indication that the injury is at least a type II. It is not uncommon for type I and II injuries to hurt for a longer period of time than type III injuries due to residual articular contact and tethering of partially torn ligamentous structures. Abrasions over the superolateral area of the shoulder must be noted if surgery is considered because surgery should be delayed until re-epithelialization has occurred.
An anteroposterior (AP) X-ray of the shoulder reveals the injury; however, visualization of the joint is improved with a 10-degree cephalic tilt view centered over the AC joint, also known as a Zanca X-ray view. Imaging of both AC joints on the same large X-ray cassette helps to demonstrate relative displacement, as well as anatomic variations of the AC facets. An increase in CC distance of 5 mm or > 25% usually indicates a complete tear of the CC ligaments.6 Weighted stress radiographs taken with the patient hanging weights in each hand are no longer routinely obtained because it is painful and rarely provides any new information that would change management.
Nonoperative Treatment
Indications
Rockwood type I and II AC injuries should be treated nonoperatively, with the expectation of excellent short- to midterm results.7 In the event that late, symptomatic AC arthrosis occurs, elective distal clavicle excision can predictably relieve pain and restore function.8 Nonoperative management can also be performed on type III AC dislocations, as the collective weight of evidence reveals no benefit from surgical treatment9,10; however, some authors believe that the overhead throwing athlete and manual laborer should undergo reconstruction, which is also the bias of the senior author of this chapter.11,12
Reductions, Casting Techniques, and Orthoses
Ice should be provided in the acute setting to relieve pain and swelling, and a sling is useful for support of the upper extremity against gravity. There is no benefit to closed reduction because the joint cannot be maintained in a reduced position with any orthosis, including a figure-of-eight sling.
Rehabilitation
A sling may be used for 2 to 3 weeks to support the extremity during the acute phase of pain if the patient desires. Function is advanced as discomfort allows. Shorter or longer periods with relative rest are required according to the severity of the sprain or dislocation. Patient reassurance is necessary during months of resolving symptoms.
Surgical Treatment
Indications
Surgical reconstruction is indicated in patients with Rock-wood type IV to VI AC injuries to prevent chronic dysfunction and pain. The management of type III injuries remains controversial. Most experts recommend nonoperative management, whereas others believe that overhead throwing athletes and manual laborers should undergo operative treatment for Rockwood type III AC injuries.11–16
Surviving the Night
Injuries of the AC joint rarely present with any issues that demand immediate treatment. One consideration would be to evaluate the patient for other chest, neck, or brachial plexus injuries that may be associated, depending on the mechanism of injury and associated fractures. Because type I and II injuries simply need treatment with a sling and expectant management, the key decision initially is whether the completely displaced AC joint is simply a type III or greater. Do not commit to surgery on type III injuries until the expertise of the surgeon and the expectations of the patient clearly dictate this intervention, as per the discussion in the previous section. If, however, the clavicle is displaced posteriorly and buttonholed through the triceps, or inferiorly, then urgent surgical management should be planned after appropriate diagnostic studies and resuscitation of the patient is complete.
Surgical Anatomy
Fusion of the secondary ossification centers about the AC joint occurs at around 17 years of age for the acromial portion and 24 years of age for the distal clavicle. The average size of the joint is 9 × 19 mm. Branches of the axillary, suprascapular, and lateral pectoral nerves innervate the AC joint.5 Urist10 found that the clavicle slightly overrides the acromion process half the time, and that 21% of AC joints are incongruent. The lateral clavicular facet actually underrides the acromion 3% of the time.11 Knowledge of individual variation is helpful during diagnostic and surgical interpretation of anatomy. The AC joint capsule is strongest at its superior and posterior margin. The scapula is suspended from the clavicle via the CC ligaments, consisting of the well-defined trapezoid and conoid ligaments. These structures run from the base of the coracoid to the undersurface of the clavicle. The trapezoid ligament spans from the coracoid base just lateral to the conoid ligament. These strong ligaments provide restraint against clavicular elevation.
Surgical Techniques
Many surgical procedures have been described to repair an AC dislocation. The strategies have included fixing the distal clavicle directly to the acromion, augmenting the CC ligaments, or both. Though each strategy can be employed in the acute or delayed setting, if a late reconstruction is done, it is usually combined with a distal clavicle resection.
The most widely known historical procedure is that described by Weaver and Dunn,17 in which the CA ligament is transferred through the end of a resected distal clavicle. Today, some surgeons prefer either allograft or autograft tendon reconstructions to replace the CC ligaments. In either case, fixation across the AC joint or into the coracoid base is often added to augment the soft tissue repair during healing. One potential problem related to mobilization of the CA ligament is the concept of superior escape of the humeral head. The CA ligament may indeed play a role in containing the concentricity of the humeral head.18–20
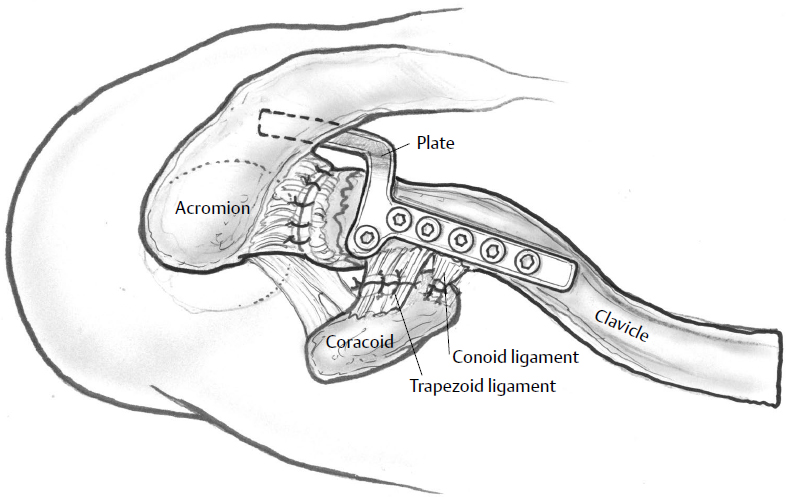
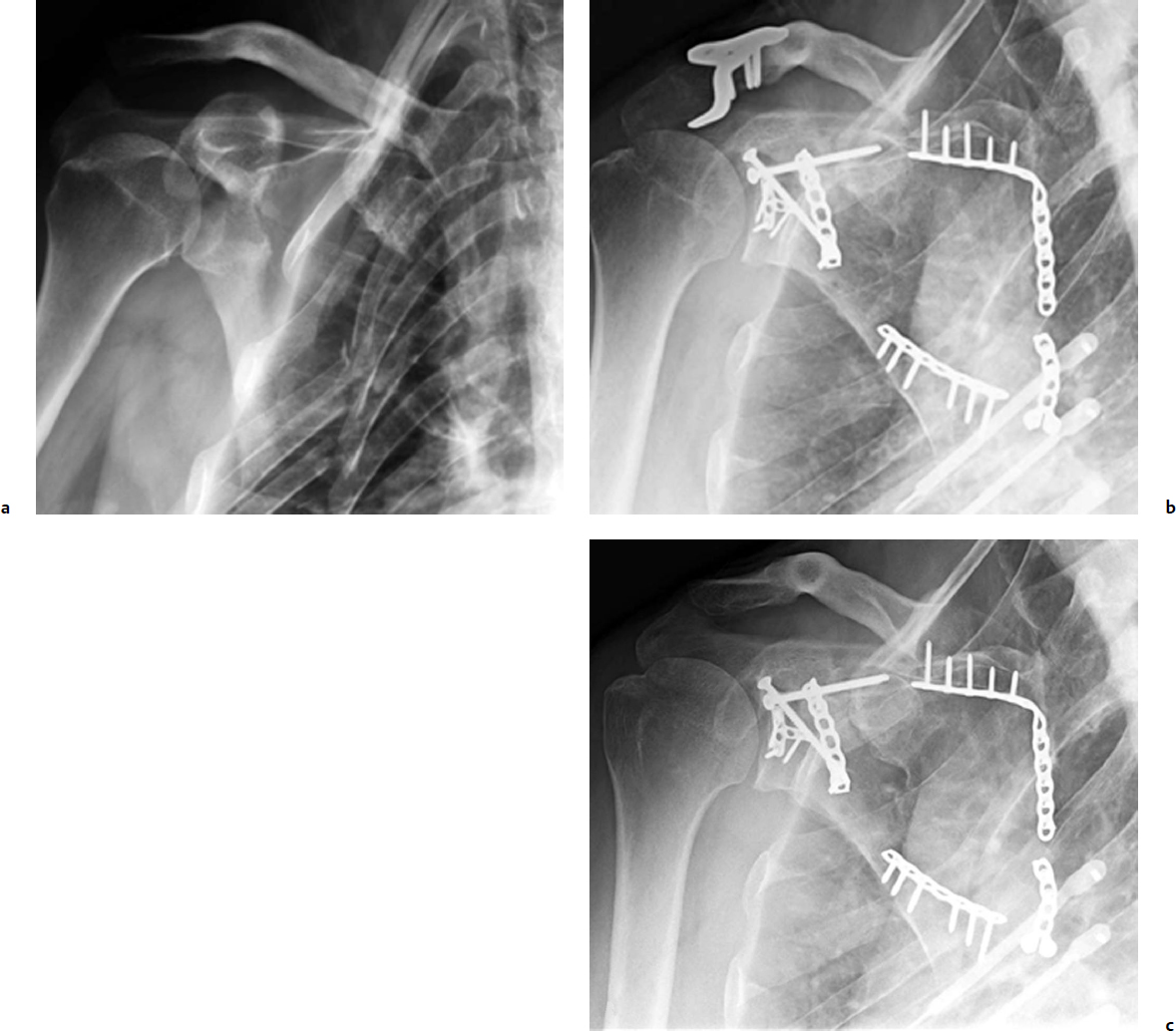
The Hook Plate (Synthes, Paoli, PA) has become an increasingly popular option for AC joint dislocations.21–25 The plate is fixed to the cephalad border of the distal clavicle, and a terminal hook sweeps under the acromion so the clavicle is restrained from springing superiorly (Fig. 13.1). This can be employed alone or in conjunction with CC ligament augmentation. It is recommended that the plate be removed at 3 to 4 months after surgery to prevent known complications of acromial osteolysis and possibly acromial fracture22,26–28 and impingement.29,30 An attempt to repair the AC joint as well as the CC ligaments should augment the use of the Hook Plate.
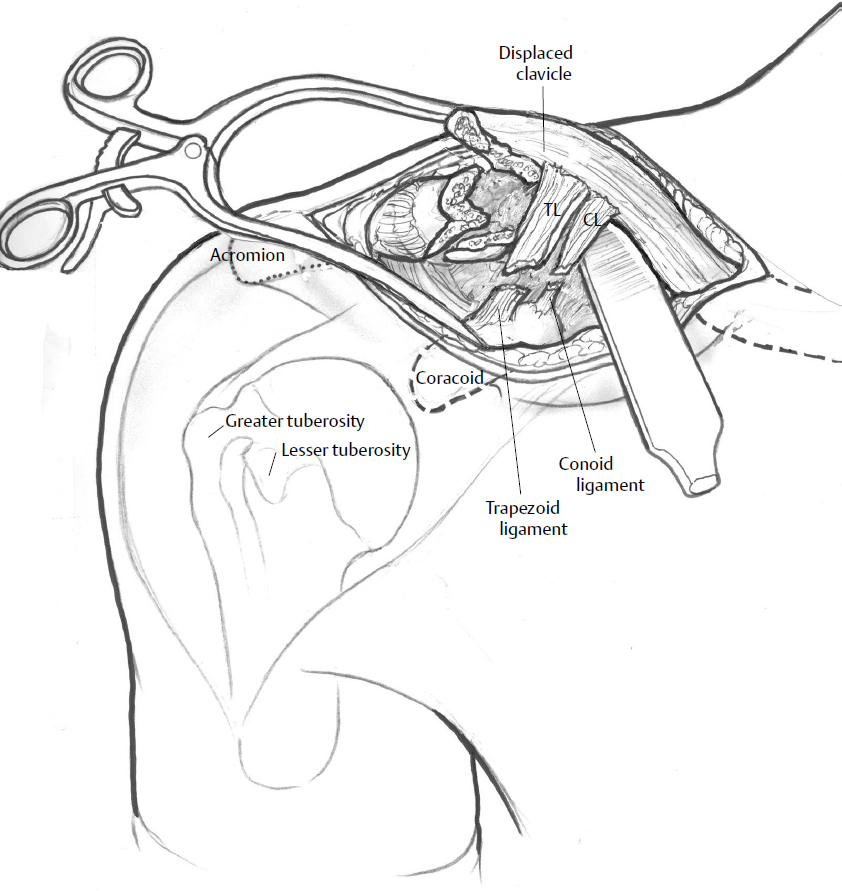
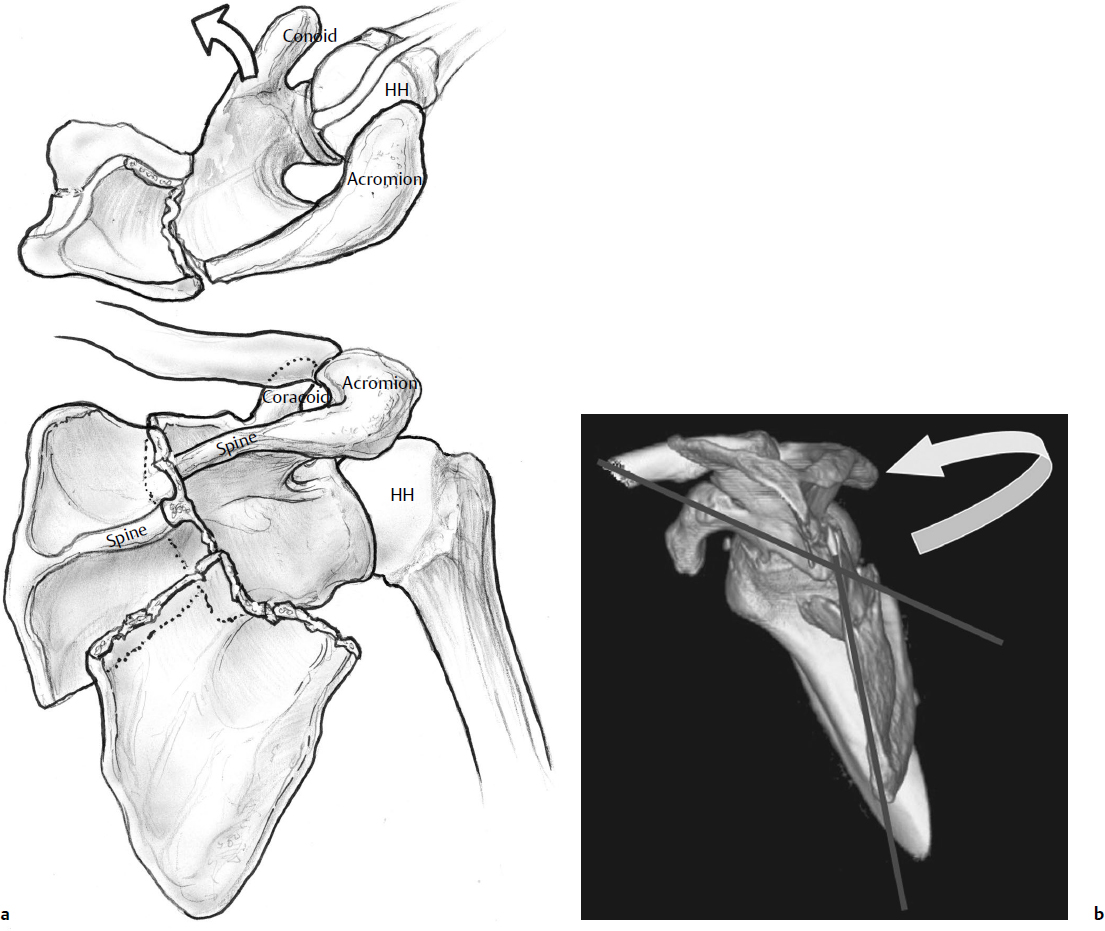
The same procedures have been employed for distal clavicle fractures, specifically those in which the shaft displaces superiorly due to ruptured CC ligaments (Fig. 13.2). The fixation and repair challenges of distal clavicle fractures, regarding maintaining reduction, are similar to the surgical challenges of AC dislocations due to the deforming force of the sternocleidomastoid muscle on the proximal clavicle shaft. However, in the case of distal clavicle, eventual bony union helps to maintain reduction after plate removal.
Positioning
The beach-chair position is utilized, and the entire fore-quarter and upper extremity are prepped and draped well up onto the neck. A towel or bump is not placed behind the shoulder during positioning because this maneuver will tend to accentuate the deformity of the clavicle. It is helpful to place an X-ray cassette optimally before draping so that the shoulder is accurately centered, facilitating a good intraoperative radiographic opportunity that should be taken prior to wound closure. The entire extremity should be sterilely prepped to facilitate evaluation of rotational nuances at the time of AC reduction by manipulating the arm, which can also aid closed reduction.
Incisions
A 6-cm incision centered over the anterior edge of the distal clavicle is made to expose the dislocated AC joint. The incision is made in Langer′s lines, and thus is vertically oriented, enabling direct exposure of the torn ligaments and an adequate exposure of the coracoid. The flaps between the deltoid and trapezius are carefully developed for later closure of the deltotrapezial tissue plane. After the distal clavicle and AC joint are exposed, the torn AC joint capsule is debrided. The articular integrity is evaluated, and if there are pieces of detached articular cartilage, they are removed. In the acute setting, the clavicle should be noted to reduce rather readily by an inferior directed force on it (in a type III injury), or pistoning the arm cephalad to meet the clavicle. The CC ligaments are then inspected for integrity, with the intention of repairing them if possible, but only after fixation of the AC joint.
If the surgeon elects to retain the distal clavicle, as in the acute AC disruption, a drill hole is made in the clavicle adjacent to where the native CC ligament attaches. Mersilene tape is then passed along the base of the coracoid under the conjoint tendon and anterior to the hook-shaped coracoid, then up through the drill hole in the clavicle, and sutured securely after reduction. The nonabsorbable synthetic tape is preferable to heavy suture due to the increased likelihood of “cutting out” the drill hole with suture, although certainly, given the strong deforming forces, the tape has been described as cutting through as well. The CC ligaments are then sutured primarily. Though the Hook Plate can be used in this scenario as well (Fig. 13.3), another way to enhance fixation is with the addition of a screw from the superior clavicle down into the coracoid base. A 6.5-mm partially threaded screw is used for this purpose, so that with the lag effect, the Mersilene tape is offloaded. As mentioned before, it is the our preference to plan for elective removal of the hardware, and this is done at approximately 3 months postoperatively, after CC ligament healing.
In the case of a symptomatic chronic dislocation, arthritic joint, or comminuted distal clavicle, the surgeon should perform a distal clavicle resection and subsequent reconstruction of the CC ligaments. The clavicle is simply cut back from its distal end to the area of insertion of the CC ligaments, about 1.5 cm proximal on the bone. The distal clavicle is prepared by opening and smoothing the exit point of the medullary canal, and a slightly more proximal hole is drilled in the cephalad surface of the clavicle. The CA ligament is then detached from its insertion on the acromion, and a No. 2 braided suture is passed in a Krackow or modified Bunnell technique through the end of the clavicle up through the drill hole, where it is then sutured as a loop around the distal resected clavicle. Again, this procedure can be augmented with the hardware options described above.
Rehabilitation
Patients undergoing surgical reconstruction of AC injuries should be protected in a sling for 4 to 6 weeks. Passive range of motion (PROM) exercises should be encouraged over this time period, but pushing, pulling, or reaching activities are not permitted to allow for deltoid reattachment. Active range of motion (AROM) may commence at 6 weeks postoperatively, and strengthening exercises at 8 weeks. Contact sports may be initiated at 16 to 20 weeks postoperatively and after hardware removal when this option is utilized.31
New Techniques
Video 13.1 Acute Type III AC Joint Separation
A new suture-button construct called the Tightrope (Arthrex, Naples, FL) is being used by some surgeons for fixation.23,32–35 It provides fixation between the coracoid process and the clavicle, which can be performed arthroscopically or through a mini-open approach. Another potential benefit is reducing the need for implant removal (Fig. 13.4). Although it has the advantage of not crossing the AC joint, it has been associated with fractures of the coracoid.

Tips and Tricks: AC Ligament
Augmentation of a ligament reconstruction with some type of fixation to offload the repair is a wise course of action. A screw, such as a modified Bosworth screw or a partially threaded 6.5-mm screw, from the superior clavicle down into the coracoid, is stronger than Kirschner wires that cross the AC joint or a plate that traverses (bridges) the AC joint because the fixation is perpendicular to the deforming force. The surgeon should plan for elective removal to prevent process erosion and fracture.
Due to the curved and slender shape of the distal coracoid, the surgeon should dissect along the proximal and posterior edge to appreciate the broader base into which fixation should be purchased. Otherwise, it is not uncommon to either fracture the coracoid or simply obtain poor purchase.
Draping the arm free during the reconstruction of an AC joint (and clavicle fracture) can enable near completion of the reduction and minimize soft tissue stripping with clamp applications.
Supplemental forms of anesthesia are useful for shoulder surgery. Begin with the infusion of a subdermal and subcutaneous local anesthetic mixed with epinephrine to decrease bleeding and intercept local pain pathways. Furthermore, it is useful to perform an interscalene block to supplement anesthesia. An indwelling interscalene catheter can be used for 1 to 2 days to facilitate early therapy.
Outcomes
The prognosis for type I injuries managed nonoperatively is excellent, whereas type II injuries have a good to excellent long-term prognosis.5 A small percentage of patients, mostly with type II injuries, develop symptomatic AC joint arthritis, requiring a distal clavicle resection.5,36 If conservative management fails, arthroscopic or open resection of the distal clavicle can be done by removing the distal 1.5 cm of bone, and results have generally been favorable.5,37–39
Complications
Most of the complications related to surgery involve failure of fixation, causing instability, recurrent prominence of the distal clavicle, and pain. Hardware failure occurs with any technique and may include slippage of Kirschner wires, cutout of CC screws, failure of grafts, or suture cutting through the distal clavicle or coracoid. Acromial erosion and fracture from retained Hook Plates, as well as fracture at the proximal end of the plate are known complications witnessed by the senior author (P.A.C.). These various modes of failure underscore the technically demanding nature of the reconstruction.
Scapula Fractures
Fractures of the scapula account for 3 to 5% of all fractures about the shoulder girdle.40–44 A study of 6,986 fractures found that 52 (0.7%) involved the scapula, which made it more common than distal humerus and distal femur fractures.45 Scapula fractures are usually evidence that formidable energy has been imparted to the body, and certainly so when it occurs in young and middle-aged patients. Large forces are required to cause a displaced scapula fracture, because of the well-endowed muscular envelope in which it lies, the mobility of the scapula on the thoracic cage, and surrounding musculoskeletal structures (proximal humerus, AC joint, and clavicle), which usually yield first.40
Fractures involving the glenoid neck and body in patients who sustain a direct impact to the posterosuperior or lateral forequarter are most often associated with other fractures and commonly with neurologic injury. Associated injuries occur in approximately 90% of these patients,41,42,46 though it has been found that mortality may be lower in this population even when controlling for injury severity score.47 This finding may be attributable to the shock absorption that occurs through the resilient thorax with commonly broken ribs.
Classification
Because of the rarity of this injury, only a few classification systems are commonly recognized for fractures of the scapula. The classification of Ada and Miller,43 as well as that of Hardegger et al,44 are comprehensive and anatomically defined.
Two classification systems were developed specifically for intra-articular glenoid fractures: those of Ideberg48 and the later modification by Mayo et al.49 The scheme of Mayo et al is a reorganized version of the Ideberg classification, but it takes into account the imaging and operative findings of 27 intra-articular glenoid fractures (see text box).
The intent of Mayo et al was to create a classification scheme that would direct surgical decision making. In so doing, there is emphasis on the associated scapula body and process fractures with which glenoid fractures commonly occur. This application may be the most useful for glenoid surgery. Scapula fractures have also been mapped from three-dimensional (3D) reconstructions to better illustrate the true nature of fracture patterns; these reconstructions could serve as a basis for a comprehensive classification scheme.50 More recent attempts to classify scapula fractures have been compromised by a lack of clinical correlation, failing to consider the associated in juries of the clavicle and AC joint, or lack of prognostic value.51–54
Ideberg Classification Modified by Mayo et al49
Type I
Transverse, anterior glenoid
Type II
Transverse, superior glenoid
Type III
Transverse, inferior glenoid
Type IV
Transverse, through body
Type V
Transverse through body and glenoid with associated coracoid, acromion, or neck fractures
Clinical Evaluation
The physical examination should reflect an understanding of the commonly associated injuries, particularly those that are life threatening. Determine whether or not the affected forequarter is medialized or depressed. Frequently, this displacement is obvious and disfiguring. This deformity is also a clue as to the amount of displacement and energy imparted.
Shoulder girdle injuries are frequently associated with neurovascular lesions, and they require an appropriate assessment of the brachial plexus and distal perfusion because 13% of patients with scapula fractures sustain a brachial plexus injury.49 The suprascapular and axillary nerves are at particular risk (Fig. 13.5),55 yet it is usually impossible to assess their motor function because of fracture displacement and pain; however, axillary nerve sensation should be documented. Abrasions over the scapula spine and acromion are common; therefore, skin integrity should be assessed for appropriate timing of surgery.


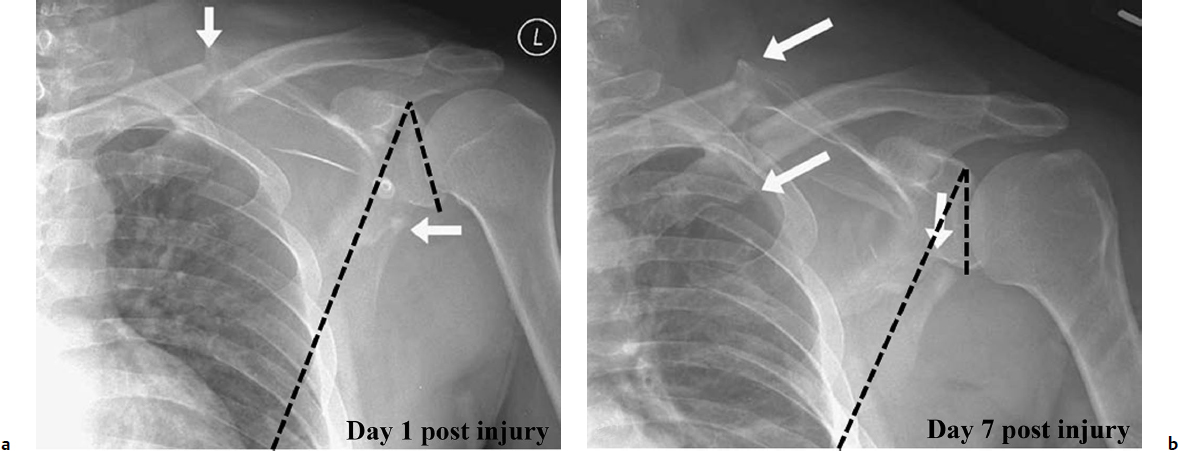
Regarding the radiographic examination, it is important to follow the displaced neck or body fracture closely. In our experience, it is not uncommon to see worsening angulation and medialization over the initial 2 to 3 weeks when the lateral border is “unhitched” or comminuted (Fig. 13.6). Anavian et al56 found that extra-articular fractures of the neck and body (Ada and Miller grade IIC43) may have a propensity to progressively displace.
Nonoperative Treatment
Indications
Isolated and minimally displaced scapula fractures should be treated expectantly. Treatment has emphasized symptom relief and early motion. In fact, because the shoulder is such a mobile joint, it can tolerate moderate displacement quite well, although the limits of tolerable displacement are not well identified in clinical studies. After motion is restored in the first 4 to 6 weeks, therapy is directed at rehabilitating the rotator cuff and strengthening the parascapular musculature. Because more than 80 to 90% of scapula fractures are minimally displaced, this noninvasive approach is effective for most of these fractures.42,43,57–64 Indications for surgery are becoming better accepted, as it seems clear that severe displacement, as described below, is associated with symptoms of stiffness, pain, and dys-function as evidenced by subsets of patients in many studies who have fared poorly.43,57,65–69
Displacement of the scapula is difficult to describe, both anatomically and with respect to the functional consequences. Clearly, significant displacement is better tolerated in some patterns of scapula fractures than in others. For example, the same amount of displacement may have different implications depending on whether it is the scapula body, neck, or glenoid. It is helpful to think in terms of extra-articular and intra-articular fractures. Regarding intra-articular fractures, a superior glenoid fracture in the horizontal plane, such as the Ideberg grade II, which often exits inferior and medial to the coracoid, is a more stable pattern than a posterior or anterior glenoid fracture of the same size, due to the implications for shoulder instability. Thus, a surgeon may be less inclined to operate in the situation where the glenohumeral joint will likely remain stable despite some degree of articular stepoff. Regarding scapular neck fractures, if a fracture enters the spinoglenoid notch, then the glenoid is more unstable than if it exits the spine of the scapula medial to the acromion base. Furthermore, a fracture exiting the scapular spine may be more unstable than a fracture exiting the medial vertebral border of the scapula. These implications are not well understood, and clearly there are different deforming forces on each fragment depending on where fractures enter and exit. Consider the forces from the levator scapula, the rhomboids, and latissimus as they interact on fragments depending on where fractures relate to insertions of these muscles. These nuances may influence slightly the indications for operative intervention based on a surgeon′s interpretation of relative stability in each situation.
Reduction and Casting Techniques and Functional Bracing
There is no known or identified role for closed reduction or casting. No brace has proven to be efficacious for scapula fractures.
Rehabilitation
If the scapula fracture is treated nonoperatively, a 2-week period of immobility while the arm is supported with a sling is appropriate. Active mobility of the elbow and wrist are encouraged in the immediate phase to reduce swelling. After this, the patient should begin passive motion, advancing to a full range as symptoms allow. It is helpful to begin with pendulum exercises and increase the PROM under the guidance of a therapist.
The patient should be taught to use the uninvolved extremity to assist with exercises. Scapula fractures will heal rapidly due to a well-endowed blood supply. Therefore, AROM can be started at 4 weeks and maximized quickly. Resistive exercises are begun by 8 weeks, and restrictions lifted (including weight bearing) as symptoms allow by 3 months.
Surgical Treatment
Indications
Displaced articular fractures of the glenoid are the clearest and most accepted indication for surgery. Although some studies recommend initial displacement of between 2 to 10 mm,49,70,71 we recommend 4 mm of step or gap as an appropriate indication for surgery72,73 (Fig. 13.7a,b). If humeral head subluxation, early arthrosis, and a poor outcome are to be prevented, open reduction and internal fixation (ORIF) should be performed.41,58,72,74 (Fig. 13.8).



Displaced fractures of the scapula neck should be treated operatively if displacement or angulation causes functional imbalance of the parascapular musculature. There is no agreement as to the exact definition of a neck fracture, but the variant entering lateral to the acromion base is most unstable; however, the variant entering medial to the acromion base, when displaced and angulated, can still be highly problematic.65 Though the original contemporary surgical recommendations by Ada and Miller43 included a medially displaced glenoid more than 9 mm or 40 degrees of angular displacement of the neck and body, more recent recommendations have allowed for more displacement, and are based on the interpretation of results from larger clinical series. We recommend considering operative intervention if relative displacement between the lateral border of the scapula and the glenoid exceeds 20 mm, or the lateral border angular deformity exceeds 45 degrees (Fig. 13.7c–f). Simultaneous displacements of > 15 mm and 30 degrees of angulation are also an indication that multiple planes of deformity should be considered.73,75
Perhaps the greatest amount of information correlating poor outcome with malunion relates to the deformity in the coronal plane, described as the glenopolar angle (GPA). This is the angle between vectors drawn from the inferior to superior edge of the glenoid, and then from the superior glenoid to the inferior body on an AP scapula view (Fig. 13.7c,d). Multiple studies show an association between poor outcome and a GPA < 20 degrees.66,69,76,77 We use 22 degrees as our indication, but also obtain an opposite-shoulder AP radiograph to compare to the normal side.
Double disruption of the superior shoulder suspensory complex (SSSC) is another indication for surgical treatment of scapula fractures. The SSSC is an osseoligamentous ring made up of the glenoid, coracoid, and acromion processes, as well as the distal clavicle, the AC joint, and the CC ligaments.59 The superior strut is the middle clavicle, and the inferior strut is the neck of the scapula. Lesions to two or more of these structures theoretically destabilize the shoulder and create the “floating shoulder” lesion. Stabilization of one or both lesions has been recommended to restore integrity to the SSSC, thereby preserving its function of maintaining a stable relationship between the upper extremity and axial skeleton and providing a firm attachment for the many soft tissues that enable shoulder function.78
Our approach to these double lesions is to restore integrity of the SSSC with ORIF of both lesions (i.e., clavicle and scapula) if each are displaced greater than 1 cm (Fig. 13.9). We use an opposite shoulder AP radiograph and a computed tomography (CT) scan to make such a determination. One can be misled by a single AP X-ray of the injured shoulder because the glenoid may be significantly displaced and angulated, making it impossible to get a “true” AP view of the glenohumeral joint perpendicular to the normal plane of the scapula. Wijdicks et al79 demonstrated that whereas a clear view through the glenohumeral joint is used as the criteria for determining a true AP, even subtle rotation of the shoulder can affect measurements significantly.

The operative indications for performing open reduction and fixation of extra-articular scapula fractures can be summarized as follows:
Lateral border displacement (medialization) of > 2 cm
Angulation as determined by a scapula-Y view of > 45 degrees
Medialization and angulation of > 15 mm and 30 degrees, respectively
A glenopolar angle of < 20 degrees
Displacement of a clavicle and scapula fracture of > 1 cm (or complete disruption of an AC joint)
Intra-articular stepoff or gap of the glenoid > 4 mm
These indications are based on measurement techniques shown in Fig. 13.7 . These criteria are not absolute and must be placed in the context of the patient′s age, comorbidities, activity demands, and extremity dominance.
Other extra-articular fractures that require ORIF include displaced fractures of the scapular spine, coracoid, and acromion processes. Process fractures carry a poor prognosis when treated nonoperatively.30,57,60–62,80,81 Anavian et al81 published the largest combined series of scapula process fractures, detailing an indication for surgery of a centimeter of displacement to prevent malunion and nonunion, inclusive of techniques for fixation. If the acromion fracture heals in a caudad position, causing encroachment into the subacromial space, impingement can become a major problem, so at times surgery of the acromion may be indicated even is lesser displacements. This angular displacement must be taken into consideration.
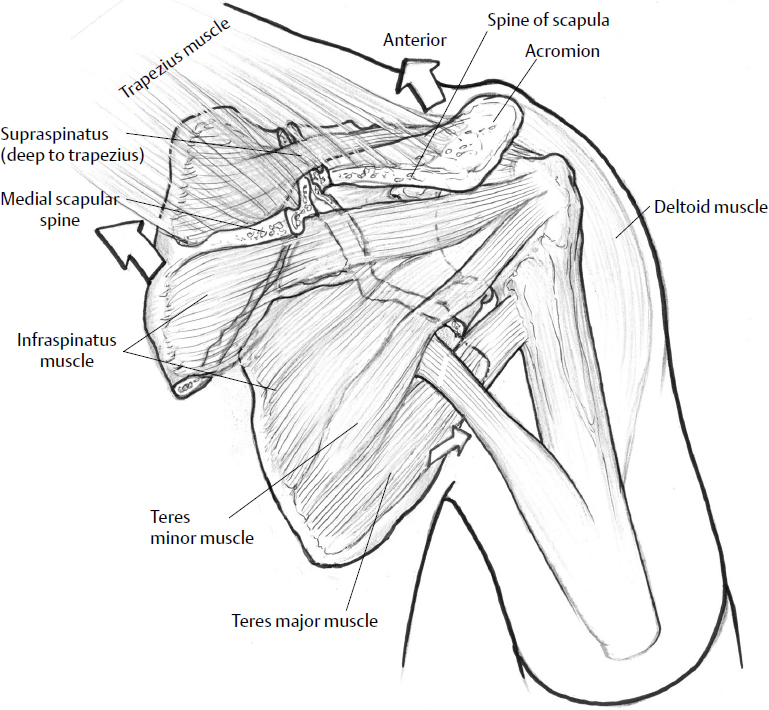
Surgical Anatomy
The scapula is approximately flat and triangular, with a thin translucent body, surrounded by borders that are well developed because of their positions as muscular origins and insertions. When fractured, landmarks are a bit harder to appreciate because predictable deforming vectors are at work based on muscular forces (Fig. 13.10). The scapular spine divides the superior and inferior angles of the scapula, thus forming the supraspinatus and infraspinatus fossae, which are origins for their respectively named muscles (Fig. 13.11). Its concave anterior surface serves as a broad origin for the subscapularis muscle.
Surviving the Night
Significantly displaced scapula fractures are associated with many bodily injuries: 15% have cervical spine injuries, 15% have a traumatic brain injury, 15% have brachial plexus and peripheral nerve injury, and a majority have multiple broken ribs and resultant hemopneumothorax; thus, all these conditions take more immediate priority. Therefore, thorough assessment of the brachial plexus and distal perfusion must be done at admission.
Occasionally, open wounds about the posterior shoulder communicate with a scapular fracture particularly at the AC joint or acromion. These should be irrigated and debrided emergently, but repair of the associated fracture, if warranted, can wait for an appropriately experienced surgical team.
Though the rare scapulothoracic dissociation should be identified, scapula fractures are almost never associated with this condition because the fractures occur from lateral impact, whereas dissociations result from traction to the extremity. The scapulothoracic dissociation has a high correlation with catastrophic injuries, including subclavian thrombosis or avulsion, and plexus lesions including cervical nerve root avulsion; thus, emergent vascular or spine consultation is needed. A single AP view of the scapula is not adequate for assessment of displacement, and the team working up a scapula fracture must acquire three views of the shoulder, including an axillary view to assess the glenoid. If there is significant displacement, then a 3D CT scan is necessary to appropriately understand the deformity, take measurements, and place the surgical decision-making process in proper context. Often the 3D CT scan highlights spectacular displacement that X-rays completely miss.
The spine of the scapula ends laterally as the acromion, which arches over the humeral head from which it is separated by the rotator cuff and subacromial bursa. Along with the clavicle, it serves as the origin of the deltoid muscle. The trapezius also originates on the acromion and scapular spine anteriorly. The medial border of the scapula is the site of attachment of the serratus anterior, which functions during scapula protraction, and the rhomboid muscles, which assist with scapular retraction. The levator scapulae muscle inserts on the superior medial border and is specifically named for its function. The lateral border of the scapula sweeps up from the inferior angle, forming a thick condensation of bone that ends in the neck of the scapula. The lateral border is the site of origin of the teres major and minor muscles, as well as the insertion for the long head of the triceps on the neck and part of the latissimus dorsi at the inferior angle. The coracoid process is a curved osseous projection medial to the anterior neck of the scapula, which serves as the origin for the CC and CA ligaments as well as for the coracobrachialis, short head of the biceps, and pectoralis minor muscles. Just above the coracoid process on the superior margin of the scapula is the scapular incisura, traversed by the transverse scapular ligament, above which lays the suprascapular artery and below which runs the same nerve.
The pear-shaped glenoid fossa lies at the lateral angle of the scapula, its peripheral margin covered by a fibrocartilaginous labrum that is confluent above with the long head of the biceps tendon at the supraglenoid tubercle. The labrum increases the depth of the glenoid by 50%.63 The glenoid fossa is approximately 39 mm in a superior-inferior direction and 29 mm in an anterior-posterior direction in its lower half, which is 20% wider than the top half.64
The scapula is part of the superior shoulder suspensory mechanism, which attaches the upper extremity to the axial skeleton by the clavicle. Eighteen muscle origins and insertions on the scapula aid in its function to provide a stable base from which glenohumeral mobility can occur.82
Surgical Techniques
Video 13.2 ORIF Scapula Posterior Approach
Logical operative approaches should provide adequate exposure of the fracture, add as little structural damage as possible, and take into account the restorative capacity of the biological repair process.83 Most scapula fractures are best operated by some modification of the posterior approach of Judet or the anterior deltopectoral approach.
Posterior Approach
Positioning
The patient is placed in the lateral decubitus position, “flopping” slightly forward for better access to the posterior shoulder. An axillary roll must be appropriately positioned. Arm rests, towels, or specially designed positioning bumps should support the extremity in 90 degrees of forward flexion and slight abduction (Fig. 13.12). The entire upper extremity and forequarter should be prepped and draped to allow manipulation of the shoulder. Manipulation after fixation in delayed fractures is important to overcome the contractures. From a posterior view, the prep should include patient′s neck superiorly, the vertebral column medially, and the latissimus fold caudally.

Incisions
The key to a successful surgical incision is accurate palpation of the bony landmarks of the acromial spine and vertebral border of the scapula. The prominent posterolateral acromion is palpated and followed medially to the base of the spine of the scapula, and then caudad along the vertebral (medial) border. It is very helpful to manually protract and retract the scapula by grabbing the arm and “shucking” it medially and laterally to create scapulothoracic excursion. This enables the surgeon to feel the vertebral border as it is indirectly manipulated. Note that the incision makes an acute angle at the superomedial corner of the scapula.
A Judet posterior incision is planned using these landmarks, with the horizontal limb 1 cm caudad/distal to the scapular spine and the vertical limb 1 cm lateral to the scapular vertebral border. This adjustment places the scar off the prominent bony border for better plate coverage and enables lateral retraction of a slightly less voluminous flap.
The incision is made through subcutaneous tissue and then directly down onto the bony ridge of the scapula spine around to the medial angle and down the vertebral scapular border. For access to the lateral border of the scapula, the incision must be sufficiently generous to facilitate flap retraction. Properly executed, the fascial incision along the acromial spine and medial border should yield a cuff of tissue to suture back to its bony origin at the end of the procedure if the posterior musculature is elevated (Fig. 13.13).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








