, Mark J. Jameson2, Max Wintermark3 and Sugoto Mukherjee4
(1)
Division of Neuroradiology, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
(2)
Division of Head and Neck Surgical Oncology, Department of Otolaryngology – Head and Neck Surgery, University of Virginia Health System, Charlottesville, VA, USA
(3)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(4)
Division of Neuroradiology, Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
Abstract
The bony skeleton of the nose is formed by the nasal bones and the nasal processes of the maxillae. The nasal septum is comprised of the septal cartilage anteriorly, the vomer posteroinferiorly, and the perpendicular plate of the ethmoid bone superiorly. The Kiesselbach’s/Little’s area is located in the anterior/inferior septum, and this is where branches of the sphenopalatine, greater palatine, and facial arteries anastomose; it is the most common site of epistaxis.
9.1 Anatomy and Physiology
9.1.1 Nose and Nasal Cavity
The bony skeleton of the nose is formed by the nasal bones and the nasal processes of the maxillae. The nasal septum is comprised of the septal cartilage anteriorly, the vomer posteroinferiorly and the perpendicular plate of the ethmoid bone superiorly. The Kiesselbach’s/Little’s area is located in the anterior/inferior septum, and this is where branches of the sphenopalatine, greater palatine, and facial arteries anastomose; it is the most common site of epistaxis.
The piriform aperture is the anterior bony opening of the nasal cavity. The posterior choana is the posterior opening, divided in the midline by the vomer.
The roof of the nasal cavity is formed by the cribriform plate of the ethmoid bone. The floor is formed anteriorly by the palatine processes of the maxilla and posteriorly by the horizontal processes of the palatine bones.
Three meati (spaces) are present along the lateral wall of the nasal cavity lateral to the superior, middle, and inferior turbinates. They contain the sites of drainage of the paranasal sinuses.
9.1.2 Paranasal Sinuses
There are three or four turbinates, designated as supreme (variable), superior, middle, and inferior. The inferior turbinate is a separate bone, while the other three are parts of the ethmoid bone. The middle turbinate is attached to the lateral nasal wall by the basal lamella, which separates the anterior and posterior ethmoid air cells. The space between the basal lamella and the ethmoid bulla is the sinus lateralis or suprabullar recess (Fig. 9.1).
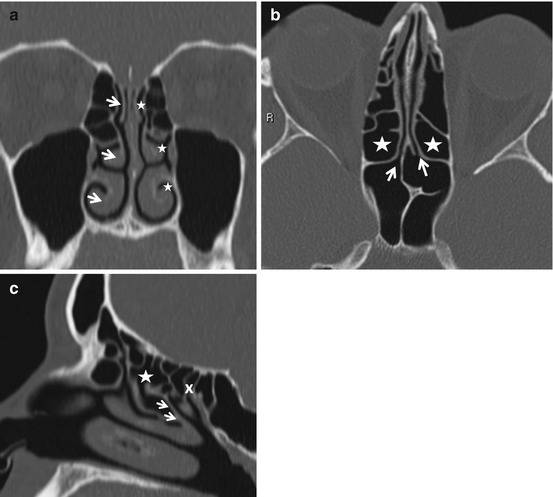
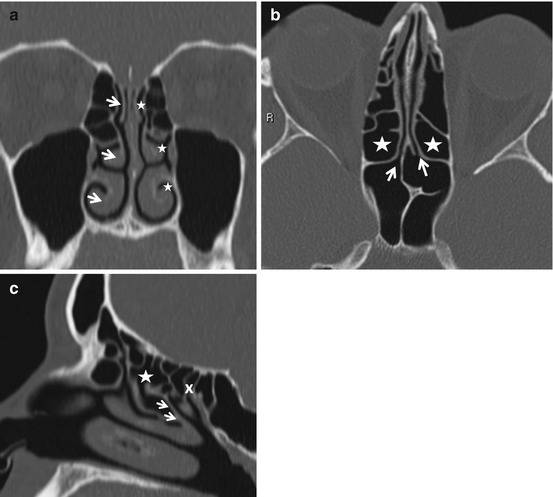
Fig. 9.1
(a) The 3 arrows point to the superior, middle, and inferior turbinates. The 3 asterisks indicate the corresponding meati. (b) The arrows point to the ostia of the sphenoid sinus, which open into the sphenoethmoidal recesses. The asterisks indicate the posterior ethmoid air cells. (c) The arrows indicate the basal or ground lamella of the middle turbinate, which separates the anterior (asterisk) from the posterior ethmoid air cells (x)
The lateral nasal wall is comprised of two ostiomeatal units. The anterior ostiomeatal unit consists of the frontal sinus ostium, frontal recess, maxillary sinus ostium, infundibulum, and middle meatus. The posterior ostiomeatal unit is comprised of the sphenoid sinus ostium, sphenoethmoidal recess, and the superior meatus (Fig. 9.1).
The uncinate process is a sickle-shaped sheet of bone arising from the lateral nasal wall and directed superiorly. Lateral to the superior free edge is the infundibulum. The ethmoid bulla is the largest anterior ethmoid air cell. Its medial wall forms the lateral wall of the infundibulum. The infundibulum is the air passage bounded medially by the uncinate process and laterally by the ethmoid bulla; it connects the maxillary sinus ostium to the middle meatus. The hiatus semilunaris is the crescentic gap between the free edge of the uncinate process and the ethmoid bulla (Fig. 9.2).


Fig. 9.2
The curved dashed arrow represents the infundibulum. Its medial opening is the hiatus semilunaris. It is bounded by the uncinate process (arrow) medially and the bulla ethmoidalis (asterisk) laterally
The frontal recess is the funnel-like drainage pathway of the frontal sinus. The term “frontonasal duct” is now avoided as no discrete ductal structure exists. The frontal recess drains into the anterior part of the middle meatus and may be divided into a superior compartment that lies below the frontal sinus ostium in the floor of the sinus and an inferior compartment which either opens into the infundibulum (if the uncinate process is directed towards the skull base) or continues into the middle meatus (if the uncinate process is attached to the lamina papyracea) (Fig. 9.3).
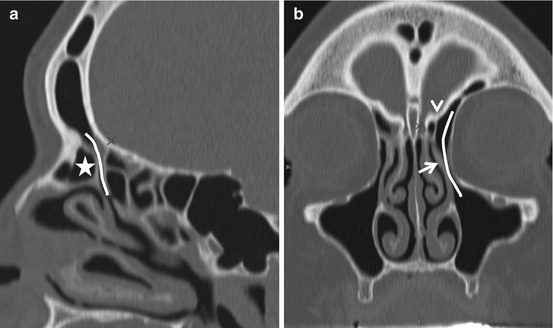
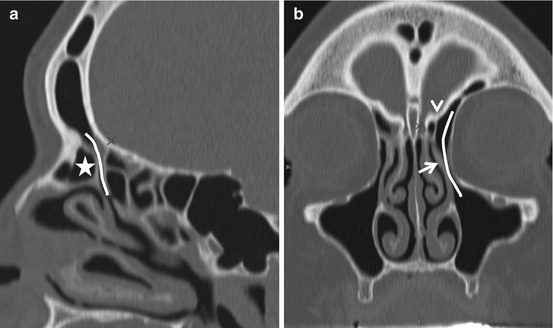
Fig. 9.3
The frontal sinus drainage pathway. The curved lines represent the frontal recess. An agger nasi (asterisk) cell is seen anterior to the frontal recess in (a). In (b), note that the uncinate process (arrow) is attached superiorly to the fovea ethmoidalis (arrowhead). This results in the frontal recess opening into the infundibulum
The fovea ethmoidalis is the roof of the ethmoid cavity. The cribriform plates are the portion of the ethmoid bone that forms the roof of the nasal cavity medial to the fovea ethmoidalis. They are perforated by the foramina of the olfactory nerves. The crista galli is a vertically oriented midline ridge of bone arising from the cribriform plates and attaching to the falx cerebri (Fig. 9.4). The anterior and posterior ethmoid air cells are separated by the basal lamella of the middle turbinate. The lamina papyracea is the gracile medial wall of the orbit. The agger nasi designates the most anterior ethmoid cells that form due to pneumatization into the lacrimal bone and the frontal process of the maxillae. They may be anterior, inferior, or posterolateral to the frontal recess and may encroach upon it (Fig. 9.3).
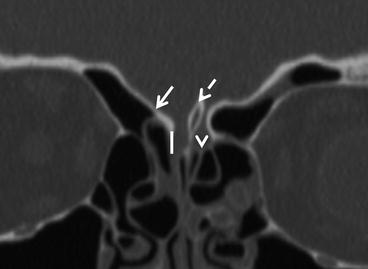
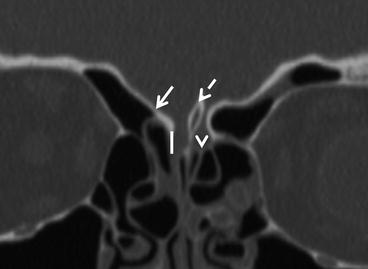
Fig. 9.4
Roof of the nasal cavity. The arrow points to the fovea ethmoidalis and the arrowhead to the cribriform plate. The vertical line represents the depth of the floor of the anterior fossa. The Keros system classifies this as type 1 where the depth is 1–3 mm, type 2 where the depth is 4–7 mm, and type 3 where the depth is between 8 and 11 mm. The greater the depth, the greater the potential for injury during endoscopic surgery. The cribriform plates may be dehiscent, as is the case on the right. The dashed arrow indicates the crista galli, to which the falx cerebri is attached. Occasionally the crista may be pneumatized and rarely contain a mucocele
The sphenoethmoidal recess is the site of drainage of the sphenoid and posterior ethmoid air cells (Fig. 9.1).
A summary of sinus drainage is provided in Box 9.1.
Box 9.1. Paranasal Sinus Drainage
Frontal sinus | Through frontal recess into middle meatus |
Anterior ethmoid cells | Middle meatus, mainly into infundibulum |
Posterior ethmoid cells | Sphenoethmoidal recess (superior meatus) |
Maxillary sinus | Through infundibulum into middle meatus |
Sphenoid sinus | Sphenoethmoidal recess (superior meatus) |
9.1.3 Anatomic Variations of Clinical Importance
The commoner anatomic variations are listed in Box 9.2.
The nasal septum is deviated in 25–30 % of the population. Marked deviation, especially with an osteocartilaginous spur, may compromise the middle meatus and predispose to recurrent sinonasal inflammation/infection (Fig. 9.5).


Fig. 9.5
Nasal septal deviation. Septal deviation may predispose one to recurrent sinus inflammatory disease. The sharp leftward deviation in this case has resulted in hypoplasia of the middle turbinate and uncinate process and consequently a narrow infundibulum
The middle turbinate may be completely pneumatized (concha bullosa) or pneumatized only within its vertical portion (lamellar concha or intralamellar air cell). Concha bullosae may become inflamed and rarely transform into a mucocele. In addition to conchae, paradoxically curved middle turbinates may also crowd the middle meatus leading to maxillary sinus obstruction (Fig. 9.6).
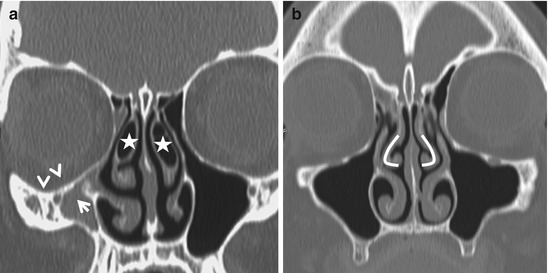
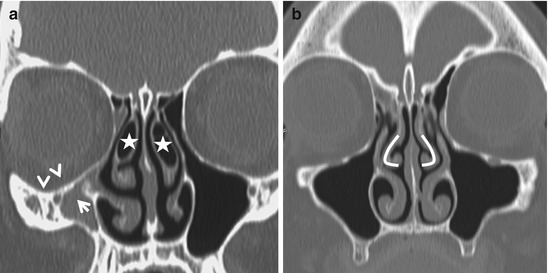
Fig. 9.6
(a) Concha bullosa. Pneumatization of the middle turbinates (concha bullosa, asterisks) is a fairly common anatomic variation and when substantial, can narrow the middle meatus. In (a), note that the right uncinate process (arrow) is deviated laterally (atelectatic) closing off the infundibulum, resulting in an obstructed, hypoplastic maxillary antrum. The right orbital floor has descended (arrowheads) and is at risk for injury during surgery. When accompanied by enophthalmos, this entity is referred to as the silent sinus syndrome. In (b), note that the convexity of the middle turbinates is directed laterally (curved lines) rather than towards the midline (paradoxical curvature). This can theoretically compromise the middle meatus
The free edge of the uncinate process may attach to the lamina papyracea (atelectatic uncinate) resulting in a chronically obstructed maxillary sinus ostium and hypoplasia of the maxillary sinus with associated descent of the orbital floor (silent sinus syndrome) (Fig. 9.7). If not recognized preoperatively, the plunging roof of the maxillary sinus may be inadvertently breached by the surgeon. The uncinate process may attach superiorly to the fovea ethmoidalis, in which case excessive traction during surgery may result in violation of the anterior cranial fossa and a CSF leak. The uncinate process may also be pneumatized (uncinate bulla), which encroaches upon the infundibulum and impedes frontal and anterior ethmoid sinus drainage (Fig. 9.7).
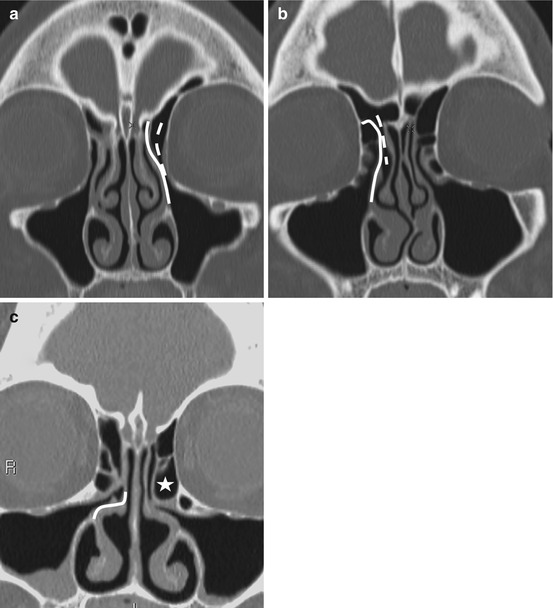
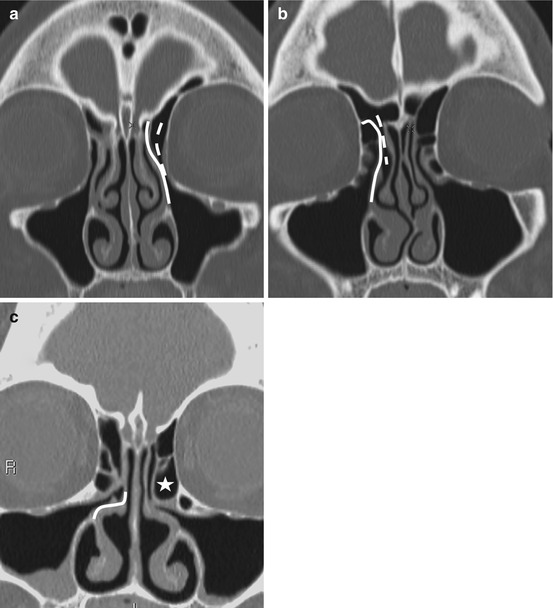
Fig. 9.7
Variations in uncinate process (UP) attachment. In (a), the uncinate process is attached superiorly to the fovea ethmoidalis (continuous line), resulting in the frontal recess opening into the infundibulum (dashed line). This configuration means that infundibular obstruction can result in simultaneous disease in the frontal, maxillary, and anterior ethmoid air cells. In (b), the UP is attached to the lamina papyracea (continuous line), resulting in the frontal recess (dashed line) draining into the middle meatus. This implies that the frontal and anterior ethmoid sinus drainage pathways are separated. Also, traction upon the UP during surgery may result in injury to the delicate lamina. In (c), the continuous line indicates attachment of the UP to the middle turbinate. The asterisk indicates a large ethmoid bulla, likely the cause of the UP being rotated medially
A giant ethmoid bulla is an unusually large ethmoidal bulla that compromises the infundibulum (Fig. 9.7).
Haller cells are infraorbital ethmoidal air cells. They may narrow the infundibulum and predispose patients to recurrent maxillary sinusitis (Fig. 9.8).
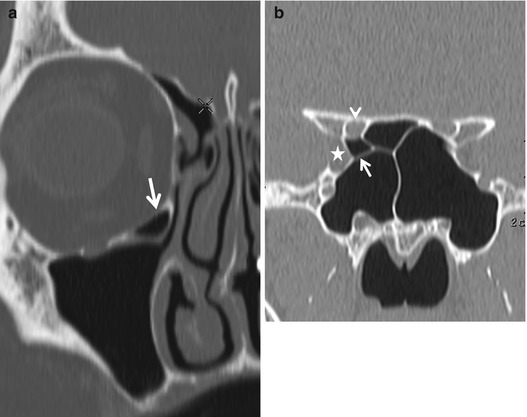
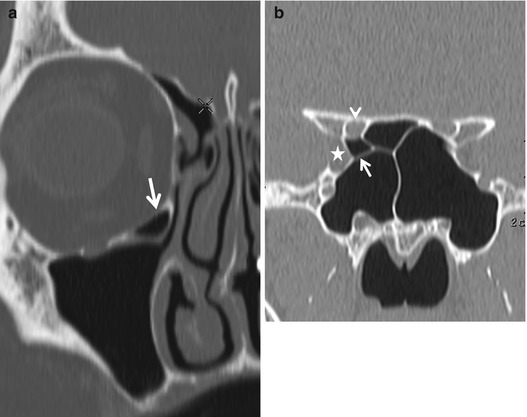
Fig. 9.8
(a) A Haller cell (arrow) represents an infraorbital ethmoid air cell and can compromise the infundibulum. (b) Onodi cells (arrow) result from posterior ethmoid pneumatization extending superior and lateral to the sphenoid sinus. These cells lie in close proximity to the optic nerves and occasionally, the internal carotid arteries, structures that may be injured if these cells are violated. Infection in an Onodi cell may also spread to the orbital apex rapidly. The arrowhead points to the optic canal and the asterisk indicated the superior orbital fissure
Onodi cells are the most posterior ethmoid air cells and are intimately related to the optic canal; they can completely surround the optic nerve, increasing the risk of optic nerve injury at surgery. Onodi cell mucoceles may compress the optic nerve (Fig. 9.8).
The sphenoid sinus is usually divided by a single sagittal septum, but multiple septa may be present. Sphenoid septa that insert laterally adjacent to the cavernous internal carotid artery may be associated with arterial injury at surgery. Pneumatization of the sphenoid sinus may extend into the anterior clinoid process and the horizontal carotid canals conferring increased risk of surgical injury to the optic nerves and internal carotid arteries, respectively. The lateral sphenoid sinus walls are occasionally dehiscent allowing the optic nerves and internal carotid arteries to pass through the sinus (Fig. 9.9).
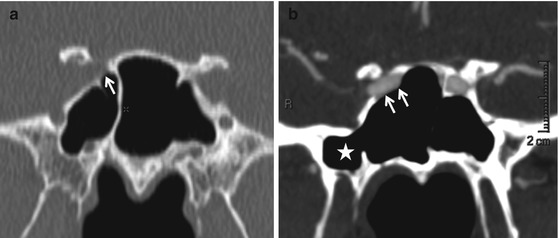
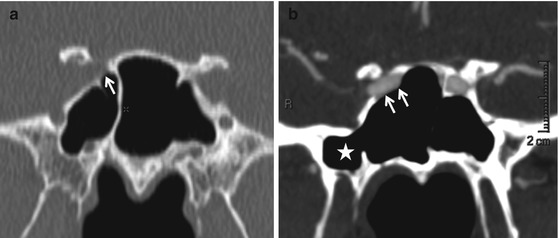
Fig. 9.9
The wall of the sphenoid sinus adjacent to the internal carotid arteries may be variable in thickness. In these images, there is no bony separation between the right ICA and the sinus cavity (arrows, a and b). In (b), note that pneumatization of the sphenoid sinus extends to the root of the pterygoid process (asterisk, pterygoid recess). A pterygoid recess may be the site of mucocele formation. Also, the greater sphenoid wing overlying, it can be thin enough to permit a CSF leak in some patients
Box 9.2. Anatomic Variations
Nasal septal deviation |
Middle turbinate |
Paradoxical curvature |
Concha bullosa |
Uncinate process |
Pneumatization (uncinate bulla) |
Variable attachment of free edge to lamina papyracea (atelectatic)/fovea ethmoidalis |
Giant ethmoid bulla |
Lamina papyracea dehiscence |
Variations in ethmoid pneumatization |
Haller cells |
Onodi cells |
Supraorbital cells |
Frontal cells |
Agger nasi cells |
Accessory maxillary sinus ostia |
Cribriform plates |
Variability in depth |
Dehiscence |
Sphenoid sinus |
Attachment of septum to lateral wall adjacent to the ICA |
Lateral wall dehiscence |
Anterior clinoid process pneumatization |
9.1.4 Physiology
The nasal cycle is a normal, cyclical side-to-side alteration in nasal airway resistance. It can be associated with mucosal hypertrophy, which is detectable on CT and MR imaging, especially around the inferior turbinate; this must not be mistaken for pathology (Fig. 9.10).


Fig. 9.10
Alternating physiologic congestion and decongestion of the mucosa of the nasal cavity is known as the nasal cycle. Note that the mucosa of the right inferior turbinate is more prominent than on the left on this T2-weighted MR image. This must not be misconstrued as pathology
9.2 Imaging Evaluation
Inflammatory sinonasal disease is evaluated most effectively by CT. Contrast is not usually required, except when spread of infection or inflammation beyond the sinonasal cavities into the orbits or adjacent soft tissues is suspected.
For effective evaluation using MRI, precontrast T1-weighted images must be obtained without fat suppression. The intrinsic T1 hyperintensity of fat provides a useful contrast against which low T1 signal intensity disease processes are easily seen. Fat suppression is useful on postcontrast T1-weighted sequences and enables the detection of enhancing abnormalities against a background of low fat signal. MRI is best used in mapping the extent of neoplasms and in the evaluation of intracranial spread of infectious diseases.
Plain radiography in the evaluation of sinonasal disease plays a minor role. One may rarely encounter a Waters’ view of the paranasal sinuses, obtained to demonstrate the presence of fluid/fluid levels in the setting of acute sinusitis. Plain films may also be used to evaluate nasal bone fractures, but ideally these are diagnosed clinically. Catheter angiography is best utilized for preoperative embolization of vascular sinonasal lesions such as juvenile nasopharyngeal angiofibromas and in the treatment of epistaxis.
9.3 Inflammatory Sinonasal Disease
9.3.1 Acute Inflammation and Its Complications
Acute inflammation of the sinuses may occur due to viral, bacterial, fungal, or allergic causes. A classic radiographic sign of acute sinusitis is a fluid level, but fluid levels may also be seen in a setting of trauma, prolonged nasogastric intubation, barotrauma, or CSF leak (Fig. 9.11). The presence of frothy secretions in a sinus may also indicate acute inflammation. Given the tendency of acute frontal and sphenoid sinusitis to progress to life-threatening complications, it is imperative that the clinician be alerted to fluid levels in these areas. Acute sinusitis may also manifest as thickened mucosa on CT. The signs of early acute fungal sinusitis may be subtle and are discussed below.
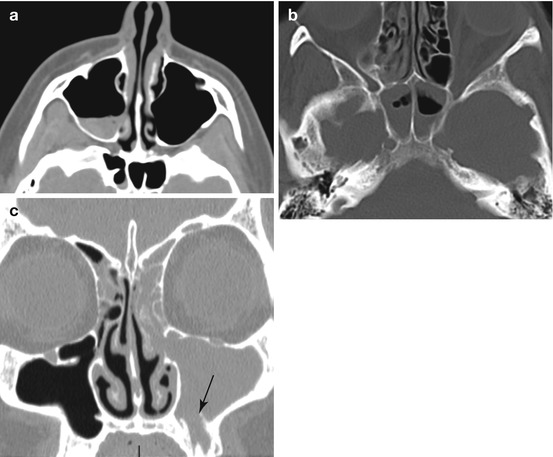
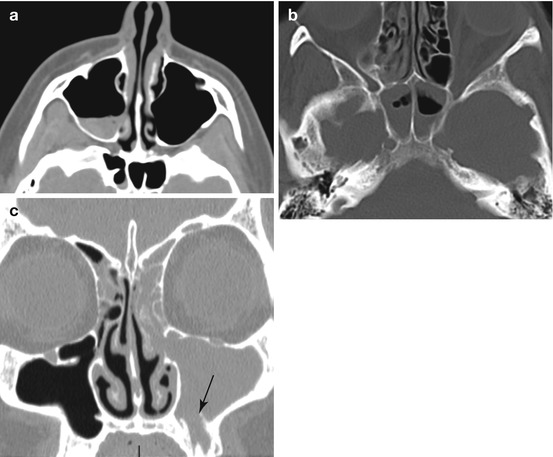
Fig. 9.11
Acute sinusitis. Fluid levels, in the appropriate clinical setting, indicate acute sinusitis (a, b). In a patient with acute maxillary sinusitis, it is always useful to evaluate the upper teeth. When periodontal disease occurs in a maxillary tooth whose roots project into the antrum, odontogenic sinusitis may occur (c, arrow)
Complications of acute sinusitis may involve the orbits or cranial cavity (Box 9.3). The orbits are most likely to be affected by ethmoid sinusitis. The lamina papyracea is a poor barrier to the spread of infection. The absence of valves in the anterior and posterior ethmoid veins also permits free spread of infection into the orbits. An extensive intradiploic anastomotic venous network allows spread of infection between the frontal sinuses and the meninges.
Orbital complications follow a loosely defined sequence of events (Fig. 9.12). Preseptal cellulitis (stage I) is manifested on CT by thickening and enhancement of the eyelid soft tissues; this can, however, be the consequence of simple transudative edema from impaired sinus venous outflow. At this stage, inflammation is restricted from posterior spread by the orbital septum. With orbital (postseptal) cellulitis (stage II), the intra- and extraconal fat demonstrates increased attenuation and stranding. The presence of a lentiform peripherally enhancing collection, applied to the lamina papyracea or orbital plate of the frontal bone and confined by the periorbita, indicates a subperiosteal abscess (stage III). A similar collection within the orbit itself indicates an orbital abscess (stage IV). Left untreated, this progresses to thrombophlebitis of the superior and inferior ophthalmic veins and then of the cavernous sinus itself (stage V). Enlargement and lack of enhancement of these venous structures, a convex contour to the cavernous sinus, and extraocular muscle engorgement are signs of cavernous sinus thrombosis. While unenhanced MRI may show T1 hyperintense thrombus in the cavernous sinus, contrast-enhanced CT or MRI is the best imaging modality to evaluate this entity. MR venography is usually insensitive to cavernous sinus thrombosis as the normal cavernous sinuses themselves are not well seen.
Get Clinical Tree app for offline access
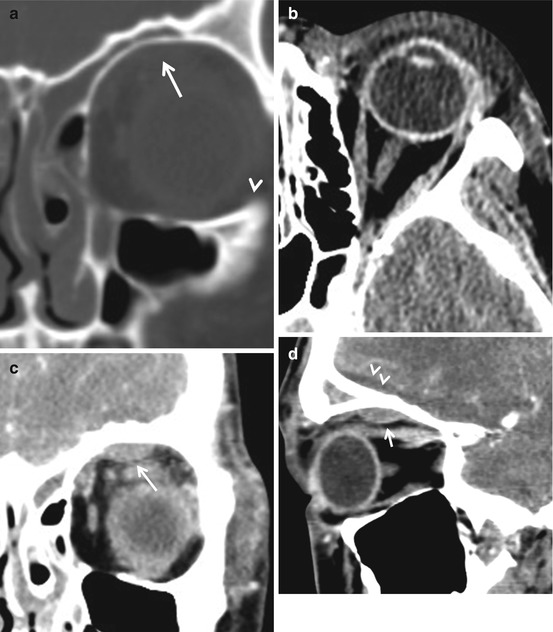
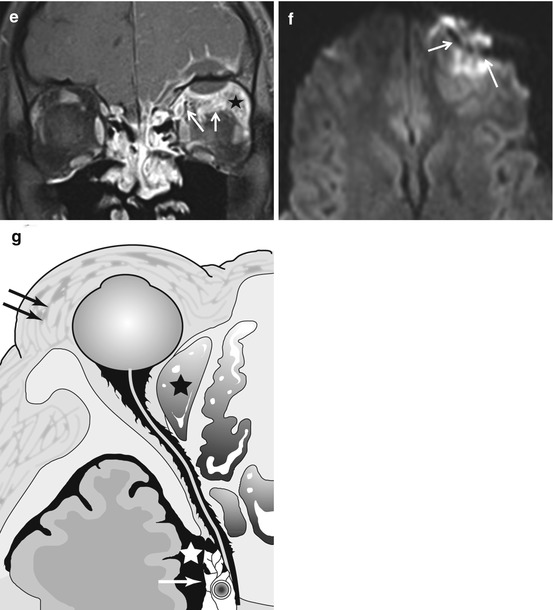
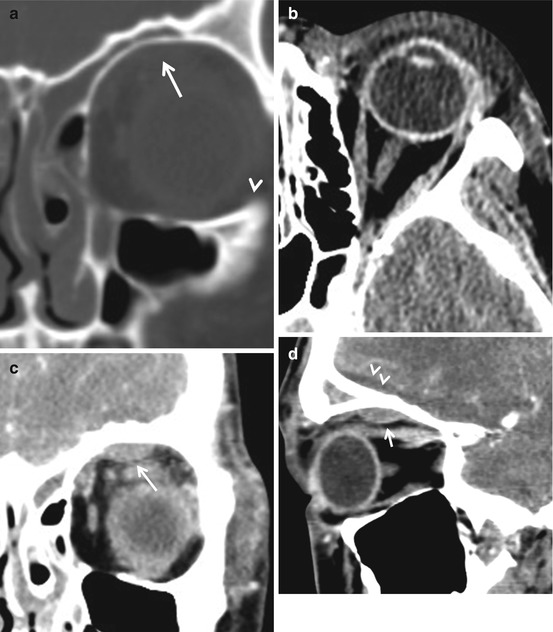
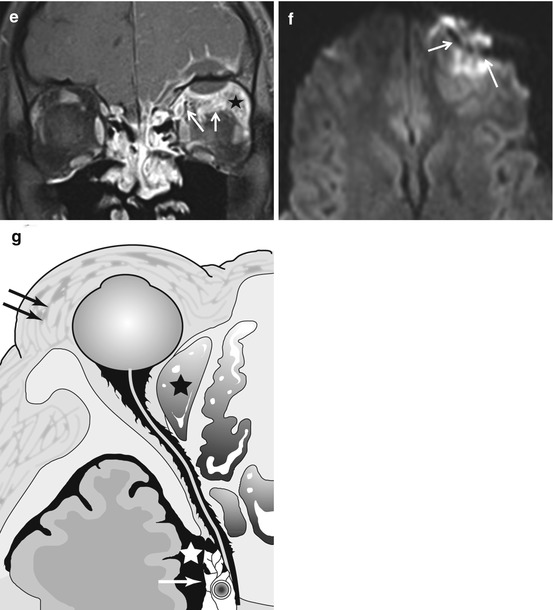
Fig. 9.12
(a) Orbital complications of acute frontal and ethmoid sinusitis. Image (a) shows fluid in the frontal and ethmoid air cells. In (b), edema of the preseptal soft tissues (arrows) is evident. The white lines roughly indicate the plane of the orbital septum, a fibrous sheet that is an effective but not always reliable barrier to the spread of inflammation. In (c, d), a lentiform collection (arrows) with its base against the orbital roof representing a subperiosteal abscess is present. Also in (d), note a low-density epidural abscess (arrowheads) under the right frontal lobe. Inspecting CT images in narrow window settings may help detect subtle findings of intracranial complications. In (e), on this contrast-enhanced fat-suppressed MR image, the epidural abscess and the associated meningeal enhancement (arrowhead) are obvious. Also, note the stranding and enhancement of the orbital fat (asterisk) indicating cellulitis and thickening and enhancement of the superior rectus and oblique muscles representing myositis (arrows). Diffusion-weighted images are very useful in demonstrating intracranial purulence (arrows, f). The graphic, (g), illustrates the various complications that may follow acute bacterial sinusitis – preseptal cellulitis (double arrows




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree