Skeletal System Scintigraphy
David K. Shelton
Amir Kashefi
Technique
Musculoskeletal imaging studies performed with gamma cameras and Technetium-99m (Tc-99m) labeled diphosphonates are a staple of nuclear medicine. The bone scan is a map of osteoblastic activity that occurs in response to various benign and malignant conditions. It is an excellent complement to anatomic studies of the skeletal system but is usually far more sensitive in detecting bony abnormalities, such as osteomyelitis or bony metastatic disease. After injection, blood flow is required to deliver the radiopharmaceutical to the extracellular space around functioning osteoblasts. Within minutes, they begin to assemble labeled diphosphonates into the hydration shell of hydroxyapatite crystals as they are formed and modified. Osteoclastic function is not measured by this technique.
Radiopharmaceuticals. The primary radiopharmaceuticals used for skeletal scintigraphy have been technetium pyrophosphate and most recently the technetium-based diphosphonates, primarily Tc-99m-MDP. Being technetium-based, Tc-MDP has a half-life of 6 hours and an energy of 140 KeV (Table 54.1). The usual adult dose is 20 mCi intravenously; however, up to 30 mCi may be used in heavy patients or for better detail.
Fluorine-18 is a positron-emitting radionuclide used for PET bone scanning or PET/CT scanning. The usual dose given is 5 to 15 mCi intravenously and it has an energy of 511 KeV with a 110-minute half-life.
Two common radionuclides are used for internal radiotherapy of painful bony metastatic disease. Strontium-89 (Metastron®) is a pure beta emitter with an energy of 1.46 MeV and a 50.5-day half-life. It is given intravenously with a typical dose 2 to 4 mCi. Samarium-153 (Quadramet®) is a beta emitter with 0.81 MeV and has a gamma photon of 103 KeV, which can be used for imaging. The usual dose is 1 mCi/kg intravenously and it has a half-life of 1.9 days.
Biodistribution and Physiology. Tc-99m-MDP is administered intravenously and is delivered to the skeletal system on the basis of vascular distribution. Vigorous osteoblastic activity in the growth plates of juvenile skeletons, healing fractures, pathological conditions stimulating skeletal blood flow, and bone repair increase the bone labeling. The technetium agents are excreted by glomerular filtration from the kidneys. In a normal subject, 50% is excreted by 4 hours and up to 80% of the injected diphosphonate will be excreted by 24 hours. Normal renal function clears soft tissue activity thus improving the quality of bone images because of improved target to background ratios. Decreased renal function for any reason degrades image quality. Waiting 3 to 4 hours before delayed skeletal imaging is a compromise between radiotracer decay and the clearance of background activity around the skeleton. Three-phase and four-phase skeletal scintigraphy have proven clinically useful in determining the vascular nature of lesions as well as in separating soft tissue injury or infection such as cellulitis from a focal skeletal disease such as osteomyelitis. Phase one is the dynamically acquired arterial phase. Phase two is a set of static images, which can be acquired in multiple views, representing the blood pool and soft tissue phase. Phase three is acquired 3 to 4 hours later and represents the delayed skeletal uptake. Phase four can be acquired the following morning if better skeletal detail is needed, usually when the patient has poor renal function, such as in the diabetic foot.
The mechanism of Tc-MDP tracer localization is by chem-adsorption to the mineral phase of bone, primarily in the areas of increased osteogenic activity. The bladder is the critical organ for Tc-MDP with 2.6 rads per 20 mCi and the whole body radiation absorbed dose is 0.13 rads per 20 mCi. Strontium is a calcium analog and binds avidly to the hydroxyapatite crystals of bone. Fluorine-18 is a hydroxyl ion analog, which also binds to the hydroxyapatite crystals in bone.
F-18-FDG is a glucose analog radiopharmaceutical, which is a tumor avid agent, also capable of identifying malignant tumors and bony metastatic disease.
Technical Issues. Skeletal scintigraphy has a resolution of about 5 mm in the best conditions. Adult IV doses of 20 mCi (740 mBq) or more for Tc-MDP are usually adequate for static imaging 3 to 4 hours after injection. Flow images are typically acquired in the anterior and posterior planes or as plantar/palmar views of the area in question. Blood pool images can be obtained in multiple views similar to “spot-view” images. Whole body delayed images are typically acquired in the anterior and posterior planes with oblique, lateral, or other spot views as required. The static “spot-views” usually have better resolution than the table-feed, whole body images. High-resolution, low-energy collimation is most commonly used for good quality images. Ultra-high-resolution collimation will produce a minor improvement in image quality but at the price of a geometric increase in imaging time. A pinhole collimator can be used to produce exquisite images of limited areas such
as the wrist. The completed bone scan should be interpreted “online” and tailored as necessary to answer the specific clinical question. SPECT imaging may be used for improved contrast resolution and better anatomic depiction in such areas as the spine, skull, knees, or ankles.
as the wrist. The completed bone scan should be interpreted “online” and tailored as necessary to answer the specific clinical question. SPECT imaging may be used for improved contrast resolution and better anatomic depiction in such areas as the spine, skull, knees, or ankles.
Table 54.1 Radionuclides Used in Skeletal Scintigraphy | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
More importantly, combining SPECT with CT not only has improved correction for attenuation in single-photon emission tomography but also has improved accuracy in identifying the anatomical site and extent of disease. These dual advantages of this hybrid equipment have further enhanced specificity and accuracy of diagnostic nuclear medicine.
The potential benefits of SPECT/CT stem from the ability to correct attenuation based on individual patient-based tissue density, to perform iterative reconstruction, and to display three planes (transaxial, coronal, sagittal) and 3-D images including maximum intensity projection (MIP) and
surface volume rendering. These abilities, as well as important socioeconomic considerations and irreplaceability of some of the single-photon emitting agents with PET tracers, have helped SPECT/CT survive the challenges from PET imaging, considering the advantages of PET imaging compared with single-photon imaging. Therefore, newer and more accurate single-photon radionuclide imaging procedures (such as new SPECT devices with CdTe/CdZnTe semiconductors instead of the classic NaI(Tl) scintillation crystals) are developing, in competition with many innovative PET applications.
surface volume rendering. These abilities, as well as important socioeconomic considerations and irreplaceability of some of the single-photon emitting agents with PET tracers, have helped SPECT/CT survive the challenges from PET imaging, considering the advantages of PET imaging compared with single-photon imaging. Therefore, newer and more accurate single-photon radionuclide imaging procedures (such as new SPECT devices with CdTe/CdZnTe semiconductors instead of the classic NaI(Tl) scintillation crystals) are developing, in competition with many innovative PET applications.
On the other hand, the radiation burden of the CT component of the SPECT/CT ranges from 0.3 to 1.5 mSv and is considerably lower than the dose delivered by diagnostic CT (2.1 to 3.1 mSv). Several studies have compared the efficacy of SPECT and SPECT/CT in differentiating benign from malignant bone disease and have found SPECT/CT to be helpful in reaching a definite diagnosis in 85% to 90% of lesions considered equivocal on SPECT or planar bone scintigraphy. SPECT/CT has also improved diagnostic confidence of the reviewers, which should reduce the need for further diagnostic imaging. For the patient, SPECT/CT can reduce time to treatment and the anxiety of an unknown diagnosis.
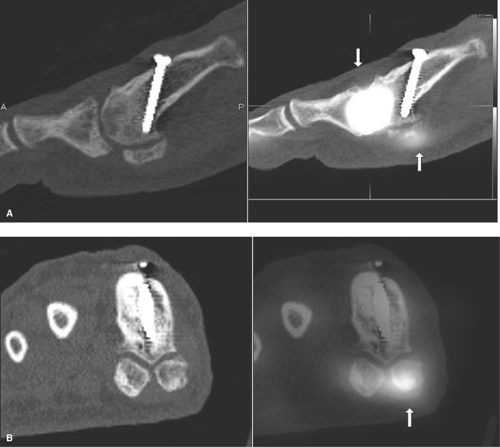
The clinical benefits of SPECT/CT in benign orthopedic conditions are also promising. Adding the low-dose multislice CT to SPECT has been found critical to correctly diagnose 59% of the lesions in nononcological patients with inconclusive 99m Tc-MDP bone scans (Fig. 54.1). In patients without cancer who had pain in the extremities and were investigated with both three-phase bone scintigraphy and SPECT/CT, the SPECT/CT findings led to revision of the diagnostic category in 32% of patients.
Interpretation
Normal Skeletal Scintigram. In the normal adult, skeletal tracer uptake is fairly uniform and symmetrical. Uptake is greater in the axial skeleton (pelvis, spine) than in the appendicular skeleton (skull and extremities). Mild, uniform soft tissue uptake is noted in the background. The kidneys should be slightly hotter than the soft tissues and should be symmetrical and normal anatomically. The renal collecting system, ureters, and bladder activity appear very intense. Children will demonstrate intense, symmetrical activity in their growth plates, which need to be evaluated carefully, preferably on the workstation.
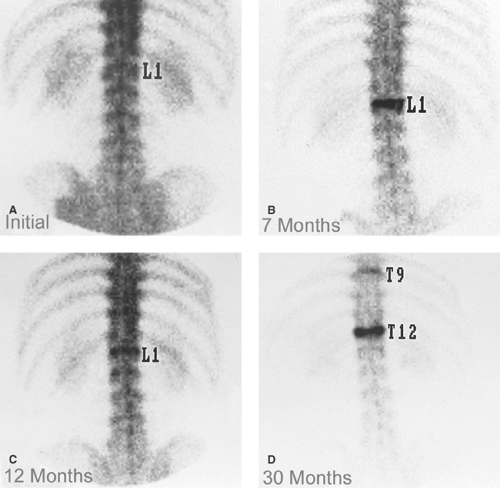
Trauma to the skeleton may be undetectable on standard radiographic examinations. The classic stress fracture may be caused by overuse of the normal skeleton or an insufficiency fracture may result from normal use of weakened bone. Scintigraphically demonstrated trauma precedes radiographically detectable fracture healing by approximately 10 days. Decreased or normal osteoblastic activity is seen at the fracture site in this first phase of repair. The subsequent osteoblastic activity then shows as a “hot spot,” weeks before the calcified callus appears on a radiograph (Figs. 54.2, 54.3). In an uncomplicated fracture, repaired bone returns to normal appearance as the callus at the fracture site remodels over a period of months (Fig. 54.4). A complicated fracture in a weight-bearing bone, healing with angulation, may take many years to return to normal bone scan activity. Some fractures may show remodeling on bone scans for life. Bone scans or SPECT of the spine is frequently useful in osteoporotic vertebral fractures, prior to vertebroplasty. The scan evaluates for a metastatic pattern and for the acuteness and level of the fracture.
The three-phase bone scan can accurately diagnose shin splints and discriminate them from the more serious stress fracture. Shin splints demonstrate superficial, vertically oriented uptake in the tibia, usually posteromedially. Stress fractures are more localized and run horizontally. Recent studies have shown that pinhole bone scan is more sensitive than plain film or CT for scaphoid and other fractures of the wrist. Whole body bone scans are useful in detecting unsuspected fractures, following severe cases of multitrauma.
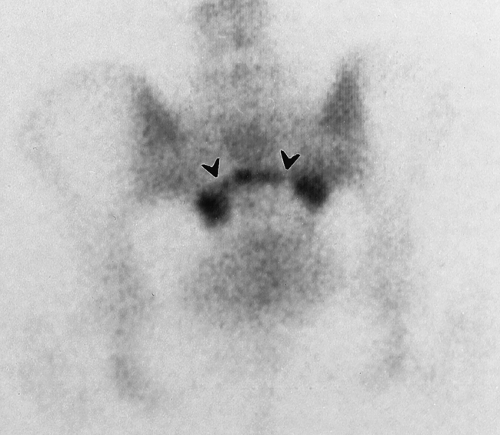
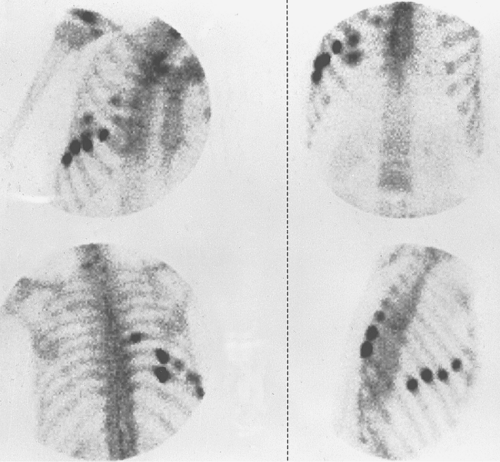 Figure 54.2. Multiple Rib Fractures. Vigorous osteoblastic repair activity is seen in two rows of fractures, which were not visible on radiographs. Note the “linear array” distribution not seen with the metastases in scans of Figures 54.13 and 54.14. |
Prosthetic joint replacements may loosen and/or become infected. For about 6 months after hip replacement surgery, the bone around the prosthesis is expected to have increased osteoblastic activity. Thereafter, increased labeling correlates with infection, loosening, and heterotopic bone formation, depending upon the pattern of localization. The toggle sign is indicative of prosthetic loosening and refers to a hot spot at
the tip of a prosthesis and two areas of increased uptake at the proximal end, like a toggle switch. Radiographs and occasionally radiolabeled white blood cell scans may be required to further diagnose abnormal findings (Fig. 54.5).
the tip of a prosthesis and two areas of increased uptake at the proximal end, like a toggle switch. Radiographs and occasionally radiolabeled white blood cell scans may be required to further diagnose abnormal findings (Fig. 54.5).
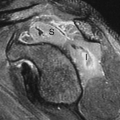
Arthropathies and Arthritides. Inflammation of a joint creates increased blood flow and increases radiopharmaceutical supplied to those portions of the bone bounded by the synovial capsule. Increased bone labeling is seen in toxic synovitis, septic joints, inflammation associated with early degenerative conditions, and connective tissue arthropathies. In early osteoarthropathy, high-resolution bone scan images detect increased subchondral bone labeling long before there are radiographic findings. Intense, abnormal labeling is also seen in neuropathic joints long before the abnormality is detected by radiographs (Fig. 54.6).
Osteomyelitis. In a large bone such as a tibia, acute hematogenous infection of bone that precedes radiographic abnormality can be sensitively and specifically diagnosed by three-phase bone scans. Early arterial flow seen seconds after injection (first phase), increased blood pool (second phase) seen for a few minutes before bone labeling begins, and intense delayed labeling 3 or more hours after injection (third phase) are characteristic of early infection. This phenomenon requires several days of symptoms before it develops. Radiographic changes may not be seen for 10 to 14 days. The scan is more difficult to read and not as specific when the target is small (like the bones of the foot) in comparison with the resolving power of the camera (Figs. 54.7, 54.8). False-negative examinations have been reported in children when the duration of clinical illness is brief.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree