Clinical Indications
Clinical Indications
Primary Diagnosis
• Benign nonvascular tumors
• Benign vascular tumors
• Malignant tumors
• Vascular lesions
• Articular and periarticular lesions
• Inflammatory and infectious lesions
• Exogenous skin components
• Nail lesions
Ancillary Diagnosis: Determination of Disease Extension, Activity, or Response to Treatment
• Hemangiomas
• Morpheas
• Plantar warts
• Basal cell carcinoma
Therapeutics: Presurgical Definition of Lesional Anatomy
• Involvement of extralesional tissue structures
• Characterization of lesional and perilesional blood supply and hemodynamics
Limitations
The use of ultrasound in skin imaging requires a trained physician. The large heterogeneity of cutaneous lesions and the distortional effect introduced by uneven pressure from alterations in the compressibility of skin tissues complicates the imaging process. Moreover, lesions of solely epidermal localization, of flat subepidermal lesions, or measuring less than 0.1 mm can give normal ultrasound images (false-negatives). In these cases, ultrasound can help exclude concomitant pathologies, while providing anatomic information on the surrounding tissues. Calcium deposits, foreign bodies, and hair follicle fragments are easily defined on ultrasound, but cutaneous pigment deposits cannot be detected.
 Technical Guidelines
Technical Guidelines
The ultrasound examination starts with a thorough visual inspection of the lesion to determine the positional approach that would place the affected site closest to the operator. Sedation is administered to children less than 4 years old (chloral hydrate, 50 mg/kg, orally, 30 minutes prior to the exam) to prevent artifacts in the color Doppler spectral curve analysis. Sedation recovery is monitored with a modification of the Aldrete test score.
A copious amount of gel is then applied to the affected skin to serve as a sound conductor, pressure distributor, and focusing agent, thus directing the probe to the most superficial layers of the skin.
Lesions are examined on the screen along all cross-sectional axes (longitudinal, transverse, and oblique), and described with regard to shape, echogenicity, composition, location, and vascularity. Relevant details of the surrounding tissues, including the presence and location of feeding and surrounding vessels are also noted.
To magnify the contrast between lesional and extralesional structures, it may be helpful to perform comparative evaluations examining the contralateral side or different areas in the same corporal segment. Compression maneuvers may help define venous vessels or free-fluid collections.
 Normal Anatomy
Normal Anatomy
The skin layers can be defined on ultrasound as clearly separated structures: the epidermis appears as a fine hyperechoic line, except in the palm of the hands and sole ofthe feet where it is thicker and bilaminar. The dermis shows a hyperechoic band of variable thickness, produced by the dense collagen content, which is thicker in the dorsal area and thinner in the ventral forearm. The subcutaneous tissue (hypodermis) contains hypoechoic fat lobules separated by hyperechoic fibrous septa (Fig. 9.1)
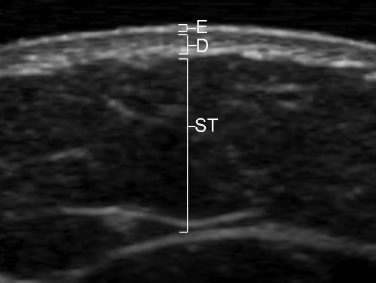
Fig. 9.1 Sonographic anatomy of the skin. E, epidermis; D, dermis; ST, subcutaneous tissue.
The nail unit comprises a hypoechoic nail bed that changes proximally to hyperechoic at the junction where the underlying dermis defines the hypoechoic matrix. The dorsal and ventral plates appear as a bilaminar parallel hyperechoic structure with a narrow, almost virtual space between the plates. The bone margin of the distal phalanx is also visibleas a hyperechoic line (Fig. 9.2).
Low-flow vessels, venous or arterial, may be detected in the subcutaneous tissue and within the nail bed.
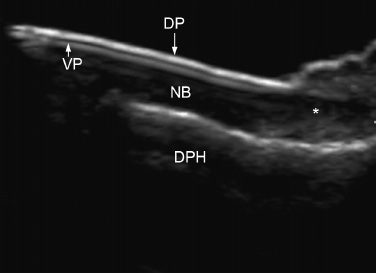
Fig. 9.2 Sonographic anatomy of the nail unit. DP, dorsal plate; VP, ventral plate; NB, nail bed; (*), matrix; DPH, bone margin of the distal phalanx.
Benign Tumors
Skin Cysts
Skin cysts, particularly epidermal, trichilemmal, or pilonidal cysts represent one of the most common requests for ultrasound skin examination. All these cystic lesions are located in the dermis and superficial subcutaneous tissue and present as a cosmetic problem, or as inflammatory lesions containing clear fluid, pus, or cheesy material. On ultrasound, skin cysts vary in their appearance depending on the density of the keratinous component, or the presence of inflammation or wall rupture. Noninflamed cystic lesions are round or oval, with well-defined anechoic or hypoechoic content that may contain hyperechoic hair follicle fragments or calcium deposits. In contrast, in the inflammatory stages or after wall rupture, the lesion outline becomes ill defined with a heterogeneous echo pattern and increased blood vessel signals in the periphery. In these cases, the detection of a posterior acoustic enhancement artifact can help identify the cystic origin of the lesion.
Epidermal cysts, sometimes called sebaceous cysts, originate in the infundibular portion of the hair follicle. They are not related to the sebaceous glands; hence, a “sebaceous cyst” is a misnomer. Epidermal cysts can be congenital or the result of previous trauma, including surgery. They can contain calcium deposits and/or a connecting tract to the skin surface clinically seen as a punctum. Histologically, these cysts are composed of a wall that contains squamous stratified epithelium with a granular layer and a center that contains keratin squames and fluid (Figs. 9.3 and 9.4).
Trichilemmal cysts originate in the external sheath of the hair follicle root; they generally do not have a connecting tract to the epidermis and are more common in areas with high hair density such as the scalp. Histologically, they are composed of a wall that contains epithelium without a granular layer and a center that contains fluid, keratin, cholesterol crystals, and sometimes calcium deposits (Fig. 9.5).
Pilonidal cysts are located in the intergluteal region. They are presumably related to the development of a sacral dimple that traps hair follicles; they may also be the result of repetitive local trauma. They frequently become inflamed and infected, with purulent matter discharging through a draining fistulous tract. Pilonidal cysts may be large structures; they usually present as hypoechoic fistulous tracts that become enlarged downward and contain multiple and large hyperechoic lines corresponding to a nest with hair follicle fragments (Fig. 9.6).
Lipomas
These are the most common soft tissue tumors and are composed of mature adipose cells. On ultrasound, they show variable echogenicity, most frequently hypoechogenicity, but a mixed pattern of hypo-/hyperechogenicity may also be seen. The lipomas may be oval or round and usually run parallel to the main axis of the skin, most often as single tumors, in the subcutaneous tissue, although in 5 to 15% of the cases they may appear as multiple tumors (Fig. 9.7).
Pilomatrixomas
Also called calcifying Malherbe epitheliomas, these tumors are derived from the hair matrix. They are most frequently found in children and young adults. Pilomatrixomas appear as single or multiple skin-colored or purplish lesions mainly in the head and neck. Sonographically, they are target round-shaped lesions located in the dermis and subcutaneous tissue composed by a hypoechoic rim corresponding to the tumor capsule that surrounds a hyperechoic center.
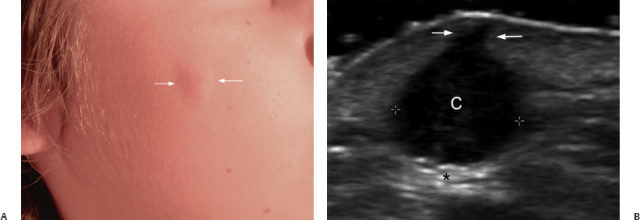
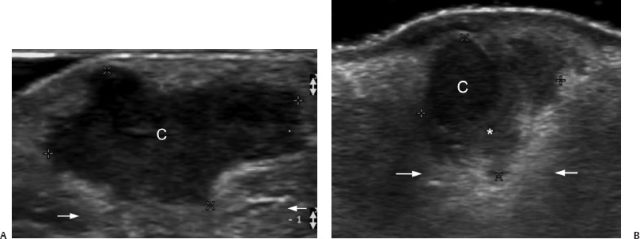
Fig. 9.3 Epidermal cyst. (A) Erythematous lesion in the cheek of a child (arrows). (B) Transverse view shows a round anechoic structure with inner echoes (between markers) in the dermis and upper subcuta neous tissue, and connected by a duct to the subepidermal zone (arrows). Posterior acoustic enhancement artifact is visible (*). C, cyst.
Fig. 9.4 Epidermal cyst complicated with inflammation. (A) Transverse view shows a hypoechoic structure of irregular shape (C) that corresponds with the epidermal cyst. A posterior acoustic enhancement artifact, seen in fluid-filled structures, is also present (arrows). (B) Transverse view shows a cyst with disruption of its capsule and inflammatory reaction to the keratinous component released to the surrounding tissue (*).The posterior acoustic enhancement artifact is still detectable under the cyst (arrows).
This center is composed of epithelial cells, and in 75% of the cases, of calcium deposits that appear as hyperechoic dots (Fig. 9.8).
Malignant Tumors
Skin cancer affects sun-exposed areas of the skin and is classified into nonmelanoma skin cancer (NMSC) and melanoma. NMSC, the most frequent tumors, include two subtypes: basal cell carcinoma (BCC) and squamous cell carcinoma (SCC).
Basal cell carcinoma is the most common cancer in humans; it is a slow-growing lesion affecting mostly individuals with light colored skin. They may be locally aggressive, but rarely metastasize. The most frequent location is the face; less often, the trunk and extremities. Several subtypes are recognized histologically: nodular, adenoid, and morpheaform, but clinically they have a common presentation as a round pearly nodule covered with telangiectasias, ulceration, and/or bleeding. Rare clinical presentations are as a bluish–gray cystic nodule or as a scarring plaque lesion. On ultrasound, BCCs appear as oval-shaped tumors of heterogeneous hypoechogenicity, with irregular contour and increased arterial vascularization deep within the tumor and at the periphery. Hyperechoic dots inside the tumor have been also described (Figs. 9.9 and 9.10).
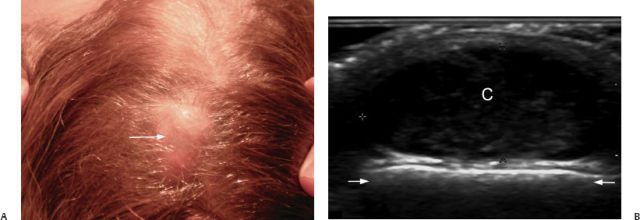
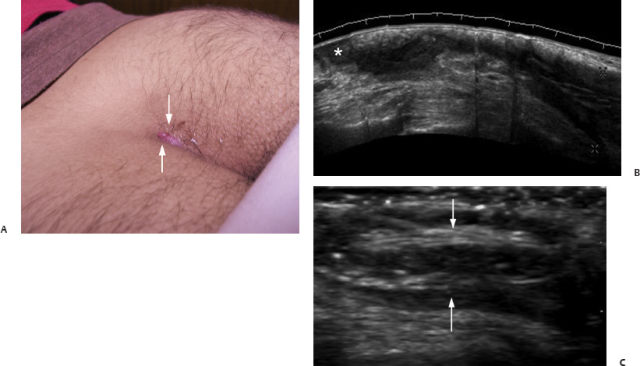
Fig. 9.5 Trichilemmal cyst in the scalp. (A) Clinically, there is an area of swelling and alopecia in the scalp (arrow). (B) Ultrasound (transverse view) in the scalp shows an anechoic cystic lesion (C, between markers) with echoes that correspond to the keratinous content. Posterior acoustic enhancement is clearly detectable (arrows).
Fig. 9.6 Pilonidal cyst. (A) Clinically, there is erythematous swelling in the intergluteal zone (arrows). (B) Panoramic longitudinal view of the intergluteal region shows an extensive fistulous tract that runs through the cutaneous layers and becomes wider in the sacral region (between markers). The clinical cutaneous lesion corresponds to only the upward part of the cyst (*). (C) Longitudinal view shows multiple hyperechoic lines inside the cyst that correspond to hair fragments (arrows) inside the cyst.
Squamous cell carcinoma is the second most common cancer of the skin and appears as crusted or scaly patches with a red inflamed base, as a growing nodule, or as a non-healing ulcer. On ultrasound, they are seen as slightly ir regular heterogeneous hypoechoic lesions, or as nodules extending to deeper structures. SCC has tumoral blood vessels on color Doppler that are more prominent than in BCC and also a higher recurrence rate (Fig. 9.11).
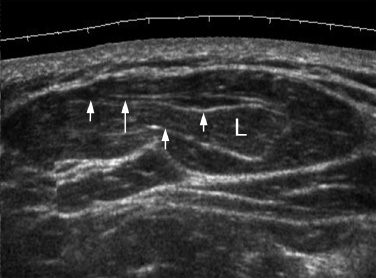
Fig. 9.7 Lipoma. Longitudinal panoramic view shows an oval hypoechoic structure (L) with hyperechoic fibrous septa (arrows) in the subcutaneous tissue that runs parallel to the skin layers’ axis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Pathologies
Pathologies