Solitary Pulmonary Nodules
Todd M. Blodgett, MD
Alex Ryan, MD
Carl Fuhrman, MD
Key Facts
Terminology
Solitary pulmonary nodule (SPN)
Opacity in the lung parenchyma measuring up to 3 cm with no associated mediastinal adenopathy or atelectasis
Imaging Findings
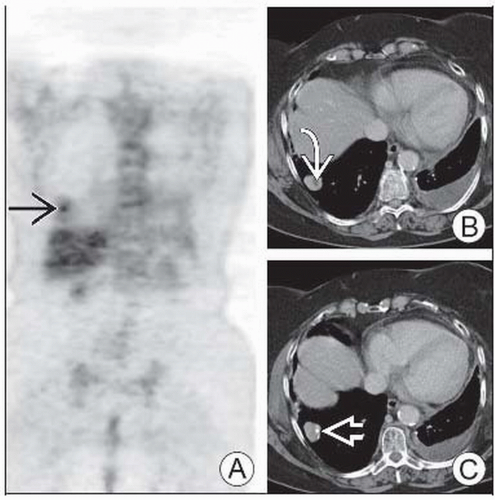
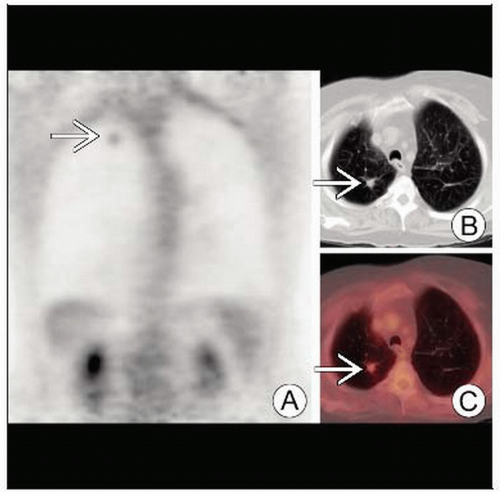
Risk of malignancy highest when nodule has SUV > 2.5 and spiculated morphology
PET/CT superior to CT or PET alone for overall accuracy
Nodules with internal calcifications generally benign
Central calcification is characteristic of benign nodules
Dual-time point imaging may be helpful in differentiating benign from malignant pulmonary nodules
Top Differential Diagnoses
Metastasis
Infection
Granulomatous Disease
Benign Lesions
Pulmonary Infarct
Pathology
Granuloma is the most common entity accounting for SPN
Diagnostic Checklist
Continued CT follow-up in PET-negative SPN
If nodule has features of BAC, a negative PET does not rule out malignancy
Predictive value of stability in size over time of a SPN is only 65%
TERMINOLOGY
Abbreviations and Synonyms
Solitary pulmonary nodule (SPN)
Bronchioloalveolar carcinoma (BAC)
Definitions
Opacity in the lung parenchyma measuring up to 3 cm
Usually no associated mediastinal adenopathy or atelectasis
IMAGING FINDINGS
General Features
Best diagnostic clue
High suspicion for malignancy
Any detectable FDG activity higher than background (> mediastinal blood pool) for SPN < 1.5 cm
SUV > 2.5 in any nodule
Spiculated morphology, particularly with a history of smoking
Low suspicion for malignancy
Round nodule with dense calcification and uniform morphology
FDG uptake equal to background activity
Location
No regional pattern for benign nodules
2/3 of primary lung tumors arise in upper lobes
SPN from extrapulmonary primary most often located in outer 1/3 of lower lobes
Size
Definition: Nodule < 3.0 cm < mass
Larger SPN more likely malignant
Over 85% are cancer when larger than 2.0 cm
Growth rate
26% increase in diameter corresponds to a doubling of the nodule’s volume
Time to 26% increase in diameter = one doubling time
Most cancer doubling times: ˜ 30-200 day range
Nodule dimension stability: > 2 years highly suggestive that nodule is benign
Increase in size seen within 30 days suggestive of infection, infarction, lymphoma, fast-growing metastases
Morphology
Benign characteristics
Margin: Well-circumscribed with smooth borders
Density: Fat or water density
Calcification: Common
Cavitation: Wall thickness < 5 mm
Enhancement: Usually minimal
Ground-glass opacity (suggests inflammation)
Air-fluid level (abscess)
Satellite nodules: Common in granulomatous lesions
Malignant characteristics
Margin: Irregular, lobulated, ill-defined with spiculated borders
Density: Soft tissue density
Calcification: 10% demonstrate calcification that is usually peripheral and stippled
Cavitation: Present in 80% of cavitary lung cancers (e.g., squamous cell carcinoma)
BAC may appear entirely as ground-glass opacity
Enhancement: More prominent
Spiculation highly specific for malignancy
Up to 20% of smooth nodules with sharp margins are malignant (e.g., carcinoid)
Air bronchogram: Present in 25-65% of cancers
Pseudocavitation: Common to malignancies such as BAC
Wall thickness > 1.5 cm strongly suggestive of malignancy
Imaging Recommendations
Best imaging tool: PET/CT demonstrates superior accuracy to CT or PET alone
Protocol advice
Dual-time point imaging may be helpful in differentiating benign from malignant pulmonary nodules
Malignant nodules gain intensity between hour 1 and hour 2
Benign nodules decrease in intensity
Radiographic Findings
Chest X-rays (CXR) helpful for determining time course of nodule development
Little change over 2 years or longer is strongly suggestive of a benign process
1-2 SPN detected per 1,000 CXR, routine screening radiographs
CXR has low sensitivity for detection of subcentimeter noncalcified nodules
CT Findings
Indications
Accurate localization of nodule (intra-/extrapulmonary)
Detection of additional unsuspected nodules
Characterization of margin, density, and calcification patterns
Assessment of extrapulmonary involvement (lymph nodes, pleura, chest wall, liver, adrenals, etc.)
Malignant morphology
CT may misclassify 25-40% of nodules as benign based on morphologic characteristics
BAC and lymphoma, for example, often appear benign
Coarse spiculation and bronchovascular bundle thickening around tumor
More common in presence of vessel invasion &/or lymph node metastasis
Heterogeneous internal composition
Hazy or indistinct margins
Peripheral spiculation with halo
Pleural retraction adjacent to tumor
Necrosis
Extension to bronchi or pulmonary veins
SPN calcification characteristics
Malignant
Generally not calcified
Nodules with eccentric calcification cannot be classified as benign
Bone cancer, soft tissue sarcoma, and mucinous adenocarcinoma metastases may calcify
1/3 of carcinoid tumors calcify
Colon and ovarian metastases may show psammomatous calcification
Internal hemorrhage may simulate calcification (melanoma and choriocarcinoma)
Benign
Central, laminated, popcorn, diffuse
Diffuse calcifications > 300 HU through nodule
> 1/2 granulomas are calcified
1/3 of hamartomas have popcorn calcification
Ground-glass opacity (GGO)
GGO nodules are lower density than solid nodules and do not obscure lung parenchyma
20% of lung nodules demonstrate this density
34% of these are malignant
More difficult to distinguish malignant from benign disease based on morphology
Much higher incidence of malignancy among ground-glass and mixed opacity nodules
Bronchoalveolar carcinoma often demonstrates this density
Also adenocarcinoma with BAC features
Adenocarcinoma > 2 cm with > 50% GGO has low risk of lymph node metastasis and vessel invasion
Enhancement
Malignant nodules often hypervascular and highly enhancing
Generally, > 25 HU = malignant, and < 15 HU = benign
Insensitive for subcentimeter, cavitary, or necrotic nodules
Fat
Malignant: Liposarcoma, renal cell carcinoma metastases (uncommon)
Benign: Hamartoma, lipoid pneumonia
Air bronchograms
Caused by small airway distortion
More typical of malignant than benign nodules
Seen in 30% of malignant nodules and 6% of benign nodules
As much as 55% of BAC shows bubble-like lucencies = pseudocavitation
Nuclear Medicine Findings
PET
Significant overlap in FDG activity between benign and malignant nodules
SUV > 2.5 has sensitivity/specificity 90-100%, 69-95% for detection of malignancy
Detection depends largely on size
Lower resolution limit 6-8 mm
Partial volume averaging of small nodules can produce falsely low SUV
Bronchioloalveolar carcinoma has multifocal form that is often detected with FDG PET
Overall, BAC tends to have lower FDG uptake than other pulmonary malignancies
False positives
Focal hypermetabolic uptake unrelated to malignancy
Most common include infection, inflammatory reaction, granulomata, hamartoma
False negatives
Malignant subcentimeter nodules may not be detected on FDG PET
Hypometabolic tumors: BAC, carcinoid
Temporary decrease in FDG uptake of active lesions post-therapy (“stunned tumor”)
Ground-glass nodules often false negative due to size and association with BAC
PET provides prognostic information for malignant nodules
May be more accurate than pathology in predicting recurrence-free survival
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree