Sonography plays an important role in the evaluation of patients who have thyroid carcinoma by identifying metastatic disease to the regional cervical lymph nodes. The sonographic appearance of lymph node metastases may vary from subtle alterations in echogenicity or vascular patterns to more obvious findings of calcifications and cystic changes within an affected node. Identification of metastatic disease to lateral cervical lymph nodes by sonography may affect the extent of surgical resection at the time of diagnosis. In patients who have had thyroidectomy for cancer, sonographic evaluation has proved to be the most sensitive imaging technique to detect thyroid cancer recurrence in the neck.
Sonographic evaluation of the neck plays an important role in the evaluation of patients who have thyroid carcinoma at the time of initial diagnosis and in the assessment of recurrent disease. Most patients diagnosed with differentiated thyroid cancer have lesions that are confined to the thyroid or are minimally invasive into the adjacent soft tissues of the neck, yet often these cancers have already metastasized to the regional cervical nodes. Sonography has been established as the most sensitive imaging test to diagnose these nodal metastases. Detection of metastatic cervical lymph nodes by sonography at the time of initial presentation may alter the surgical approach to include a modified lateral neck dissection at the time of thyroidectomy. Ultrasonography of the neck also offers an inexpensive and readily available means to detect recurrent thyroid cancer following thyroidectomy. Furthermore, when abnormalities are identified by neck sonography, they can be biopsied under direct sonographic visualization.
Anatomy
It is helpful for the imager evaluating the patient for metastatic thyroid cancer to have familiarity with the nomenclature used to describe the location of cervical nodes. The classic description of nodal location based on superficial anatomic landmarks has been replaced by imaging-based classifications. The cervical lymph node classification most widely used by clinicians who specialize in head and neck cancer is that established by The American Joint Committee on Cancer Staging and the American Academy of Otolaryngology–Head and Neck Surgery, which groups the cervical nodes by regions (levels) to more closely reflect the clinical staging of head and neck tumors. Level I refers to nodes in the submental and submandibular regions. Levels II, III, and IV refer to nodes along the anterior cervical and internal jugular chains. Level II encompasses those nodes from the base of the skull to the lower border of the hyoid bone, Level III from the hyoid to the lower margin of the cricoid cartilage, and level IV from the cricoid to the clavicle. Level V nodes are those in the posterior compartment of the neck, along the course of the spinal accessory nerve, and are divided into upper (VA) and lower (VB) levels by the cricoid cartilage. Level VI nodes, the paratracheal nodes, are in the visceral or central compartment of the neck. This compartment extends from the hyoid bone superiorly to the suprasternal notch inferiorly. On each side of the neck, the lateral border of the central neck compartment is formed by the medial border of the carotid sheath. Level VII nodes are in the superior mediastinum ( Fig. 1 ).

Technique
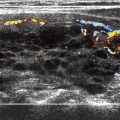
In general, higher-frequency, linear transducers offer the best spatial resolution, whereas lower frequencies give better tissue penetration of the emitted sound waves. Because the findings of metastatic thyroid cancer may be subtle, the examination should be performed with the highest frequency possible. The superficial neck nodes should be evaluated with a linear, high-frequency transducer of at least 7.5 MHz, preferably greater than 10 MHz. Evaluation of the deep lymph nodes of the neck and the superior mediastinal nodes may require a lower frequency (5 to 7.5 MHz), small footprint curvilinear or sector probe that allows deeper sound penetration and can be positioned in the narrow suprasternal notch. Transducers with color Doppler capability are also preferred because assessment of the vascularity of lymph nodes is often helpful in identifying metastatic disease.
The patient should be in a supine position, with a pillow or rolled towel under the upper back to allow maximal extension of the neck. This technique is particularly important to examine the lower level IV and level VI nodes and the upper mediastinum. The examination should be systematic, imaging all the lymph node levels in the transverse plane. The longitudinal plane should also be used to examine levels II through V. Gray-scale sonography is used to identify the size, shape, and nodal architecture. Color Doppler sonography, or the more sensitive power Doppler sonography, is then performed to assess the presence and distribution of intranodular vessels.
Technique
In general, higher-frequency, linear transducers offer the best spatial resolution, whereas lower frequencies give better tissue penetration of the emitted sound waves. Because the findings of metastatic thyroid cancer may be subtle, the examination should be performed with the highest frequency possible. The superficial neck nodes should be evaluated with a linear, high-frequency transducer of at least 7.5 MHz, preferably greater than 10 MHz. Evaluation of the deep lymph nodes of the neck and the superior mediastinal nodes may require a lower frequency (5 to 7.5 MHz), small footprint curvilinear or sector probe that allows deeper sound penetration and can be positioned in the narrow suprasternal notch. Transducers with color Doppler capability are also preferred because assessment of the vascularity of lymph nodes is often helpful in identifying metastatic disease.
The patient should be in a supine position, with a pillow or rolled towel under the upper back to allow maximal extension of the neck. This technique is particularly important to examine the lower level IV and level VI nodes and the upper mediastinum. The examination should be systematic, imaging all the lymph node levels in the transverse plane. The longitudinal plane should also be used to examine levels II through V. Gray-scale sonography is used to identify the size, shape, and nodal architecture. Color Doppler sonography, or the more sensitive power Doppler sonography, is then performed to assess the presence and distribution of intranodular vessels.
Normal lymph nodes
Normal cervical lymph nodes are typically imaged during high-frequency sonography examination of the neck. Normal nodes are most commonly seen in the submandibular region, the upper cervical chain, and the posterior triangle (Levels IB, II, III, and V, respectively). There is a tendency for nodes to be larger with advancing age, perhaps because of increased fat deposition. The normal node is typically flat, oval, or kidney bean shaped ( Fig. 2 ). Nodes in the submandibular region and parotid region may be rounded without underlying pathology ( Fig. 3 ). Each lymph node is encased in a dense connective tissue known as the capsule. The periphery of the lymph node is known as the cortex and contains most of the lymphoid follicles. This dominant portion of the lymph node is typically hypoechoic, less commonly isoechoic to the surrounding soft tissues. The inner part of the node or the medulla is made up of fluid-filled sinuses and medullary cords from which the lymph flows from the afferent lymphatic vessels into the node. The feeding artery and vein are located in the hilum of the node along with the efferent draining lymphatic vessels. On sonography, the central nodal hilus is typically an echogenic structure caused by sound reflecting off the multiple fluid-filled sinuses. Normal nodes typically demonstrate only hilar vessels or are avascular, with the ability to detect vascularity by sonography paralleling the size of the node Figure 2 .
Metastatic lymph nodes
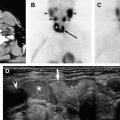
Various sonographic features have been described to aid in the differentiation of metastatic lymph nodes from normal ones, including increased lymph node size, rounded shape, absence of the echogenic hilus, hyper echogenicity, cystic change, presence of calcifications, and increased vascularity. Cervical lymph node size is unreliable as the sole criterion of metastatic thyroid carcinoma because hyperplastic nodes may be large and metastatic nodes may be normal in size ( Fig. 4 ). In general, lymph nodes are considered to be enlarged when the short axis exceeds 8 mm in the submandibular region (Level II) and 5 mm in other cervical regions. Malignant infiltration typically transforms nodes from an oval to a rounded shape ( Fig. 5 ). This change in shape is quantified by an increase in the short axis/long axis (S:L) ratio to a value greater than 0.5 ( Figs. 5, 6 ). An elevated S:L ratio carries a false-positive rate of approximately 10% to 15%, however, reflecting the common occurrence of lateral cervical node enlargement attributable to benign inflammatory conditions of the oropharynx, and a false-negative rate of 20% reflecting the propensity for microscopic nodal metastases to occur without enlarging the node, particularly with papillary thyroid carcinomas.
Absence of the echogenic hilus of a lymph node raises concern for tumor infiltration, obliterating the central sinuses and has been reported to carry a positive predictive value of 92% for the presence of metastatic thyroid cancer (see Fig. 6 ). It is worth noting that the detection of a normal hilum does not exclude metastatic disease to that node. The hilar vessels may still be identified with color or power Doppler sonography even in the setting of a non-visualized hilum secondary to metastatic disease. Malignant nodes may demonstrate abnormal vascular patterns, including increased peripheral or capsular flow either diffusely or focally, with or without increased central vascularity. Tumor deposits within a node may displace hilar vessels, produce avascular areas, or demonstrate focal regions with tortuous and aberrant vessels. These vascular patterns help to differentiate metastatic nodes from enlarged hyperplastic nodes, which tend to preserve nodal architecture with only increased central flow (see Fig. 4 ).
Hyperechogenicity, calcifications, and cystic change are features that highly predict the presence of metastatic thyroid cancer, particularly papillary thyroid cancer to affected nodes. Hyperechogenicity of a node relative to the adjacent musculature is a finding noted in up to 86% of metastatic lymph nodes from papillary thyroid cancer and is a rarely noted in benign nodes. The increased echogenicity is believed to be secondary to malignant follicular cells and colloid deposition within the metastatic node, which alters the normal hypoechoic appearance of cortex to the increased echogenicity typical of thyroid tissue ( Fig. 7 ). Initially the metastatic tumor deposits may be noted as tiny, focal hyperechoic regions in the periphery of the node or near the hilum. The sonographic detection of these often subtle metastatic foci to otherwise normal-appearing nodes can be improved by the use of color Doppler examination, which demonstrates focal increased vascularity in the suspect areas ( Fig. 8 ). As the node becomes progressively infiltrated with tumor, it demonstrates more diffuse regions of hyperechogenicity and increased vascularity, and typically other features of metastatic disease, such as enlarged size, rounded shape, obliteration of the hilum, calcifications, and cystic necrosis.
Intranodal calcifications have been noted in 46% to 69% of metastatic nodes from papillary thyroid carcinoma ( Fig. 9 ). Although intranodal calcifications may be seen in nodes affected by tuberculosis, sarcoidosis, and following radiotherapy, they are rare in non-thyroid metastases. The calcifications are typically fine or punctate and are located in the periphery of the node.