There are well-established differences in dementia incidence between communities and within communities over time. In part, these differences may be attributable to local improvements in dementia diagnosis and classification. Nevertheless, there are grounds for cautious optimism that there have been slight, but significant, recent reductions in dementia incidence. Possible causes include public health measures to reduce mortality attributable to stroke and heart disease, improved nutrition, and greater personal wealth. A life-course approach to dementia pathophysiology may help to elucidate the nature and timing of interventions that might delay dementia onset.
- 1.
There is nonrandom distribution of dementia incidence in space and time.
- 2.
International comparisons are needed to estimate the current and future dementia burden in developed and developing countries.
- 3.
In developed countries, there is some evidence that dementia incidence is decreasing, and this may be attributable to public health measures to reduce vascular disease and/or greater personal resources to buffer the effects of dementia.
- 4.
Nutritional epidemiology is relevant to understanding how and why dementia incidence might vary in space and time. This is true of folate/vitamin B 12 metabolism and, possibly, dietary fish oil.
- 5.
A life-course approach to understanding how and when risk factors increase susceptibility to vascular disease is relevant to late-life dementia. This approach may identify epigenetic pathways that involve both environmental and molecular genetic factors.
First, at one time it seemed that epidemiologic studies in dementia would be superseded by advances in laboratory molecular genetics. Supported by identification of genetic mutations in early onset AD (EOAD), claims were made that the causes of AD, irrespective of age at onset, were genetic and that these would soon be remediable. So far, among many putative associations only APOE ϵ4 has remained a well-established genetic susceptibility factor for late-onset AD (LOAD). Molecular genetic research programs can deploy large-scale detection techniques using genome-wide association study methods. These powerful methods detect many genes each of small effect and results so far are promising. However, convincing replication of findings in LOAD remains elusive and, at least for some time, a considered combination of molecular genetic and epidemiologic methods will continue to be used to unravel the complex multifactorial causes of AD. To date, no evidence relevant to understanding genetic sources of differences between geographic areas has been presented.
Second, epidemiologic data cannot be assumed to be transferable across cultures or to be stable within 1 culture over time. However, what seems like a major potential source of error can become a strength and it is here that spatial epidemiology is most helpful. Apparent inconsistencies in cross-cultural epidemiologic observational data provide clues to the complex multifactorial nature of the dementias. When well-defined populations differ significantly from others in patterns of AD incidence, their genetic structures and environmental exposures become topics of intense scrutiny. The best-known example is found among the Chamarro people of the Pacific Island of Guam who suffer from a complex syndrome with features of Parkinson disease, AD, and motor neuron disease (the Parkinson-dementia complex of Guam) but for whom there is no clear-cut evidence for either a genetic or environmental cause.
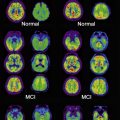
Dementia diagnosis and classification
Secular trends and spatial distributions of AD are relevant to understanding how multiple causal factors might influence life-course pathways toward AD. To become a case of dementia, an individual must cross thresholds of loss of cognitive performance and activities of daily living, and should show worsening progression from a premorbid (ie, original) level of mental performance. These thresholds are open to individual variation. People of higher socioeconomic status who have strong family support and who can retain sufficient mental flexibility to compensate for early deficits attributable to the presence of brain pathology present to health services later in the course of their dementia. At presentation, these individuals often show a greater degree of brain pathology than those who do not have similar support or advantageous socioeconomic circumstances. Therefore, it follows that, when there are improvements in the material well-being of a society, when measures are in place to enhance family and community support, the apparent incidence of dementia might decline. Accurate dementia case ascertainment should continue to rely on prospective longitudinal studies with access to a wide range of data sources relevant to both hospital-treated cases and those who remain in the community and do not enter the hospital system.
These considerations weaken the preconception that a simple mechanistic model of dementia onset, with gold standard criteria for case recognition, suffices for all individuals with dementia. In turn, acceptance of sources of individual variation indicates that, in some instances, certain putative risk factors for dementia identified in observational studies might not be determinants of dementia but consequences of case-finding methodology. A good example of the steps needed to identify and allow for these effects was provided by a ground-breaking cross-cultural study.
During the second half of the last century, consistent measures of the incidence and prevalence of late-onset dementias were gradually established. Using harmonized diagnostic criteria and acceptable survey methods, findings from pioneering European studies in Scandinavia, the United Kingdom, Italy, and Holland were used to inform public policy and social and biomedical research. Within the broad grouping of the late-onset dementias, and encouraged by progress in neurochemical studies, governments and the pharmaceutical industry began to focus on AD almost to the exclusion of other forms of dementia. The public and press became aware of AD as a major cause of disability and premature death that was seriously underreported and had remained a neglected research topic. Opinion leaders emphasized that the burgeoning epidemic of AD would become the single greatest threat to the maintenance of health care and living standards of old people, with great potential to jeopardize the capacity of developed countries to maintain satisfactory standards of health care and social support for all sections of society. Urgent concern about the implications of a silent dementia epidemic is, with hindsight, now recognized as the first tangible benefit of more than 25 years of intense epidemiologic research in dementia.
Although broadly similar estimates of the incidence and prevalence of AD are now widely accepted, there are some caveats. The first is that research methods have differed between localities and over time. Specifically, European investigators pioneered diagnostic procedures based on standardized psychiatric interviews and were greatly influenced by the success of the UK-US diagnostic project for which an interview-based method (The Present State Examination [PSE]) amenable to the application of computerized diagnostic algorithms was developed. The PSE was founded on precise definitions of psychopathology that would discriminate most efficiently between functional psychoses, specifically schizophrenia, and the affective psychoses. Systematic questions posed by trained interviewers (who did not need to be clinicians) contained elements of each definition to determine the presence of a symptom or sign of disorder, its severity, and its duration. The PSE did not deal adequately with the dementias and Copeland and colleagues addressed this deficiency by applying the PSE format to dementia diagnosis, leading to the development of the Geriatric Mental State (GMS) Examination. As with the PSE, computer-based algorithms provided classifications of the mental disorders of late life, each of which could be validated against clinical examinations that included data from a clinical history, from informants, and, where indicated, from a limited neurologic examination.
These semistructured interviews represented a major improvement on previous attempts at case finding in epidemiologic studies of dementia. Although most often used in a single interview, the interviews could be used in 2 or more phases in longitudinal studies of dementia incidence. During this early phase of development of diagnostic criteria for AD for use in epidemiologic studies, great care was taken to distinguish between dementias of presumed vascular origin and dementia without evidence of cerebrovascular disease. A simple checklist had been devised from criteria listed in standard textbooks and provided a total score to represent the presence of cortical infarcts. In large part, this approach was based on the idea that detection of large cortical infarcts supported a diagnosis of multi-infarct dementia and allowed for minor cerebrovascular involvement with some AD features but, if there was no evidence of cerebrovascular disease, then an AD diagnosis was likely. The diagnosis of AD was, therefore, made largely by exclusion of other causes of dementia, principally vascular dementias.
In the United States, dementia researchers developed a second approach that is now popular in European studies, probably because it makes better use of the wide range of possible data sources relevant to a dementia diagnosis. The US approach accepted that, in the absence of valid and reliable diagnostic biomarkers to detect the presence of dementia or any of its subtypes, and faced by variations between clinicians in the detection and recording of diagnostic features, a consensus group drawn from relevant disciplines (eg, psychiatry, neurology, clinical psychology, neuroimaging, neuropathology) could achieve agreement on diagnostic classification in the absence of gold standard biomarkers. This approach allowed for variation in mental state over time and the presence of vascular lesions, and provided a counterbalance to the tendency for the application of diagnostic procedures to become idiosyncratic when reliance was placed solely on a single individual repeatedly applying the same criteria to datasets of uneven quality. The US approach was particularly notable for its clear recommendations that certain cognitive deficits were more often found in early AD (eg, dyspraxia) than in other dementias. Advantages of the prevailing US approach included the opportunity to examine relationships between acute cerebrovascular events as triggers for the gradual onset of dementia of the Alzheimer type, whereas, at that time, the European approach would most likely have categorized any subsequent dementia as cerebrovascular in origin. The consensus approach also identified opportunities to improve dementia diagnoses using biomarkers.
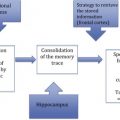
The US consensual diagnostic approach seems also to deal appropriately with the contribution of individual differences in the capacity to cope with or adjust for the presence of dementia pathology. This last is not a trivial point: the capacity of an individual to cope with a dementia disorder may depend on personal attributes loosely labeled resilience, but more precisely may be understood as aspects of intelligence, a socially engaged lifestyle, and a preference for mentally effortful recreational pursuits. The idea that an individual possesses a quantifiable cognitive reserve to mitigate the effects of neuropathology (arising from dementia or brain damage incurred through stroke or trauma) is widely discussed and is supported by the repeated observation that there is not a direct relationship between the degree of brain pathology and the severity of clinical features of dementia. From an epidemiologic perspective, the positive contributions of cognitive reserve that could buffer the effects of AD neuropathology suggest a basic distinction between those factors that increase AD risk and those that decrease it, perhaps through neuroprotective mechanisms.
The geography of dementia
Shared environmental exposures and nongenetic transmission of disease are closely related to detection of spatial proximity. Observational studies of this type often assume that risk of disease is greater if people at increased risk are closely related in space and time. The basic approach in spatial epidemiology is to examine maps of disease distributions and/or secular trends in the incidence of a disease. Beyond this basic idea lies a major problem of testing a statistical hypothesis. The typical aim is to identify clusters of disease, but these aims rarely extend to explicit causal inferences being drawn with confidence from the data. However, in terms of public understanding of disease risk, maps provide an accessible method of presenting otherwise difficult-to-understand scientific evidence in support of a particular estimation of disease risk.
The prevailing research strategy in the epidemiology of LOAD is to study multiple risk factors in samples at risk of LOAD on grounds of age and the presence or absence of specific risk factors (eg, family history of dementia). Population samples are usually drawn from well-defined areas with known demographics. It is especially helpful if exposures to dementia risk or neuroprotective factors have already been established in the population. A good example of this approach is provided by studies that explored the possible benefits and timing of nonsteroidal antiinflammatory agents (NSAIDs) in the prevention of AD. Table 1 is adapted from population-based cross-sectional studies at 11 study sites and summarizes current estimates of the prevalence of dementia adjusted for differences in the age and sex distribution of local populations. This type of study is an excellent example of the research methods required in spatial epidemiology to understand how dementia might present at different sites, how diagnostic practices might influence findings, and how levels of dementia-related disability are important. The investigators needed to devise methods to adjust for survival differences, socioeconomic factors, and variations in education and health service provision between geographic regions to obtain reliable estimates of dementia prevalence in each study locality.
| Study Sites | Standardized Prevalence (%) | SMR (EURODEM) a |
|---|---|---|
| Latin America (urban) | 4.6 | 80 (70–91) |
| Latin America (rural) | 1.5 | 27 (16–41) |
| China (urban) | 3.0 | 57 (36–86) |
| China (rural) | 2.4 | 56 (32–91) |
| India (urban) | 0.9 | 22 (7–41) |
| India (rural) | 0.8 | 18 (5–34) |
a SMR is obtained by applying estimates derived from pooled European surveys (EURODEM) to the samples recruited at each of the listed study sites. An SMR of 100 implies that the observed number of dementia cases agrees with the number expected in that sample using EURODEM estimates; an SMR less than 100 implies that the prevalence is lower than would be expected in a European sample with the same age and sex distribution.
International studies also support the proposal that dementia prevalence varies between geographic regions, and encourages the view that environmental exposures contribute to dementia. Among these studies, comparisons between African Americans living in Indianapolis (IN) and the indigenous Yoruba living in and around Ibadan in Nigeria provide compelling evidence that these international differences between populations are not spurious and require explanation. The Ibadan-Indianapolis studies stimulated useful discussion about the genetic structure of African American and native Nigerian populations and how intergenerational continuities of poverty and poor diet could have affected African Americans to a greater extent than native Nigerians, and stimulated a search for sources of geographic difference in dementia risk. The heuristic value of these comparisons has several possible explanations:
- a.
More stressful urban life of African Americans
- b.
Lower intensity and shorter duration of formal schooling among rural African Americans
- c.
Exposure in urban United States to pollutant neurotoxins (eg, atmospheric lead)
- d.
A Western diet that is calorie rich and nutrient poor
- e.
An increased risk of abnormal age-related glucose metabolism and type II diabetes
- f.
Greater use of alcohol and tobacco among African Americans
- g.
Better diet of native Nigerians, with fewer calories, more fresh fruit and vegetables, little red meat, and more fish
- h.
Differences in intracerebral cholesterol metabolism between Nigerians and African Americans.
Scottish studies on the geographic distribution of EOAD support the view that EOAD distribution is nonrandom. Clusters of cases were found in areas of Scotland associated with coal mining at the time of birth of EOAD cases. Kinship analyses of these clusters suggested that genetic relatedness did not explain these areas of high EOAD density.
To understand environments within which an individual develops and loses cognitive competencies, it is helpful to apply research methods that can distinguish between different components of the environment that are relevant to cognitive maturation and decline. This distinction can be achieved by arranging environmental influences in a hierarchy based on the size of their effects at different points in the life course and judgments about the relative importance of specific timing of exposures (critical periods). These methods of life-course research in aging research and in the epidemiology of diseases of late life (including the dementias) are in the first phase of construction. Life-course theory has the potential to draw together apparently diverse contributions identified in epidemiologic studies concerning the causes of late-onset dementias including AD. The application of life-course methodology to different geographic settings has the potential to show how childhood experiences can modify the risk of late-onset dementia.
The geography of dementia
Shared environmental exposures and nongenetic transmission of disease are closely related to detection of spatial proximity. Observational studies of this type often assume that risk of disease is greater if people at increased risk are closely related in space and time. The basic approach in spatial epidemiology is to examine maps of disease distributions and/or secular trends in the incidence of a disease. Beyond this basic idea lies a major problem of testing a statistical hypothesis. The typical aim is to identify clusters of disease, but these aims rarely extend to explicit causal inferences being drawn with confidence from the data. However, in terms of public understanding of disease risk, maps provide an accessible method of presenting otherwise difficult-to-understand scientific evidence in support of a particular estimation of disease risk.
The prevailing research strategy in the epidemiology of LOAD is to study multiple risk factors in samples at risk of LOAD on grounds of age and the presence or absence of specific risk factors (eg, family history of dementia). Population samples are usually drawn from well-defined areas with known demographics. It is especially helpful if exposures to dementia risk or neuroprotective factors have already been established in the population. A good example of this approach is provided by studies that explored the possible benefits and timing of nonsteroidal antiinflammatory agents (NSAIDs) in the prevention of AD. Table 1 is adapted from population-based cross-sectional studies at 11 study sites and summarizes current estimates of the prevalence of dementia adjusted for differences in the age and sex distribution of local populations. This type of study is an excellent example of the research methods required in spatial epidemiology to understand how dementia might present at different sites, how diagnostic practices might influence findings, and how levels of dementia-related disability are important. The investigators needed to devise methods to adjust for survival differences, socioeconomic factors, and variations in education and health service provision between geographic regions to obtain reliable estimates of dementia prevalence in each study locality.