
Spinal Registration Accuracy and Error
Interactive frameless stereotactic technology has been successfully applied to spinal surgery. By linking digitized image data to spinal surface anatomy, image-guided spinal navigation facilitates the surgeon’s orientation to unexposed spinal structures, thereby improving the precision and accuracy of the surgery. It is typically used to optimize the placement of spinal fixation screws and to monitor the extent of complex decompressive procedures. It can also be used as a preoperative planning tool.
The critical step in applying stereotactic technology to spinal surgery is the registration process. Both paired point registration and surface mapping techniques have been applied to image-guided spinal navigation. This chapter discusses the accuracy and errors of these registration techniques.
Over the last decade, the surgical options for managing complex spinal disorders have expanded through the continued evolution of spinal instrumentation devices as well as a variety of surgical approaches to the spine. However, intraoperative orientation to unexposed spinal anatomy provides difficulties to even the most experienced spinal surgeon. Regardless of the approach selected, much of the spinal anatomy in the surgical field is not directly visualized in the operative field. This is not problematic for routine decompressive procedures but can pose significant problems during the management of complex disorders such as fractures, neoplasms, and deformities.
Orientation to this unexposed spinal anatomy is critical to the success of complex spinal surgery. In particular, the variety of spinal fixation techniques that utilize the placement of bone screws into the pedicles of the thoracic, lumbar, and sacral spine; into the lateral masses and across joints of the cervical spine; and across the vertebrae of the thoracic and lumbar spine require a thorough understanding of the spatial relationships of the unexposed spinal anatomy to that portion of the spine seen in the surgical field. Although standard intraoperative imaging (i.e., fluoroscopy) can be helpful, it does not provide an axial plane image. For most spinal screw fixation procedures, the axial plane provides critical trajectory information that cannot be provided by either a sagittal or a coronal image.
The development of image-guided technology for spinal surgery was influenced by these difficulties of intraoperative spatial orientation during complex surgery as well as by the limitations of standard intraoperative imaging.1,2 The initial application of stereotactic principles to spinal surgery was not intuitive. Unlike intracranial surgery, an external frame system was not practical for spinal surgery. Furthermore, the use of surface landmarks or fiducials could not be used because of skin movement with respect to bony landmarks.3,4 This is less of a problem with intracranial applications because of the relatively fixed position of the overlying scalp to a set of attached fiducials.
The application of stereotactic technology to spinal surgery involves using the rigid spinal anatomy itself as a frame of reference for registration of the image data to the spinal anatomy. Two separate techniques of registration can be applied. Paired point registration involves matching selected points in the image data set to their corresponding points in the spinal anatomy.
Alternatively, the surface mapping technique involves selecting multiple nondiscrete points only on the exposed and debrided surface of the spine in the surgical field. This technique does not require the preselection of points in the image set, although several discrete points in both the image data set and the surgical field are frequently required to improve the accuracy of surface mapping. The positional information of these points is transferred to the workstation, and a topographic map of the selected anatomy is created and “matched” to the patient’s image set.
Typically, paired point registration can be done more quickly than surface mapping. The average time needed for paired point registration is 10 to 15 seconds. The time needed for surface mapping is much longer, with difficult cases requiring as much as 10 to 15 minutes. This time difference can significantly impact the length of the navigational procedure and the surgery itself.5
Regardless of the technique used, the registration process represents the step during image-guided navigation that can have the greatest effect on navigational accuracy. Registration accuracy is dependent on the surgeon carefully selecting the correct reference points or performing the surface mapping process. If properly performed, registration will allow for the display of reformatted, multiplanar CT or MRI images to assist the surgeon with orientation to the unexposed spinal anatomy.
 Navigational Technique
Navigational Technique
A variety of navigational systems have evolved over the past decade. The common components of most of these systems include an image-processing workstation interfaced with a two-camera optical localizer (Fig. 3–1). The optical localizer tracks infrared light emitted by a series of light-emitting diodes (LEDs) mounted on a customized handheld navigational probe or selected surgical instruments (Fig. 3–2). Alternatively, the optical localizer itself can be the source of infrared light, which is continuously reflected back to the camera system by passive reflectors attached to the probe or selected surgical instruments.
The computer workstation knows the dimensions of each navigational probe or customized trackable surgical instrument and also recognizes the spacing of the LEDs or passive reflectors. The infrared light that is transmitted from or reflected by these instruments is relayed to the computer workstation, which can then calculate the precise location of the instrument tip in the surgical field as well as the location of the anatomic point on which the instrument tip is resting.
When applying navigational technology to spinal surgery, the standard surgical exposure for a particular procedure is carried out. The registration process is performed immediately after surgical exposure and prior to any planned decompressive procedure. This preserves the spinal anatomic landmarks that facilitate an easy and accurate registration process.
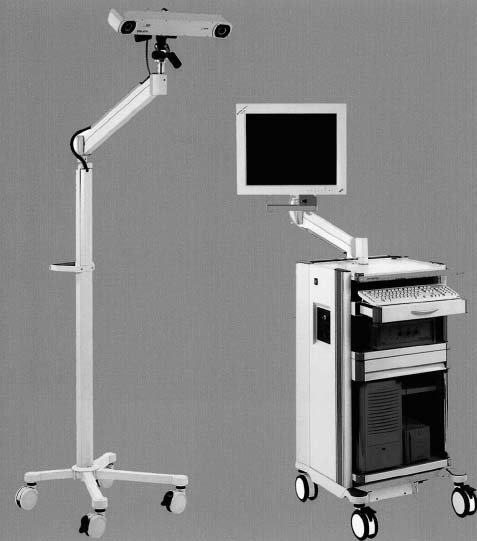
FIGURE 3–1. Image-guided navigational workstation with infrared camera localizer system.
The registration process establishes a precise spatial relationship between the image space of the data and the physical space of the patient’s corresponding surgical anatomy. If the patient is moved after registration, this spatial relationship is distorted, which creates navigational information that is inaccurate. This problem can be minimized by the optional use of a spinal tracking device consisting of a separate set of LEDs or passive reflectors mounted on an instrument that can be attached to the exposed spinal anatomy (Fig. 3–3). The position of the reference frame can be tracked by the camera system. Movement of the frame alerts the navigational system to any inadvertent movement of the spine. The system can then make correctional steps to keep the registration process accurate and eliminate the need to repeat the registration process. The disadvantages of using a tracking device are the added time needed for its attachment to the spine, the need to maintain a line of sight between it and the camera, and the inconvenience of having to perform the procedure with the device placed in the surgical field.
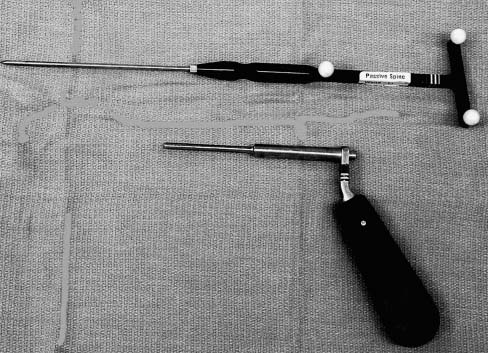
FIGURE 3–2. Navigation probe with drill guide for spinal surgery.
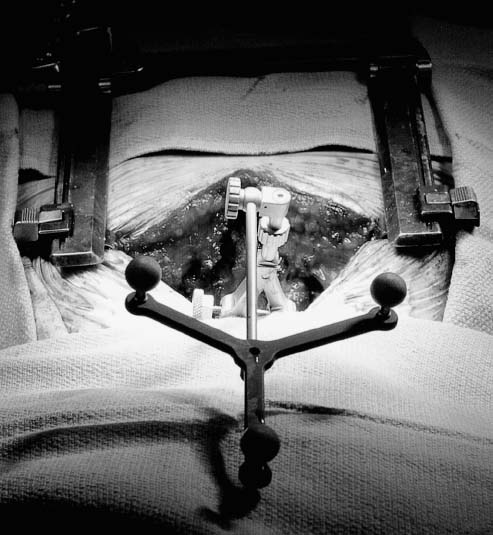
FIGURE 3–3. Reference frame attached to spinal anatomy. The reference frame monitors inadvertent movement of the spinal anatomy that may interfere with navigational accuracy.
Alternatively, image-guided spinal navigation can be performed without a tracking device.1,2,5,6 This involves acknowledging the effect of patient movement on the accuracy of image-guided navigation and maintaining reasonable stable patient position during the relatively short amount of time needed (i.e., 10–20 seconds) for the selection of each appropriate screw trajectory. Patient movement can be caused by respiration, the surgical team leaning on the table, or a change of table position. Movement associated with patient respiration is negligible and does not require any tracking even in the thoracic spine. Although movement associated with leaning on the table or repositioning the table or the patient will affect registration accuracy, it can be easily avoided during the short navigational procedure. If inadvertent patient movement does occur, the registration process can be repeated.
Repeating the registration process is far more practical with the shorter paired point technique than it is with the more time-consuming surface mapping technique.
 Registration Accuracy
Registration Accuracy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





