Spine
Methods of imaging the spine
Many of the earlier imaging methods are now only of historical interest (e.g. conventional tomography, epidurography, epidural venography):
1. Plain films. These are widely available, but with low sensitivity. They are of questionable value in chronic back pain because of the prevalence of degenerative changes in both symptomatic and asymptomatic individuals of all ages beyond the second decade. They are, however, useful in suspected spinal injury, spinal deformity and postoperative assessment.
2. Myelography/radiculography. This is used when MRI is contraindicated or unacceptable to the patient. It is usually followed by CT for detailed assessment of abnormalities (CT myelography).
3. Discography. Advocates still regard it as the only technique able to verify the presence and source of discogenic pain.
4. Facet joint arthrography. Facet joint pain origin can be confirmed if it is abolished after diagnostic injection of local anaesthetic, and treated by steroid instillation. The radiological appearances of the arthrogram are not helpful for the most part except in showing a communication with a synovial cyst. Vertical and contralateral facet joint communications can arise in the presence of pars interarticularis defects.
5. Arteriography. This is used for further study of vascular malformations shown by other methods, usually MRI, and for assessment for potential embolotherapy. It is not appropriate for the primary diagnosis of spinal vascular malformations. It may be used for pre-operative embolization of vascular vertebral tumours (e.g. renal metastasis).
6. Radionuclide imaging. This is largely performed for suspected vertebral metastases and to exclude an occult painful bone lesion (e.g. osteoid osteoma) using a technetium scintigraphic agent, for which it is a sensitive and cost-effective technique.
7. Computed tomography (CT). CT provides optimal detail of vertebral structures and is particularly useful in spinal trauma, spondylolysis, vertebral tumours, spinal deformity and postoperative states, especially if multidetector CT (MDCT) is available.
8. Magnetic resonance imaging (MRI). This is the preferred technique for virtually all spinal pathology. It is the only technique that directly images the spinal cord and nerve roots. MRI with intravenous (i.v.) gadolinium-DTPA is indicated in spinal infection, tumours and postoperative assessment.
9. Ultrasound (US). This is of use as an intra-operative method, and has uses in the infant spine.
Imaging approach to back pain and sciatica
There are a variety of ways to image the spine, many of which are expensive. The role of the radiologist is to ensure that diagnostic algorithms are selected for diagnostic accuracy, clinical relevance and cost-effectiveness. Each diagnostic imaging procedure has a different degree of sensitivity and specificity when applied to a particular diagnostic problem. A combination of imaging techniques can be used in a complementary way to enhance diagnostic accuracy. The appropriate use of the available methods of investigating the spine is essential, requiring a sensible sequence and timing of the procedures to ensure cost-effectiveness, maximal diagnostic accuracy and clinical effectiveness with minimum discomfort to the patient.
The philosophy underlying the management of low back pain and sciatica encompasses the following fundamental points:
1. Radiological investigation is essential if surgery is proposed.
2. Radiological findings should be compatible with the clinical picture before surgery can be advised.
3. It is vital for the surgeon and radiologist to identify those patients who will and who will not benefit from surgery.
4. In those patients judged to be in need of surgical intervention, success is very dependent on precise identification of the site, nature and extent of disease by the radiologist.
5. The demonstration of degenerative disease of the spine by non-invasive methods cannot be assumed to be the cause of the patient’s symptoms, as similar changes are often seen in asymptomatic individuals.
The need for radiological investigation of the lumbosacral spine is based on the results of a thorough clinical examination. A useful and basic preliminary step, which will avoid unnecessary investigations, is to determine whether the predominant symptom is back pain or leg pain. Leg pain extending to the foot is indicative of nerve root compression and imaging needs to be directed towards the demonstration of a compressive lesion, typically disc prolapse. This is most commonly seen at the L4/5 or L5/S1 levels (90–95%), and MRI should be employed as the primary mode of imaging. If the predominant symptom is back pain, with or without proximal lower limb radiation, then invasive techniques may be required, including discography and facet joint arthrography. The presence of degenerative disc and facet disease demonstrated by plain films, CT or MRI has no direct correlation with the incidence of clinical symptomatology. The annulus fibrosus of the intervertebral disc and the facet joints are richly innervated, and only direct injection can assess them as a potential pain source. However, unless there are therapeutic implications, there is no indication to go to these lengths, as many patients can be managed by physiotherapy and mild analgesics.
Conventional radiography
Routine radiographic evaluation at the initial assessment of a patient with acute low back pain does not usually provide clinically useful information. Eighty-five per cent of such patients will return to work within 2 months having received only conservative therapy, indicating the potential for non-contributory imaging. Despite the known limitations of radiographs, it is often helpful to obtain routine radiographs of the lumbar spine before another investigation is requested. The role of conventional radiographs can be summarized in the following points:
1. They assist in the diagnosis of conditions that can mimic mechanical or discogenic pain, e.g. infection, spondylolysis, ankylosing spondylitis and bone tumours, though in most circumstances 99mTc scintigraphy, CT and MRI are more sensitive.
2. They serve as a technical aid to survey the vertebral column and spinal canal prior to myelography, CT or MRI, particularly in the sense of providing basic anatomical data regarding segmentation. Failure to do this may lead to errors in interpreting correctly the vertebral level of abnormalities prior to surgery.
3. Correlation of CT or MRI data with radiographic appearances is often helpful in interpretation.
Computed tomography and magnetic resonance imaging of the spine
CT and MRI have replaced myelography as the primary method for investigating suspected disc prolapse. High-quality axial imaging by CT is an accurate means of demonstrating disc herniation but, in practice, many studies are less than optimal due to obesity, scoliosis and beam-hardening effects due to dense bone sclerosis. For these reasons, and because of better contrast resolution, MRI is the preferred technique and CT is only employed when MRI cannot be used. MRI alone has the capacity to show the morphology of the intervertebral disc, and can show ageing changes, typically dehydration, in the nucleus pulposus. It provides sagittal sections, which have major advantages for the demonstration of the spinal cord and cauda equina, vertebral alignment, stenosis of the spinal canal, and for showing the neural foramina. Far lateral disc herniation cannot be shown by myelography, but is readily demonstrated by CT or MRI. CT may be preferred to MRI where there is a suspected spinal injury, in the assessment of primary spinal tumours of bony origin, and in the study of spondylolysis and Paget’s disease. MRI in spinal stenosis provides all the required information showing all the relevant levels on a single image, the degree of narrowing at each level and the secondary effects such as the distension of the vertebral venous plexus. The relative contributions of bone, osteophyte, ligament or disc, while better evaluated by CT, are relatively unimportant in the management decisions. Furthermore, MRI will show conditions which may mimic spinal stenosis such as prolapsed thoracic disc, ependymoma of the conus medullaris and dural arteriovenous fistula.
In addition to the diagnosis of prolapsed intervertebral disc, CT and MRI differentiate the contained disc, where the herniated portion remains in continuity with the main body of the disc, from the sequestrated disc, where there is a free migratory disc fragment. This distinction may be crucial in the choice of conservative or surgical therapy, and of percutaneous rather than open surgical techniques. MRI studies have shown that even massive extruded disc lesions can resolve naturally with time, without intervention. Despite the presence of nerve root compression, a disc prolapse can be entirely asymptomatic. Gadolinium enhancement of compressed lumbar nerve roots is seen in symptomatic disc prolapse with a specificity of 95.9%.1
Finally, in the decision as to whether to choose CT or MRI it should be remembered that lumbar spine CT delivers a substantial radiation dose, which is important, particularly in younger patients.
The main remaining uses of myelography are in patients with claustrophobia or who are otherwise not suitable for MRI. There are advocates for the use of CT myelography in the investigation of MRI-negative cervical radiculopathy. Myelography also allows a dynamic assessment of the spinal canal in instances of spinal stenosis and instability. The use of a special MR-compatible spinal harness that provides axial loading, and the availability of open and upright MR scanners also provide non-invasive dynamic MR imaging capability.
The problems of the ‘post-laminectomy’ patient or ‘failed back surgery syndrome’ are well known. Accurate pre-operative assessment should limit the number of cases resulting from inappropriate surgery and surgery at the wrong level. The investigation of the postoperative lumbar spine is difficult and re-operation has a poor outcome in many cases. Although the investigation of the postoperative lumbar spine is difficult, it is vital to make the distinction between residual or recurrent disc prolapse at the operated level and epidural fibrosis in order to minimize the risk of a negative re-exploration. The best available technique is gadolinium-enhanced MRI.
Arachnoiditis is a cause of postoperative symptoms and its features are shown on myelography, CT myelography and MRI. In the past, many cases were caused by the use of myodil (Pantopaque) as a myelographic contrast medium. It is likely that the use of myodil as an intrathecal contrast agent caused arachnoiditis in most cases, but this became symptomatic in only a minority. The potentiating effects of blood in the CSF, particularly as a result of surgery, have been evident in many cases. New cases of arachnoiditis are now rarely seen, but there is residue of chronic disease still presenting from time to time.
Conclusions
MRI has revolutionized the imaging of spinal disease. Advantages include non-invasiveness, multiple imaging planes and lack of radiation exposure. Its superior soft tissue contrast enables the distinction of nucleus pulposus from annulus fibrosus of the healthy disc and enables the early diagnosis of degenerative changes. However, up to 35% of asymptomatic individuals less than 40 years of age have significant intervertebral disc disease at one or more levels on MRI images. Correlation with the clinical evidence is, therefore, essential before any relevance is attached to their presence and surgery is undertaken. As MRI is, at present, not as accurate as discography in the diagnosis and delineation of annular disease, and in diagnosing the pain source, there has been a resurgence of interest in discography. MRI should be used as a predictor of the causative levels contributing to the back pain with discography having a significant role in the investigation of discogenic pain prior to surgical fusion.2
Boden, SD, Davis, DO, Dina, TS, et al. Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. J Bone Joint Surg Am. 1990; 72(3):403–408.
Butt, WP. Radiology for back pain. Clin Radiol. 1989; 40(1):6–10.
Cribb, GL, Jaffray, DC, Cassar-Pullicino, VN. Observations on the natural history of massive lumbar disc herniation. J Bone Joint Surg Br. 2007; 89(6):782–784.
du Boulay, GH, Hawkes, S, Lee, CC, et al. Comparing the cost of spinal MR with conventional myelography and radiculography. Neuroradiology. 1990; 32(2):124–136.
Horton, WC, Daftari, TK. Which disc as visualized by magnetic resonance imaging is actually a source of pain? A correlation between magnetic resonance imaging and discography. Spine. 1992; 17(Suppl 6):S164–S171.
Hueftle, MG, Modic, MT, Ross, JS, et al. Lumbar spine: post-operative MR imaging with gadolinium-DTPA. Radiology. 1988; 167(3):817–824.
Myelography and radiculography
Contrast media
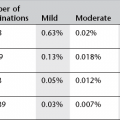
Historically, the contrast media that have been used for myelography include gas (CO2, air), lipiodol, abrodil, myodil (Pantopaque, iodophenylate), meglumine iothalamate (Conray), meglumine iocarmate (Dimer X), metrizamide (Amipaque), iopamidol (Niopam), iohexol (Omnipaque) and iotrolan (Isovist). The early oil-based media were diagnostically poor and led to arachnoiditis. The early water-soluble media were very toxic and also led to arachnoiditis, and the first intrathecal contrast medium with acceptably low toxicity was metrizamide, a non-ionic dimer. Iohexol and iopamidol are non-ionic monomers licensed for intrathecal use and the ones most commonly used currently.
Cervical myelography
This may be performed by introduction of contrast medium into the thecal sac by lumbar puncture and then run up to the cervical spine, or by direct cervical puncture at C1/2.
Indications
Suspected spinal cord pathology or root compression in patients unable or unwilling to undergo MRI imaging.
Lateral cervical or C1/2 puncture v lumbar injection
Cervical puncture is quick, safe and reliable but is contraindicated in patients with suspected high cervical or cranio-cervical pathology, and where the normal bony anatomy and landmarks are distorted or lost by anomalous development or rheumatoid disease. Complications are rare but include vertebral artery damage and inadvertent cord puncture. Cervical puncture is particularly indicated where there is severe lumbar disease, which may restrict the flow of contrast medium and may make lumbar puncture difficult, and when there is thoracic spinal canal stenosis. It is also required for the demonstration of the upper end of a spinal block. It is not a good technique for whole-spine myelography; after completion of a cervical myelogram, the contrast medium is too dilute for effective use in the remainder of the spinal canal. When lumbar injection is used, a good lumbar study is possible without dilution, following which a cervical and thoracic study is entirely feasible. Lumbar injection for cervical myelography is as effective as cervical injection when nothing restricts the upward flow of contrast medium. The post-procedural morbidity, mainly consisting of headache, is rather less after cervical puncture.
Contrast medium
Non-ionic contrast medium is used (see above). The total dose should not exceed 3 g of iodine, i.e. 10 ml of contrast medium with a concentration of 300 mg ml−1. Adequate filling for cervical myelography usually only requires 7–8 ml, or even less when the canal is narrow.
Equipment
Tilting X-ray table with a C-arm fluoroscopic facility for screening and radiography in multiple planes.
Patient preparation
Mild sedation with oral diazepam is appropriate in anxious patients, but is not essential. The skin puncture point is outside the hair line and no hair removal is generally needed, though the hair should be gathered into a paper cap.
Technique
1. The patient lies prone with arms at the sides and chin resting on a soft pad so that the neck is in a neutral position or in slight extension. Marked hyperextension is undesirable as it accentuates patient discomfort, particularly in those with spondylosis, who comprise the majority of patients referred for this procedure. In such cases it will further compromise a narrowed canal and may produce symptoms of cord compression. The patient must be comfortable and able to breathe easily.
2. Using lateral fluoroscopy the C1/2 space is identified. The beam should be centred at this level to minimize errors due to parallax. Head and neck adjustments may be needed to ensure a true lateral position. The aim is to puncture the subarachnoid space between the laminae of C1 and C2, at the junction of the middle and posterior thirds of the spinal canal, i.e. posterior to the spinal cord. A 20G spinal needle is used. There is better control with the relatively stiff 20G needle, and the requirement for a small needle size to minimize CSF loss does not apply in the cervical region, where CSF pressure is very low.
3. Using aseptic technique, the skin and subcutaneous tissues are anaesthetized with 1% lidocaine. The spinal needle is introduced with the stilette bevel parallel to the long axis of the spine, i.e. to split rather than cut the fibres of the interlaminar ligaments. Lateral fluoroscopy is used to adjust the direction of the needle, and ensure the maintenance of a perfect lateral position as the needle is advanced. It is very helpful if a nurse steadies the patient’s head.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree