Spine Infection, Inflammation, and Demyelination
David B. Khatami
Pritesh Mehta
Prachi Dubey
Yu-Ming Chang
Rafeeque Bhadelia
QUESTIONS
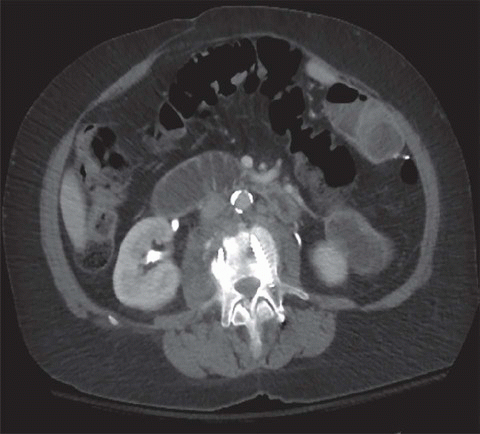
1 A 50-year-old female with back pain, fevers, and chills presented to the ER. A contrast-enhanced CT was performed. Key image is shown below.
|
1a Which of the following can be a possible explanation for the patient’s symptoms?
A. Mechanical small bowel obstruction
B. Lumbar fusion hardware infection
C. Pyelonephritis
D. Ruptured viscus with abscess formation
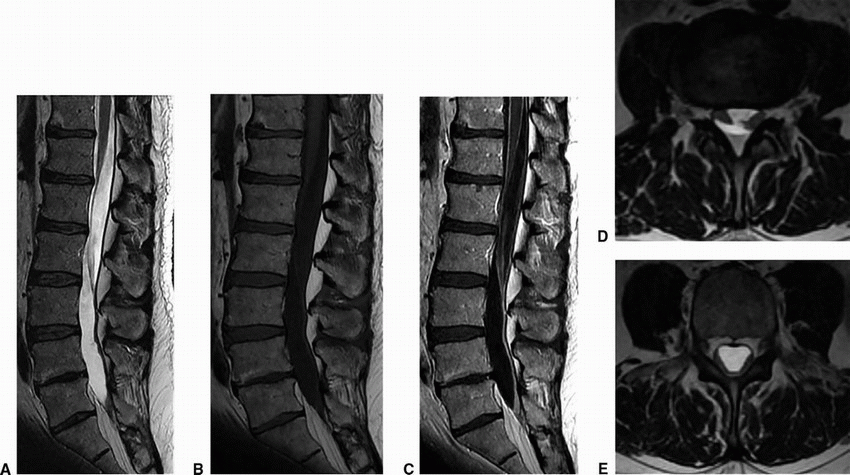
To further assess the abnormality, an MRI of the lumbar spine was performed. Key image is shown below.
|
View Answer
1a Answer B. Lumbar fusion hardware infection. Note the soft tissue thickening seen in the right psoas muscle and lucency surrounding the tip of the right pedicle screw.
1b What is the diagnosis?
A. Discitis/osteomyelitis
B. Modic type 1 endplate changes
C. Metastasis
D. Inflammatory spondylitis
View Answer
1b Answer A. Discitis/osteomyelitis. This is at the level of hardware as noted on CT and likely to be secondary to hardware infection.
Imaging Findings: Figure 1. CT demonstrates soft tissue thickening surrounding the right psoas muscle (arrow in A) and a lucency along the tip of the right pedicle screw (black circle in A), concerning for infection.
Figure 2. Sagittal STIR images demonstrate edema in the L2 and L3 vertebral bodies (long arrow in A) and within the disc space (short arrow in A), concerning for discitis/osteomyelitis.
Discussion: Discitis/osteomyelitis with hardware infection. This can be seen in the early postoperative phase, usually 1 to 4 weeks following surgery. The aseptic enhancement sometimes seen along the posterior disc or within the nerve root early on is typically reactive in nature and can be a diagnostic pitfall. Edema and enhancement may also be seen in the vertebral body and disc space in asymptomatic patients early in the postoperative course. Therefore, clinical presentation is key to better understanding early postoperative changes.
Presence of osseous erosive changes, soft tissue abscess, or phlegmon formation increases the sensitivity of MRI to hardware infection. The causes of infection may be intraoperative seeding, hematogenous seeding, or metal fretting. The risk of management includes antibiotics and surgical removal of the infected hardware.
References: Malhotra A, Kalra VB, Wu X, et al. Imaging of lumbar spinal surgery complications. Insights Imaging 2015;6(6):579-590.
Viola RW, King HA. Delayed infection after elective spinal instrumentation and fusion: a retrospective analysis of eight cases. Spine 1997;22(20):P2444-P2450.
2 A 42-year-old male with seizures was found down and brought to the ER.
|
2a Which of the following imaging features seen on this image is highly concerning and warrants further evaluation?
A. Sacroiliac joint sclerosis
B. Intraosseous gas
C. Surrounding soft tissue stranding
D. Osteophytosis
Additional workup included an MRI with contrast. Key images are provided below.
|
View Answer
2a Answer B. Intraosseous gas. Presence of intraosseous gas raises concern for emphysematous osteomyelitis, particularly given lack of contiguity with the joint space.
2b What is the most likely diagnosis?
A. Multifocal bone infarction
B. Intraosseous pneumatocysts
C. Metastasis
D. Emphysematous osteomyelitis
View Answer
2b Answer D. Emphysematous osteomyelitis. The abnormal enhancement and intraosseous collections are concerning for emphysematous osteomyelitis.
Imaging Findings: Figure 1. Noncontrast CT scan through the pelvis demonstrates intraosseous gas (arrows).
Figure 2. Postcontrast fat-suppressed axial T1w image shows abnormal soft tissue enhancement and multifocal intraosseous (solid arrows) and intramuscular abscesses (dotted arrows). The constellation of findings is concerning for emphysematous osteomyelitis.
Discussion: Emphysematous osteomyelitis is a rare but severe infection that is characterized by presence of intraosseous gas. The intraosseous gas seen with this entity is not in the typical distribution abutting the endplates as seen with degenerative disease and can involve both the axial and appendicular skeletons. Anaerobic organisms such as Fusobacterium necrophorum and Clostridium septicum and gram-negative Enterobacteriaceae family are typically implicated as common causative organisms. These patients commonly have other comorbidities such as diabetes or malignancy predisposing to this infection. Nearly every bone can be affected; however, most cases affect the vertebra, sacrum, and long bones.
Differential Diagnosis: Bone infarction, which usually presents as a serpentine contour of infarction with peripheral enhancement; however, soft tissue involvement will not be seen with this condition as noted in the presented case. Bony infarction is usually associated with steroids, sickle cell disease, pancreatitis, vasculitis, emboli, and caisson disease. Degenerative intraosseous pneumatocysts can be considered; however, those are usually abutting the sacroiliac joint and will also not have associated soft tissue changes.
References: Chen JLY, Huang YS. Emphysematous osteomyelitis of spine. QJM 2016;109(6):427-428.
Larson J, Muhlbauer J, Wigger T, et al. Emphysematous osteomyelitis. Lancet Infect Dis 2015;15(4):486.
3 A 47-year-old female presented with chronic back pain and right thigh pain. An MRI was performed. Key images are shown below.
|
3a What is the most likely diagnosis?
A. Metastases with right psoas involvement
B. Discitis/osteomyelitis with a right psoas abscess
C. Modic type 1 endplate changes and right psoas hematoma
D. Retroperitoneal fibrosis and secondary endplate changes
View Answer
3a Answer B. Discitis/osteomyelitis with a right psoas abscess. There is edema and enhancement involving the endplates of L4 and L5 is suggestive of an infectious process with a focal right psoas abscess. Paravertebral psoas abscesses should prompt a careful search for spinal infections. Infection and abscess formation in the iliopsoas is typically due to spread of infection from contiguous structures, most commonly bone, kidney, bowel, and appendix.
3b What is the most common pathology in the iliopsoas compartment?
A. Primary neoplasm (liposarcoma, fibrosarcoma)
B. Retroperitoneal hematoma
C. Abscess
D. Retroperitoneal fibrosis
View Answer
3b Answer B. Retroperitoneal hematoma. Iliopsoas is the most common site for a spontaneous retroperitoneal hemorrhage either secondary to anticoagulation or a bleeding diathesis. The MR appearance of the hematoma is variable, depending on the age of the hematoma.
|
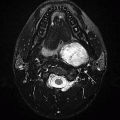
Imaging Findings: Postcontrast axial images through the lumbar spine demonstrate collection within the right psoas muscle concerning for a soft tissue phlegmon/developing abscess (A).
On the sagittal STIR, marrow edema is seen within L4 and L5 vertebral bodies and mild edema along anterior disc and prevertebral soft tissues (dotted arrow). Also note that preexisting Modic type 2/3 (type 2, yellow marrow conversion, and type 3, subchondral sclerosis) endplate changes can often partially obscure the presence of edema. These findings are consistent with discitis/osteomyelitis with right psoas involvement.
Discussion: Infection and abscess formation in the iliopsoas are typically secondary to spread of infection from contiguous structures. Common bowel sources of an iliopsoas infection include diverticulitis, Crohn disease, and appendicitis. Renal sources include pyelonephritis or renal/perirenal abscess. It is important to look for secondary features of infection such as fat stranding, blurring of the fat planes, and ectopic gas.
Primary infection is rare unless the patient is immunocompromised or a user of intravenous drugs, in which case the infection is usually due to Staphylococcus aureus and mixed gram-negative organisms. Primary neoplasms such as liposarcoma, fibrosarcoma, or hemangiopericytoma rarely originate from the iliopsoas compartment. A psoas abscess can lead to significant morbidity and mortality. Risk factors include advanced age, bacteremia, and inadequate treatment.
Differential Diagnosis: The most common differential diagnoses are hematoma, which can have a variable appearance dependent on the age of the hematoma. Neoplasms such as lymphoma, melanoma, or metastasis can be considered and may involve the psoas compartment.
References: Chern CH, Hu SC. Psoas abscess: making an early diagnosis in the ED. Am J Emerg Med 1997;15(1):83-88.
Muckley T, Schutz T, Kirschner M, et al. Psoas abscess: the spine as a primary source of infection. Spine 2003;28(6):E106-E113.
4 A 54-year-old male presents with low-grade fever, sweats, low back pain, and possible new cardiac murmur.
|
4a What is the most likely diagnosis in the current clinical scenario?
A. Rheumatoid arthritis
B. Metastasis
C. Facet joint septic arthritis
D. Modic type 1 degenerative changes
View Answer
4a Answer C. Facet joint septic arthritis. Postcontrast T1 and STIR images demonstrate a small collection and increased STIR signal abnormality within the L4-L5 facet joint, consistent with septic facet joint.
4b Which of the following is the most common organism associated with this entity?
A. Staphylococcus aureus
B. Streptococcus
C. Clostridium difficile
D. E. coli
View Answer
4b Answer A. Staphylococcus aureus. Staphylococcus aureus is the offending organism in a majority of the cases. The next most common organism is Streptococcus.
|
Imaging Findings: Sagittal postcontrast T1w imaging demonstrates a nonenhancing fluid collection seen along the inferior aspect of the L4-L5 facet joint (A). Sagittal STIR demonstrates marrow and periarticular soft tissue edema (solid arrow, B) and paraspinal muscular edema (dotted arrow). Findings are suggestive of septic facet arthritis in the given clinical scenario.
Discussion: The most common cause is hematogenous contamination. Otherwise, infection can be acquired through direct inoculation from penetrating trauma, surgical intervention, or diagnostic procedures such as facet joint injections. It is also important to consider pelvic sources such as diverticulitis/appendicitis, or IBD. Predisposing factors include immunosuppression, IVDU, and diabetes. Secondary complications to be aware of are epidural extension of infection resulting in cord compression and neuroforaminal narrowing. Intrathecal spread of infection could lead to meningitis/arachnoiditis.
Differential Diagnosis: Facet joint osteoarthritis and rheumatoid arthritis. Particularly, facet joint synovial cyst can often exist in the setting of advanced degenerative changes and pedicle stress reaction. This creates a diagnostic dilemma because of morphologic overlap with septic arthritis; however, findings such as rim enhancement and clinical features of infection favor septic arthritis.
References: Heenan SD, Britton J. Septic arthritis in a lumbar facet joint: a rare cause of an epidural abscess. Neuroradiology 1995;37:462-464.
Michel-Batot C, Dintinger H. A particular form of septic arthritis: septic arthritis of the facet joint. Joint Bone Spine 2008;75(1):78-83.
5 A 61-year-old male, newly immigrated from Brazil presents with focal back tenderness, weakness, and low-grade fever.
|
5a A CT of the chest was performed with contrast; key finding is shown above. What is the next best step?
A. Bone scan
B. MRI of the spine
C. Antibiotics
D. Surgery
View Answer
5a Answer B. MRI of the spine. Given the patient’s symptoms and paraspinal soft tissue thickening, it is important to determine intrathecal involvement. An MRI will also provide superior soft tissue detail and asses for osseous involvement.
A. Pyogenic osteomyelitis
B. Tuberculous spondylitis
C. Metastasis
D. Modic type 1 changes
View Answer
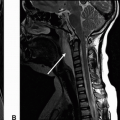
5b Answer B. Tuberculous spondylitis. Tuberculous spondylitis (TS) often presents with hyperintense marrow, disc, phlegmon/abscess on the STIR, and marrow enhancement. There is usually sparing of the intervertebral disc.
Imaging Findings: Figure 1. Postcontrast axial CT scan through the aortic arch demonstrates paraspinal soft tissue thickening.
Figure 2. Axial postcontrast T1s images shows paravertebral abscess and enhancement (A). Sagittal STIR shows subligamentous phlegmon seen along the anterior cortices (B).
Discussion: Tuberculous spondylitis, otherwise known as Pott disease, is one of the oldest known diseases. An inoculum is initially introduced along an anterior vertebral body with spread through lymphatics, commonly from pulmonary origin. It can be distinguished from pyogenic osteomyelitis where the initial infection is in the subchondral bone adjacent to the endplate and the intervertebral discs are typically affected. Furthermore, tuberculous spondylitis is more common in the thoracic spine, likely given its proximity to the pulmonary source. Current treatment modalities are highly effective against TS, particularly in the absence of severe deformity or neurologic deficit. Early diagnosis is essential to prevent significant morbidity due to progressive bone destruction, kyphotic deformity, and risk of developing paraplegia.
Differential Diagnosis: Differential diagnosis includes fungal osteomyelitis and brucellar spondylitis, both of which may be indistinguishable from tuberculous spondylitis.
References: Kilzilbash QF, Seaworth BJ. Multi-drug resistant tuberculous spondylitis. Ann Thorac Med 2016;11(4):233-236.
Smith AS, Weinstein MA, Mizushima A, et al. MR imaging characteristics of tuberculous spondylitis vs vertebral osteomyelitis. AJNR Am J Neuroradiol 1989;10:619-625.
6 A 63-year-old male with history of meningitis/encephalitis presenting with 3 days of progressive numbness and weakness. An MRI of the lumbar spine was performed; key images are shown below.
|
6a Which of the following key abnormalities is noted on these images?
A. Nerve root clumping
B. Normal enhancement
C. Subdural hemorrhage
D. All of the above
View Answer
6a Answer A. Nerve root clumping. The images demonstrates nerve root clumping and abnormal enhancement that is often associated with arachnoiditis. This is caused by irritation and inflammation of the arachnoid matter resulting in abnormal adhesions of the nerve roots to each other and to the surface of the thecal sac.
6b Which of the following is most likely to result in arachnoiditis?
A. Tumor
B. Surgery
C. Demyelination
D. Advanced degenerative change
View Answer
6b Answer B. Surgery. Historically, arachnoiditis has been associated with trauma and infection. In modern times, however, lumbar spine surgery is the most common cause.
|
Imaging Findings: Sagittal T2 and pre- and postcontrast T1w images (A-C) and two axial T2WI (D, E) of the lumbar spine show abnormal clumping and enhancement of the cauda equina nerve roots. On the more inferior axial image (E), the nerve roots are adherent to the posterior wall of the thecal sac, giving the impression of absent nerve roots, the so-called empty sac sign.
Discussion: Arachnoiditis is caused by any process that causes inflammation of the arachnoid layer such as infection, trauma, hemorrhage, or intrathecal injection of some substances. It often results in chronic irreversible clumping and tethering of the nerve roots to each other or the surface of the thecal sac. It can occur anywhere along the spine, but is most commonly observed in the lumbar spine with distinctive appearance of the cauda equina nerve roots. Arachnoiditis can also result in the formation of loculated CSF collections that are trapped as a result of adhesions. Restriction of movement and clumping of the nerve roots and leptomeningeal inflammation may present as back or leg pain or less commonly other neurologic deficits such as paresis, paresthesia, or loss of bowel/bladder control. In some cases, the inflammatory changes can calcify leading to “arachnoiditis ossificans.” No effective treatment is available. Differential diagnosis includes severe spinal stenosis, carcinomatous meningitis, and some intradural masses.
References: Delamarter RB, et al. Diagnosis of lumbar arachnoiditis by magnetic resonance imaging. Spine 1990;15(4):304-310.
Ross JS, et al. MR imaging of lumbar arachnoiditis. AJR Am J Roentgenol 1987;149:1025-1032.
7 A 39-year-old man recently recovered from an upper respiratory tract infection presents with bilateral lower extremity weakness and difficulty breathing. An MRI with contrast was performed. Key images are shown below.
|
7a What is the most likely diagnosis in the given clinical scenario?
A. Lymphoma
B. Metastasis
C. Guillain-Barre syndrome
D. Transverse myelitis
View Answer
7a Answer C. Guillain-Barre syndrome. Ascending weakness shortly after a viral illness with imaging features of smooth diffuse nerve root thickening and enhancement is highly suggestive of acute inflammatory demyelinating polyradiculoneuropathy (AIDP) or Guillain-Barre syndrome.
7b Which of the following best describes the underlying pathophysiology for the above entity?
A. Autoimmune demyelination
B. Bacterial infection
C. Drop metastases
D. Granulomatous inflammation
View Answer
7b Answer A. Autoimmune demyelination. The pathologic mechanism for Guillain-Barre syndrome is thought to be autoimmune and related to cross-reactive antibodies against myelin; hence, the effectiveness of plasma exchange or intravenous immunoglobulin (IVIG) as treatment strategies.
|
Imaging Findings: Sagittal pre- (A) and postcontrast (B) T1WI of the lumbar spine show smooth enhancement of the cauda equina nerve roots. Axial T2WI (C) and postcontrast T1WI (D) of the cauda equina show slight thickening and avid enhancement of all visualized nerve roots.
Discussion: Acute inflammatory demyelinating polyradiculoneuropathy (AIDP) or Guillain-Barre syndrome is an autoimmune demyelinating disease that is often triggered by circulating antibodies to a recent infection (most commonly respiratory or gastrointestinal). The affected individuals are typically children or young adults without a gender predilection. The disease presents as ascending weakness and can involve the respiratory muscles and the cranial nerves. In addition to supportive care, plasma exchange and IVIG have been found to be effective therapies. However, the disease has a variable course, and, depending on severity, full recovery might take weeks or months. In a minority of cases, the disease may become chronic. In some severe cases, death has been reported.
On imaging of the spine, the most common presentation is mild smooth thickening and enhancement of multiple cauda equina nerve roots and pial enhancement of the conus medullaris. The morphology and signal intensity of the spinal cord are preserved. Although nerve root enhancement is not specific to Guillain-Barre, enhancement of only the anterior nerve roots is strongly suggestive of this disease.
Differential Diagnosis: The imaging differential diagnosis includes lymphoma, metastatic disease, infection, chronic polyneuropathies, postradiation effects, etc. Clinical history and lumbar puncture provide valuable information for narrowing the differential spectrum.
References: Byun WM, et al. Guillain-Barre syndrome: MR imaging findings of the spine in eight patients. Radiology 1998;208:137-141.
Yuki N, Hartung HP. Guillain-Barre syndrome. N Engl J Med 2012;366:2294-2304.
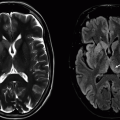
8 A 59-year-old woman presenting with new sensory changes in bilateral arms. Patient had a previous similar episode that spontaneously resolved 6 months ago. An MRI was performed; key images are below.
|
8a What is the most likely diagnosis?
A. Multiple sclerosis
B. Transverse myelitis
C. Guillain-Barre syndrome
D. Glioma
View Answer
8a Answer A. Multiple sclerosis. There are multifocal brain and cord lesions along with an enhancing lesion in the cervical cord, compatible with multiple sclerosis with evidence of dissemination in space (DIS) and time (DIT).
8b Which of the following imaging features is compatible with dissemination in space for multiple sclerosis?
A. Presence of enhancement
B. Simultaneous periventricular and cord lesions
C. Involvement of the dorsal column cervical cord
D. Multiple lesions perpendicular to the callososeptal junction
View Answer




8b Answer B. Simultaneous periventricular and cord lesions. Periventricular and infratentorial or cord lesions are classified as DIS. Although presence of enhancing or new lesion is classified as DIT, it is not a criterion for DIS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree