Spine Neoplasms, Spine and Neck Vascular Diseases
Jonathan Youngsuk Kim
Archana Siddalingappa
Lidia Mayumi Nagae
Rafael Rojas
Prachi Dubey
Rafeeque Bhadelia
QUESTIONS
A. Hemangioma
B. Osteomyelitis
C. Neoplasm
D. Aneurysmal bone cyst
View Answer
1 Answer C. Neoplasm. There is an expansile vertebral body mass that extends into the anterior epidural space, most likely neoplastic in etiology.
2 Which of the following lesions is the most common malignancy of the spine?
A. Chondrosarcoma
B. Chordoma
C. Metastasis
D. Osteosarcoma
View Answer
2 Answer C. Metastasis.
|
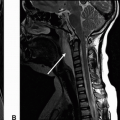
Imaging Findings: Images demonstrate a pathologic compression deformity of the L1 vertebral body with a highly T2 hyperintense (C), T1 hypointense (A), and mildly enhancing lesion (B), replacing the entirety of the vertebral body with epidural extension and resultant cord compression.
Discussion: Metastatic disease, myeloma, and lymphoproliferative tumors are the most common malignant spinal tumors. These usually present with multiple lesions. In case of solitary lesions, one must consider lesions such as plasmacytoma, Ewing sarcoma and chordoma. Chordoma, although quite rare, remains the most common primary malignancy of spine in adults after lymphoproliferative lesions and myeloma. It arises from cells of the primitive notochord and thus can arise from the bone anywhere in the axial skeleton from Rathke pouch to the coccyx. Cases typically are most common in the sacrococcygeal region followed by the clivus and then the vertebral bodies. Though chordomas are locally aggressive, they metastasize relatively infrequently, roughly 15% of the time. Chordomas are treated with surgical resection and radiation therapy with gross total resection having a better prognosis.
Differential Diagnosis: Unfortunately, the imaging appearance of chordoma can be quite nonspecific and the differential would include metastasis, lymphoproliferative disorder/plasmacytoma, chondrosarcoma, and giant cell tumor.
References: Ha AS, Chew FS. Imaging of sacral masses: self-assessment module. AJR Am J Roentgenol 2010;195:S32-S36.
Murphey MD, Andrews CL, Flemming DJ, et al. From the archives of the AFIP. Primary tumors of the spine: radiologic pathologic correlation. Radiographics 1996;16:1131-1158.
Nishiguchi T, Mochizuki K, Ohsawa M, et al. Differentiating benign notochordal cell tumors from chordomas: radiographic features on MRI, CT, and tomography. AJR Am J Roentgenol 2011;196:644-650.
3 A 72-year-old woman presenting with right lower extremity weakness.
|
3a What is the next best step in evaluation?
A. No further evaluation
B. CT with contrast
C. MRI with contrast
D. MRI without contrast
An MRI with contrast was performed. Key images are shown below:
|
View Answer
3a Answer C. MRI with contrast. Although a partially calcified mass of the spinal canal is clearly evident on the CT images, MRI with contrast is indicated for further evaluation given superior soft tissue contrast and also to evaluate the relationship of the mass to the spinal cord.
3b What is the most likely diagnosis?
A. Meningioma
B. Metastasis
C. Schwannoma
D. Paraganglioma
View Answer
3b Answer A. Meningioma. All choices are reasonable differential etiologies, however given intradural, extramedullary location, well-defined borders, broad-based dural attachment, calcifications, and relatively homogenous enhancement, meningioma is most likely. Meningioma is overall the second most common intradural, extramedullary lesion in the spine, with the thoracic spine being the most common location.
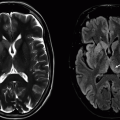
Imaging Findings: Figure 1. This figure shows a sagittal CT of the thoracic spine demonstrating a partially calcified lesion within the spinal canal at the midthoracic level.
Figure 2. This figure shows sagittal T2, T1, and T1 postcontrast images demonstrating a T1 and T2 intermediate intradural extramedullary lesion with areas of low signal corresponding to calcification, a broad-based dural attachment, and relatively homogenous postcontrast enhancement. There is significant displacement and compression of the adjacent spinal cord.
Discussion: Spinal meningioma is the second most common intradural extramedullary spinal neoplasm after schwannoma and is more common in women and elderly. Extradural or mixed location is possible, though much less common. Within the spine, meningioma is most common in the thoracic spine, followed by the cervical spine, and is rarely seen in the lumbosacral spine.
Most lesions are isolated, and when multiple lesions are seen, neurofibromatosis type 2 should be suspected. Imaging findings are generally identical to intracranial meningioma, with a dural-based, homogeneously enhancing lesion with calcifications being common. Like within the intracranial compartment, a dural tail and adjacent hyperostosis can be seen, though less common. Total surgical resection is generally curative, and recurrence is uncommon.
Differential Diagnosis: The primary differential etiology is nerve sheath tumor, though other possibilities include other intradural extramedullary lesions such as ependymoma or metastasis.
References: De Verdelhan O, Haegelen C, Carsin-Nicol B, et al. MR imaging features of spinal schwannomas and meningiomas. J Neuroradiol 2005;32:42-49.
Lee JW, Lee IS, Choi KU, et al. CT and MRI findings of calcified spinal meningiomas: correlation with pathological findings. Skeletal Radiol 2010;39:345-352.
4 A 35-year-old man presents with lower back pain and lower extremity radiculopathy.
|
4a What is the most likely diagnosis?
A. Meningioma
B. Schwannoma
C. Myxopapillary ependymoma
D. Chordoma
View Answer
4a Answer C. Myxopapillary ependymoma. This is the most common intradural extramedullary lesion of the cauda equina/filum terminale and is thus the most likely diagnosis in this case. Though imaging findings are nonspecific, hemorrhagic component and calcification, shown here, are commonly seen in myxopapillary ependymoma.
4b Which of the following anatomic location best characterizes this lesion?
A. Intradural, extramedullary
B. Intramedullary
C. Extradural
D. Presacral
View Answer
4b Answer A. Intradural, extramedullary. The lesion in question is intradural, extramedullary in location, which is most common for myxopapillary ependymoma. The other locations are possible, but far less likely.
|
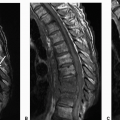
Imaging Findings: Images demonstrate a large, lobulated T2 hyperintense (A), largely homogeneously enhancing (C), intradural extramedullary mass at the lumbosacral junction. There are areas of low T2 signal suggesting hemorrhage and calcification, respectively. There is scalloping of the adjacent posterior vertebral bodies (A-C).
Discussion: Myxopapillary ependymoma is a low-grade variant of ependymoma that is limited to the conus medullaris/filum terminale and is also the most common malignancy in this location in adults. This variant has a younger age of presentation in the 30s as compared to other ependymoma subtypes and demonstrates a slight male predominance.
Differential Diagnosis: Imaging features can be difficult to distinguish from other lesions such as schwannoma or paraganglioma in the intradural location. Depending on the level of involvement, it can also be difficult to distinguish between other entities such as chordoma or giant cell tumor. However, hemorrhage is more common in myxopapillary ependymoma. As a low-grade tumor, outcomes are generally good with total surgical resection. However, in a minority of cases, the lesion can disseminate through CSF and multiple lesions can be seen.
References: Abul-Kasim K, Thurnher MM, McKeever P, et al. Intradural spinal tumors: current classification and MRI features. Neuroradiology 2008;50:301-314.
Ha AS, Chew FS. Imaging of sacral masses: self-assessment module. AJR Am J Roentgenol 2010;195:S32-S36.
Shors SM, Jones TA, Jhaveri MD, et al. Myxopapillary ependymoma of the sacrum. Radiographics 2006;26:S111-S116.
Wippold FJ, Smirniotopoulos JG, Moran CJ, et al. MR imaging of myxopapillary ependymoma: findings and value to determine extent of tumor and its relation to intraspinal structures. AJR Am J Roentgenol 1995;165:1263-1267.
A. Meningioma
B. Abscess
C. Nerve sheath tumor
D. Perineural root sleeve cyst
View Answer
5a Answer C. Nerve sheath tumor. Well-circumscribed T2 hyperintense mass centered in the neural foramen with bony expansion is most consistent with a diagnosis of nerve sheath tumor. Based on appearance, it would be impossible to distinguish between neurofibroma and Meningioma is a reasonable differential diagnosis, though is the second most common intradural extramedullary spinal lesion behind nerve sheath tumors. Abscess is unlikely given the lack of a clear source and lack of surrounding inflammatory change. Perineural root sleeve cyst is also excluded as this lesion demonstrates enhancement.
5b Multiple cutaneous lesions are also seen. Which of the following is the most likely underlying disorder?
A. Tuberous sclerosis
B. Neurofibromatosis type 1
C. Neurofibromatosis type 2
D. Von Hippel-Lindau syndrome
View Answer
5b Answer B. Neurofibromatosis type 1. Given the presence of a likely nerve sheath tumor and cutaneous lesion the patient most likely has neurofibromatosis type 1. Neurofibromatosis type 2 lacks the cutaneous lesions and is associated with intracranial schwannomas as well as meningioma and spinal ependymoma.
|
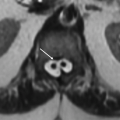
Imaging Findings: Images demonstrate a well-circumscribed, lobulated T2 hyperintense lesion, (arrow A) with heterogeneous enhancement, (arrow B and C) centered in the right C1-C2 neural foramen (arrow D and E).
Discussion: Nerve sheath tumors are benign neoplasms and constitute the most common primary intradural extramedullary spinal lesion. Purely extradural or mixed intradural and extradural location can be seen but is less common. Nerve sheath tumors include both schwannoma and neurofibroma, though these entities largely cannot be distinguished from one another by imaging characteristics alone. Nerve sheath tumors typically arise from the dorsal root ganglion, and thus affected patients present more often with pain rather than weakness.
Neurofibromas have an association with neurofibromatosis type 1 and multiple lesions are common. Neurofibromas tend to grow encasing a nerve root and sometimes a target sign suggesting this can be seen, though this is nonspecific and can also be seen in schwannoma. Although neurofibromas are a benign lesion, a minority (˜10%) can undergo malignant transformation into neurofibrosarcoma.
Spinal schwannomas have an association with neurofibromatosis type 2. When present, hemorrhage and cystic degeneration is a more common finding in schwannoma rather than neurofibroma and may suggest toward a specific diagnosis, though these can be seen in both entities. As compared to neurofibroma, schwannomas almost never undergo malignant degeneration.
For either lesion, surgical excision is considered curative, though recurrence is more common when these lesions occur in the background of neurofibromatosis type 1/2.
References: Abul-Kasim K, Thurnher MM, McKeever P, et al. Intradural spinal tumors: current classification and MRI features. Neuroradiology 2008;50:301-314.
De Verdelhan O, Haegelen C, Carsin-Nicol B, et al. MR imaging features of spinal schwannomas and meningiomas. J Neuroradiol 2005;32:42-49.
Mautner VF, Tatagiba M, Lindenau M, et al. Spinal tumors in patients with neurofibromatosis type 2: MR imaging study of frequency, multiplicity, and variety. AJR Am J Roentgenol 1995;165:951-955.
6 A 55-year-old man presenting with lower back pain.
|
6a What imaging finding is seen in this case that suggests a specific diagnosis?
A. Cap sign
B. Flow voids
C. Target sign
D. Curtain sign
View Answer
6a Answer B. Flow voids. Scattered flow voids are seen especially on the sagittal T2 sequence, which is suggestive of paraganglioma. Cap sign refers to a rim of T2 hypointensity or susceptibility artifact denoting hemorrhage, which is nonspecific and can be seen in both ependymoma and paraganglioma. The target sign refers to a targetoid appearance of neurofibroma on T2 imaging with a bright rim and dark core. Curtain sign refers to the appearance of a vertebral body lesion with anterior epidural extension, which causes a bilobed uplifting of the posterior longitudinal ligament.
6b Given the imaging findings, what is the most likely diagnosis?
A. Lymphoma
B. Hematoma
C. Meningioma
D. Paraganglioma
View Answer
6b Answer D. Paraganglioma. The presence of flow voids in this case is most suggestive of paraganglioma.
|
Imaging Findings: Images demonstrate a relatively well-defined, homogeneously enhancing, extramedullary, intradural mass centered at the level of L5. Axial T2 images demonstrate scattered, punctate areas of low signal suggestive of flow voids (arrow in D and E).
Discussion: Spinal paraganglioma is a neuroendocrine tumor, which is histologically identical to paraganglioma at any other site, and can occur at any location where there are paraganglion cells such as the adrenal gland (pheochromocytoma), paravertebral station, and head and neck (glomus tumors).
Spinal paraganglioma is rare, with most cases of paraganglioma being adrenal in origin and the majority of extra-adrenal cases being located in the head and neck. Despite its rarity, paraganglioma should be considered in the differential along with the more common entities of schwannoma or ependymoma as outcomes are dependent on totality of surgical resection and as these tumors are considered insensitive to radiation therapy. However, complete surgical resection is usually curative, and recurrence after resection is uncommon (<5%).
Differential Diagnosis: Includes schwannoma, neurofibroma, ependymoma, and meningioma.
References: Mishra T, Goel NA, Goel AH. Primary paraganglioma of the spine: a clinicopathological study of eight cases. J Craniovertebr Junction Spine 2014;5:20-24.
Sahdev A, Sohaib A, Monson JP, et al. CT and MR imaging of unusual locations of extra-adrenal paragangliomas (pheochromocytomas). Eur Radiol 2005;15:85-92.
Sundgren P, Annertz M, Englund E, et al. Paragangliomas of the spinal canal. Neuroradiology 1999;41:788-794.
7 A 15-year-old male presents with back pain. Key images are shown below:
|
7a What is the most likely etiology of this lesion?
A. Traumatic
B. Infectious
C. Benign tumor
D. Malignant tumor
View Answer
7a Answer C. Benign tumor. Nidus with surrounding edema is classic appearance of osteoid osteoma, a benign tumor.
7b Which of the following is a typical clinical presentation seen with this entity?
A. Sports injury
B. Night pain relieved with aspirin
C. Intravenous drug use
D. Known primary malignancy
View Answer
7b Answer B. Night pain relieved with aspirin. Patients with osteoid osteoma present with night pain relieved by aspirin, NSAIDs. Some patients have scoliosis related to muscle spasm.
|
Imaging Findings: Axial and sagittal CT images at L5 demonstrate a central nidus with variable amount of ossification. The nidus measures <1.5 cm. There is dense sclerosis around the tumor (A and B). Axial T2 (C) and postcontrast T1 axial (D) images demonstrate a rounded T2 hypointense nidus with surrounding T2 hyperintense edema and enhancing reactive zone.
Discussion: Osteoid osteoma is a benign osteoid-producing tumor. It is an important cause of painful scoliosis in a child or young adult. The most common symptom is night pain relieved by aspirin or other NSAIDs. The majority of the lesions are found in the lumbar spine. The best diagnostic feature is a small radiolucent tumor nidus with surrounding sclerosis. The nidus is typically <1.5 cm; the larger lesions are called osteoblastoma. The surrounding sclerosis represents reactive edema because of prostaglandin release and can be hyperintense on T2 with contrast enhancement. The nidus can show variable T2 signal but typically demonstrate avid and rapid enhancement. Complete resection of the nidus is curative in most cases. Other treatment options include thermo-/photocoagulation.
Differential Diagnoses: osteoblastoma (similar to osteoid osteoma, but larger than 1.5 cm and expansile) and stress fracture (fracture line rather than a rounded nidus, and pain related to activity). Osteomyelitis (sequestrum or focal abscess can mimic nidus but tend to be irregular shape; usually adjacent osseous erosion or destruction is present). Ewing sarcoma (no nidus, centered in the vertebral body, with diffuse surrounding edema).
References: Assoun J, et al. Osteoid osteoma: MR imaging versus CT. Radiology 1994;191(1):217-223.
Chai JW, et al. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics 2010;30(3):737-749. Erratum in: Radiographics 2010;30(4):1156.
Greenspan A. Benign bone-forming lesions: osteoma, osteoid osteoma, and osteoblastoma. Clinical, imaging, pathologic, and differential considerations. Skeletal Radiol 1993;22(7):485-500.
Woods ER, et al. Reactive soft-tissue mass associated with osteoid osteoma: correlation of MR imaging features with pathologic findings. Radiology 1993;186(1):221-225.
8 A 67-year-old male presents with severe lower extremity weakness and urinary incontinence. Key images from an MRI are shown below:
|
8a What is the salient imaging finding seen in this patient?
A. Nerve root enhancement and thickening
B. Phlegmon and inflammation
C. Endplate cortical erosion
D. Vertical fracture of the vertebral body
8b What is the most likely diagnosis?
A. Campylobacter viral infection with GI symptoms
B. Leptomeningeal metastasis
C. Demyelinating disease
D. Arachnoiditis
View Answer
8b Answer B. Leptomeningeal metastasis. This should be the most likely diagnosis given the nodular enhancing and thickened appearance of nerve roots.
|
Imaging Findings: T1 sagittal and axial postcontrast images demonstrate thickening and diffuse enhancement of the cauda equine nerve roots with nodular enhancing foci (A and B). Note diffusely abnormal marrow signal compatible with osseous metastatic disease.
Discussion: Metastases from central nervous system malignancies generally occur at a younger age and include medulloblastoma, choroid plexus neoplasms, glioblastoma, and ependymoma, among other entities. In adults, the most common non-CNS solid tumors to present with leptomeningeal metastasis are lung and breast cancer, although lymphoma can also have such presentation. MRI with contrast is the imaging modality of choice, demonstrating thickened nerve roots with enhancing nodules on the spinal cord, nerve roots, or cauda equina, with a “sugar-coating” appearance of the spinal cord. Cord edema may be seen if there is an intramedullary component.
Differential Diagnosis: Differential diagnosis for diffuse nodular enhancement (sugar coating) include arachnoiditis and Guillain-Barré syndrome. Arachnoiditis will demonstrate clumping of nerve roots, “empty sac sign,” and often history of prior surgery. Guillain-Barré syndrome tends to show smooth pial enhancement of the cauda equina and conus medullaris in a patient with a history of recent viral illness.
References: Brant WE, Helms CA. Fundamentals of diagnostic radiology. Philadelphia, PA: Lippincott Williams & Wilkins, 2006. ISBN: 0781765188.
Grossman RI, Yousem DM. Neuroradiology, the requisites. Mosby Inc., 2003.
Soderlund KA, Smith AB, Rushing EJ, et al. Radiologic-pathologic correlation of pediatric and adolescent spinal neoplasms: Part 2, Intradural extramedullary spinal neoplasms. AJR Am J Roentgenol 2012;198(1):44-51.
9 Key images from an MRI performed for evaluation of a spinal mass are shown below.
|
9a What is the most likely diagnosis?
A. Hemangioblastoma
B. Meningioma
C. Metastasis
D. Astrocytoma
View Answer
9a Answer D. Astrocytoma. There is a mass with adjacent cysts and demonstrating strong enhancement, compatible with infiltrative astrocytoma.
9b Which of the following imaging features is characteristically associated with this entity?
A. Cyst with a nodule
B. Syringohydromyelia
C. Infiltrative and enhancing mass
D. Marginal cysts and peripheral hemorrhage
View Answer
9b Answer C. Infiltrative and enhancing mass. This feature strongly supports the diagnosis of an infiltrative astrocytoma.
|
Imaging Findings: T2 and T1 postcontrast sagittal images demonstrate a long-segment infiltrative mass with cord expansion and adjacent cysts (A and B). Postcontrast images demonstrate strong enhancement of the solid mass with nonenhancing cystic component (B). There is small amount of intratumoral hemorrhage (A, low T2 signal).
Discussion: Infiltrative astrocytomas of the spinal cord are the second most common spinal cord tumor in adults and most common spinal cord tumor in children. Astrocytomas are typically long multisegment intramedullary masses approximately 4 to 7 vertebral body segments in length. The most common location is the thoracic cord. Occasionally, there can be involvement of the entire spinal cord (holocord). In contrast to cord ependymomas, a cleavage plane is not present in most spinal astrocytomas. There is diffuse cord expansion, with eccentric location of the tumor within the spinal cord. There is extensive peritumoral edema. Intratumoral and peritumoral cysts are less common. Hemorrhage is uncommon and is more commonly seen with ependymomas.
Differential Diagnosis: The main differential diagnosis is spinal ependymoma. Ependymomas are more common in adults, are typically central in location, and occasionally demonstrate a hemorrhagic cap and larger polar and intratumoral cysts.
References: Brant WE, Helms CA. Fundamentals of diagnostic radiology. Philadelphia, PA: Lippincott Williams & Wilkins, 2007. ISBN: 0781761352.
Koeller KK, Rosenblum RS, Morrison AL. Neoplasms of the spinal cord and filum terminale: radiologic-pathologic correlation. Radiographics 2000;20(6):1721-1749.
Smith AB, Soderlund KA, Rushing EJ, et al. Radiologic-pathologic correlation of pediatric and adolescent spinal neoplasms: Part 1, intramedullary spinal neoplasms. AJR Am J Roentgenol 2012;198(1):34-43.
10 A 30-year-old male presents with gait ataxia and upper extremity motor weakness. Key images from an MRI are shown below:
|
10a What is the most likely cause for the brain findings?
A. Congenital
B. Inherited
C. Acquired
D. Cannot be determined
View Answer
10a Answer B. Inherited. Multiple tumors are seen demonstrating cyst and a nodule, compatible with hemangioblastomas. These are associated with von Hippel-Lindau, an inherited syndrome.
10b What is the most likely diagnosis?
View Answer
10b Answer C. Hemangioblastoma. This typically demonstrates a cyst and a mural nodule. Additional feature not seen on these images includes flow voids.
10c Based on additional findings shown above, what is the associated syndrome?
A. Tuberous sclerosis
B. Sturge-Weber
C. Von Hippel-Lindau syndrome
D. Neurofibromatosis 2
View Answer
10c Answer C. Von Hippel-Lindau syndrome. Both intracranial and spinal involvement of hemangioblastomas are seen with VHL.
Imaging Findings: Figure 1. Axial T2 and T1 postcontrast images demonstrate multiple cysts with mural nodules within the posterior fossa (A, B). T2w (C) and T1 postcontrast (D) images demonstrate a C4-C5 cystic lesion with a peripherally located mural nodule. There is adjacent peritumoral edema. An additional small enhancing nodule is seen posterior to C2 spinal cord.
Figure 2. Axial T2 of the pancreas demonstrates numerous pancreatic cysts. Note another small cystic focus in the spinal cord seen on the same image (dotted arrow), suggestive of hemangioblastoma.
Discussion: Hemangioblastomas are WHO grade 1 highly vascular tumors. Approximately 25% to 40% of hemangioblastomas occur in patients with von Hippel-Lindau (VHL), an autosomal dominant disease caused by chromosome 3p mutation. Patients with VHL have 2 or more CNS hemangioblastomas or 1 hemangioblastoma in addition to visceral lesion or retinal hemorrhage. Hemangioblastomas typically occur in young to middle-aged adults but earlier in patients with VHL. Spinal hemangioblastoma accounts for 3% to 13% of spinal cord tumors. The tumor usually demonstrates a cyst with a highly vascular mural nodule. Cysts are presumably part of the tumor and should be resected.
Differential Diagnosis: Differential diagnoses include metastasis (sold, rather than cyst and nodule), ependymoma (usually contain hemosiderin caps and peritumoral cysts along the cranial and caudal aspect), infiltrative astrocytoma (eccentric lesions that are long segments), and, for the posterior fossa, pilocystic astrocytoma (cyst with nodule but in children) and medulloblastoma (solid and restricted diffusion).
References: Grossman RI, Yousem DM. Neuroradiology, the requisites. Philadelphia, PA: Mosby Inc., 2003.
Ho VB, Smirniotopoulos JG, Murphy FM, et al. Radiologic-pathologic correlation: hemangioblastoma. AJNR Am J Neuroradiol 1992;13(5):1343-1352.
Slater A, Moore NR, Huson SM. The natural history of cerebellar hemangioblastomas in von Hippel-Lindau disease. AJNR Am J Neuroradiol 2003;24(8):1570-1574.
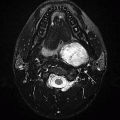
11 A 30-year-old female presents with carotidynia. Key image is shown below.
|
11a What is the most likely diagnosis?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree