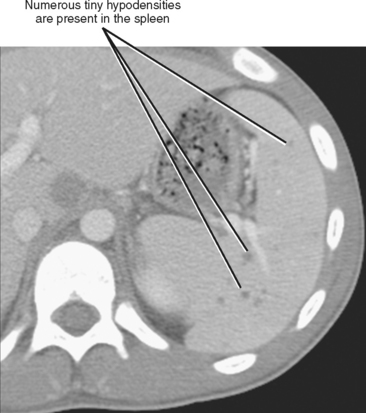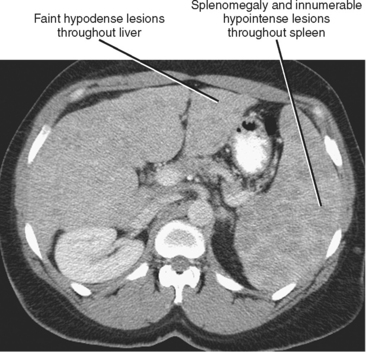
Figure 15-26 Enhanced axial computed tomographic scan through the upper abdomen of a patient with brucellosis.
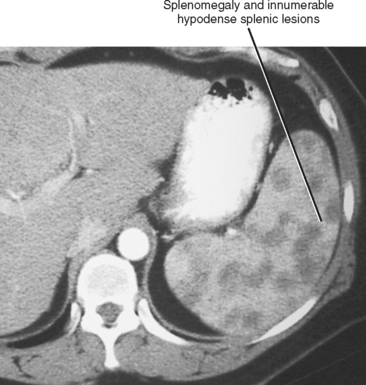
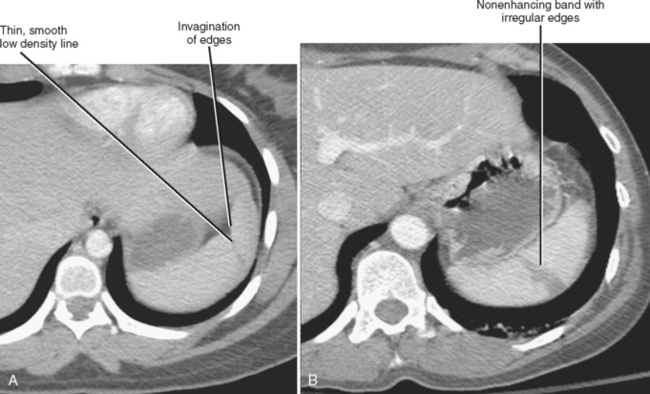
Figure 15-30 Enhanced axial computed tomographic through the upper abdomen of a patient with sarcoidosis.
CHAPTER 15 Spleen
“I don’t pay much attention to the spleen.” This quote from an abdominal imager acquaintance of mine typifies the opinion of many radiologists regarding the spleen. The spleen lacks the complex metabolism of the liver, the strategic location of the pancreas, and the crucial role of the kidneys. Most radiologists do not perceive splenic anatomy as particularly intricate. Primary malignant neoplasms of the spleen are rare, whereas incidental nonspecific splenic lesions are relatively common. No wonder the spleen is so maligned (or at least ignored).
ANATOMY
Splenic Size and Shape
The typical spleen measures less than 13 cm in length, up to 7 to 8 cm in width, and 4 cm in thickness. Normal splenic volume is usually less than 300 ml. The spleen generally has a smooth convex posterior, superior, and lateral surface. Splenic clefts are relatively common and may be confused with lacerations in the setting of trauma (Fig. 15-1). Unlike most lacerations, congenital clefts are sharply and smoothly marginated and not associated with perisplenic blood. Splenic bulges are common medially and may cause mass effect on the stomach or be mistaken for a splenic or renal mass.
Vascular Anatomy of the Spleen
The blood supply to the spleen is via the splenic artery, which travels in the splenorenal ligament with the splenic vein. The splenic artery creates many smaller arteries in addition to the terminal splenic branches, including several pancreatic branches, short gastric arteries (which travel in the gastrosplenic ligament), the left gastroepiploic artery, and occasionally a posterior gastric artery.
Accessory Splenic Tissue
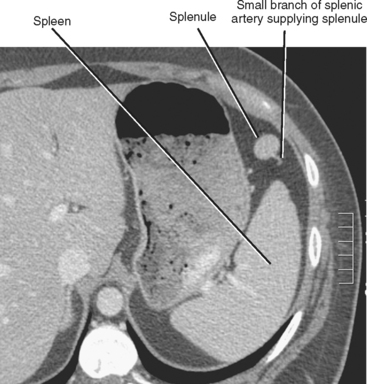
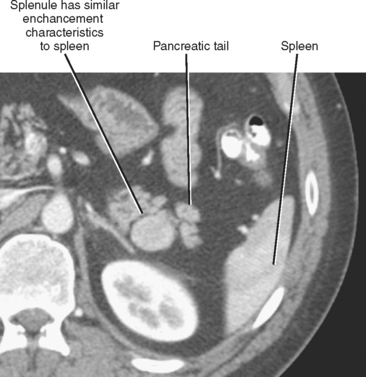
During development, several splenic islands coalesce within the dorsal mesogastrium. When some of these islands fail to join the bulk of the coalescing splenic tissue, accessory spleens or splenules result. Splenules are typically round, smooth, smaller than 2 cm, and functional. Despite being completely separate from the spleen, splenules share similar imaging characteristics with the normal spleen (Fig. 15-2). Occasionally, the branch of the splenic artery that supplies the splenule can be seen on imaging studies (Fig. 15-3). More than 95% of splenules are found in the splenorenal ligament (near or in the pancreatic tail), gastrosplenic ligament, splenic hilum, gastrocolic ligament, or greater omentum. However, accessory spleens have been localized as far away as the pelvis, and they are occasionally mistaken for adrenal, pancreatic, and peritoneal tumors (Fig. 15-4). Accessory spleens rarely reside lateral to the main spleen.
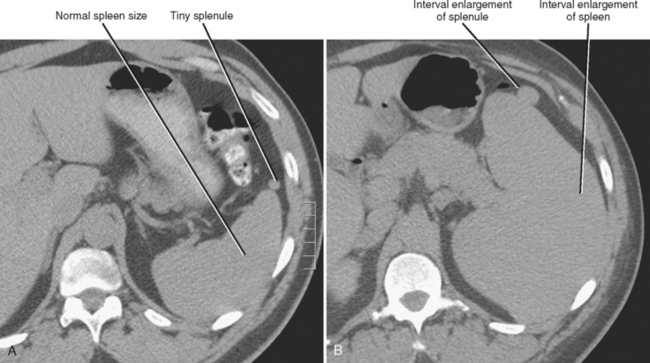
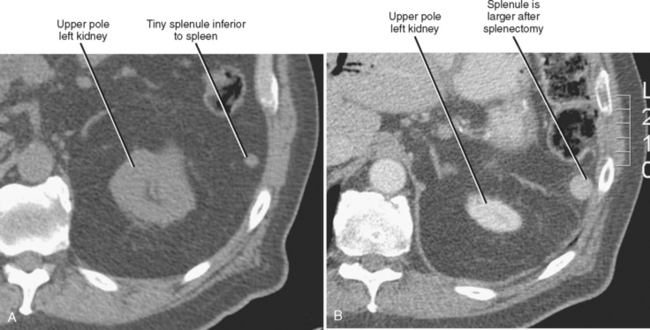
Pathologic processes that affect the spleen may also involve splenules (Fig. 15-5). Accessory spleens are important to identify before surgery in patients undergoing splenectomy for such disorders as idiopathic thrombocytopenic purpura. Failure to prospectively identify and remove accessory spleens in such a setting may result in return of hypersplenism. After splenectomy, residual accessory spleens often enlarge (Fig. 15-6). Accessory spleens may occasionally undergo torsion, infarction, or spontaneous rupture.
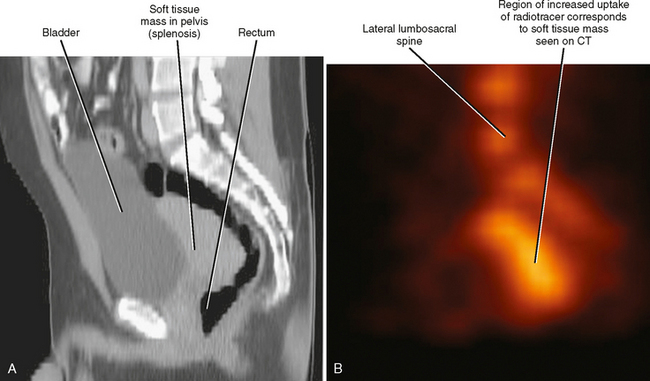
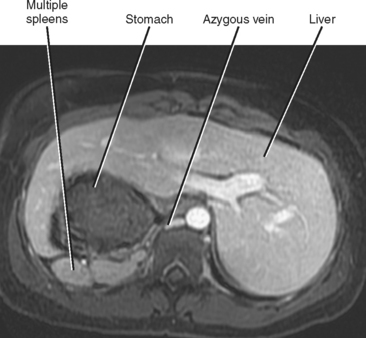
Splenosis is a condition that can result when splenic tissue gains entrance to the peritoneal cavity, usually caused by trauma, splenic rupture, or splenectomy (Fig. 15-7). Once within the peritoneal cavity, splenosis can migrate to any peritoneal recess similar to the peritoneal spread of tumor or infection. Splenosis does not receive blood supply from the splenic artery, resulting in different enhancement characteristics and poor function compared with the normal spleen and splenules. Splenosis may be confused with pathologic processes such as peritoneal metastatic disease or lymphadenopathy. Polysplenia, a congenital condition associated with a variety of other congenital abnormalities, can be distinguished from multiple accessory spleens by the absence of a normal dominant spleen in the former condition (Fig. 15-8).
NORMAL IMAGING APPEARANCE OF THE SPLEEN
During the arterial phase of dynamic multiphase, enhanced imaging with CT or MRI, the normal spleen enhances with a characteristic heterogeneous pattern that sometimes resembles the stripes of a zebra or tiger (Fig. 15-9). This heterogeneous enhancement pattern presumably results from differences in the rate of contrast (blood) flow through the different splenic compartments, with a portion of the blood percolating slowly through the splenic cords (open circulation of the spleen), and a percentage of splenic blood flow passing more rapidly through the splenic sinuses and into the venous sinuses that join to form the trabecular veins (closed circulation). Normal splenic enhancement usually becomes homogeneous after the first minute. The spleen avidly accumulates technetium sulfur colloid and heat-damaged red blood cells. Splenic uptake of superparamagnetic iron oxide particles results in significant signal loss on T2- and T2*-weighted MRI sequences.
Accessory spleens have the same imaging characteristics on ultrasound (US), CT, and MRI as the normal spleen (see Fig. 15-2). Enhancement of accessory spleens after intravenous contrast administration on CT and MR images may be similar in character and intensity to that of the normal spleen, a feature that helps distinguish accessory spleens from pancreatic, adrenal, or peritoneal neoplasms. However, when accessory spleens enhance to a lesser degree than the spleen, they may be more difficult to distinguish from other types of masses. They can be correctly identified with the same nuclear medicine techniques used to image normal spleen or with ferumoxides-enhanced MRI.
DIFFUSE SPLENIC ABNORMALITIES
Splenomegaly
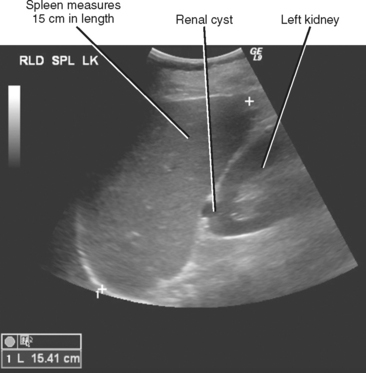
The most frequently encountered abnormality of the spleen is splenomegaly. Normal splenic size and shape varies considerably between individuals, making a simple and accurate imaging definition of splenomegaly difficult to establish. A variety of measurement techniques have been proposed to define splenomegaly on imaging studies, although most radiologists rely on the readily determined splenic length for this purpose. Although a length of more than 13 cm is often regarded as evidence of splenomegaly in clinical practice, the range of lengths considered abnormal in the literature extends from 10 to 15 cm (Fig. 15-10). More complex multidimensional indices or volumes are rarely calculated in routine practice, and a subjective assessment of splenomegaly is often made. A rounded appearance or extension of the spleen below the right hepatic lobe or lower third of the left kidney is used by some as a rapidly obtained estimate of splenomegaly.