Fig. 6.1
Normal anatomy of the sacroiliac joint, (a) anterior and (b) posterior ligaments of the sacrum and sacroiliac joint, (c) axial through right sacroiliac joint demonstrating normal interdigitations of the articulations
Traditionally, the SIJs were considered to consist of a smaller posterosuperior ligamentous compartment and a larger anteroinferior synovial compartment. More recent research has stimulated a debate on whether the articulation is best classified as a symphysis rather than a synovial joint. The articular margins of the sacrum and iliac bones are irregular with interdigitations, which limit mobility and enhance the strength of these joints. The articular surface of the sacrum is C or L shaped, opening dorsally. There are irregular bony pits, dorsal to the articular surface, at the site of ligamentous attachment, the dorsal syndesmosis. The articular surface at the centre of the SIJs has hyaline cartilage with fibrocartilage only at the periphery. The periphery of the cartilage, with the exception of the distal third of the iliac cartilage, blends with the stabilising ligaments as in a symphysis and forms a wide margin of fibrocartilage. A small synovial recess exists at the ventral aspect of the distal third of the iliac aspect of the joint. The SIJs are probably therefore best described as a symphysis with characteristics of a synovial joint being restricted to the ventral aspect of the distal cartilaginous portion at the iliac side.
Under the age of 30 years, the SIJs are usually symmetric in appearance. A higher prevalence of asymmetric non-uniform joint space narrowing and ill-defined subchondral sclerosis has been observed in women, obese and multiparous females than in age-matched males, and individuals of normal weight and non-multiparous, respectively. The width of the normal SIJ varies from 2 to 5 mm. The normal SIJ can demonstrate considerable variability, particularly with increasing age. Prominent sacral irregularities and marrow defects at the attachment of the interosseous ligaments, termed insertion pits, may be seen in normal subjects. Multiple anatomical variants have been observed in patients undergoing pelvic CT for indications other than disease of the SIJs. These include accessory joints (19 %), ‘iliosacral complex’ (6 %), bipartite iliac bony plate (4 %), crescent-like iliac bony plate (4 %), semicircular defects at the sacral or iliac side (3 %) and ossification centres (1 %).
There are a number of different imaging techniques used in the diagnosis of SII. They include plain radiographs, conventional tomography, scintigraphy, ultrasound, computed tomography and magnetic resonance imaging. Imaging allows for objective evidence of SII.
Plain Radiography
Plain radiography has and continues to play an important role in the investigation of SII and is an integral part in the diagnosis of AS. The anatomy of the sacroiliac joint, due to its oblique nature and overlap of the sacral and iliac components, has led to significant inter- and intraobserver variations particularly in the interpretation of early SII. Differentiation from normal patients is particularly problematic in women and in older age groups where early degenerative changes may simulate early SII. Plain radiographs of the sacroiliac joint can be performed and include dedicated AP and bilateral oblique views (Fig. 6.2). However, an AP radiograph of the lumbar spine often clearly demonstrates the sacroiliac joints and if fully included has been shown to be as sensitive as dedicated AP of the SIJ (Figs. 6.3 and 6.4). Because of the oblique orientation of the SIJs on the frontal radiograph, there is considerable overlap of the joints on plain radiography, and oblique views may be required for further detailed evaluation in selected cases. Some centres advocate a baseline AP pelvis. This allows for assessment of the sacroiliac joints and the hip joints; the latter is involved in up to 25 % of patients with SpA. Plain radiography should be performed as the initial imaging modality.
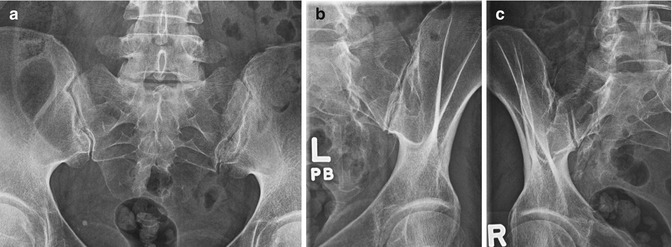

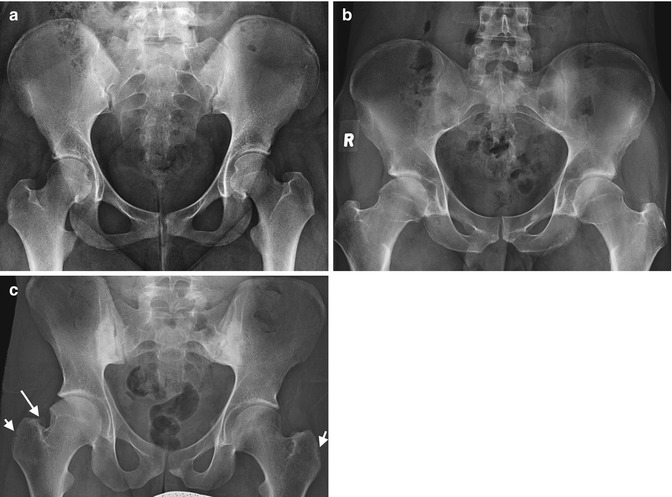
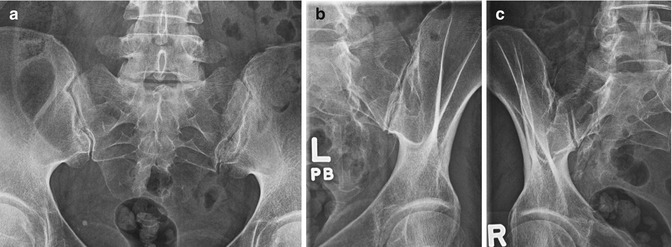
Fig. 6.2
Normal radiographs of the sacroiliac joints, (a) AP, (b) left oblique and (c) right oblique

Fig. 6.3
AP radiograph of the lumbar spine which includes normal sacroiliac joints
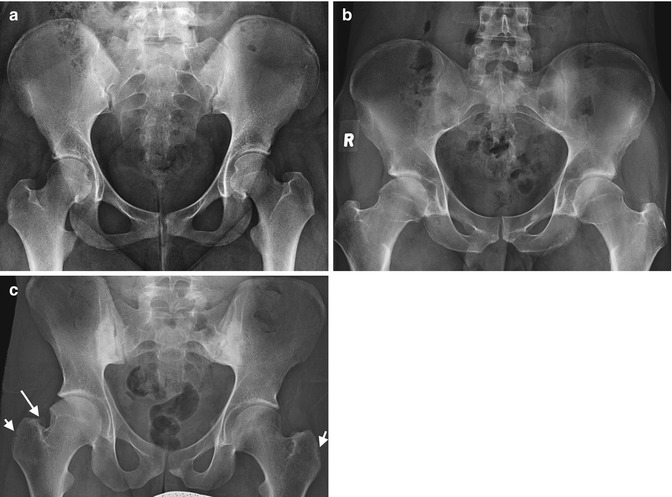
Fig. 6.4
(a) AP pelvis with normal SIJs and allows for assessment of hip joints and symphysis pubis, (b) a 34-year-old male with AS with symmetrical SIJ space loss, erosions and subchondral sclerosis and bilateral hip involvement, (c) a 35-year-old male with AS and similar changes as in fig (b) but with additional cortical changes, early erosions (small arrows) of the greater trochanter and enthesophyte formation (large arrow)
Radiographic changes include periarticular osteopenia, erosions and initial joint space widening progressing to narrowing joint space in later disease, subchondral sclerosis and finally bony ankylosis. The modified New York criteria include radiographs as a key component in the diagnosis of AS (Table 6.1). Grade 2–4 bilateral disease or unilateral grade 3–4 disease with one clinical criterion was required for the diagnosis (Fig. 6.5). Involvement of the spine was not included in this criteria set.
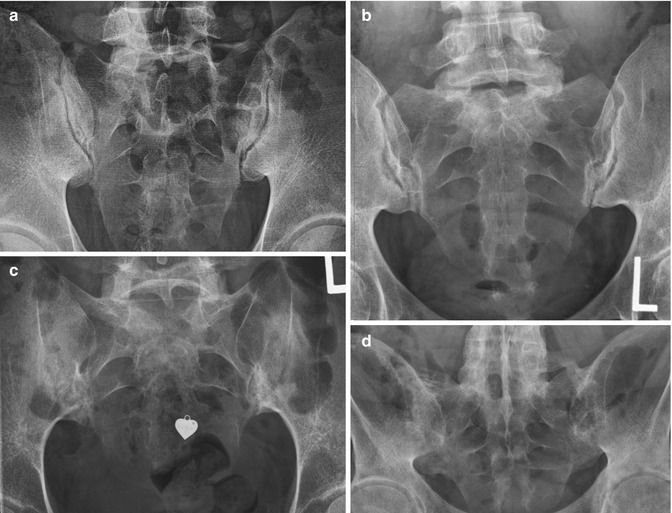
Table 6.1
Modified New York grading criteria
New York modified grading criteria | |
|---|---|
Grade 0 | Normal |
Grade 1 | Suspicious change |
Grade 2 | Minimal abnormality – small localised areas with erosion or sclerosis without alteration in joint width |
Grade 3 | Definite abnormality – moderate or advanced disease including partial ankylosis |
Grade 4 | Severe abnormality – total ankylosis |
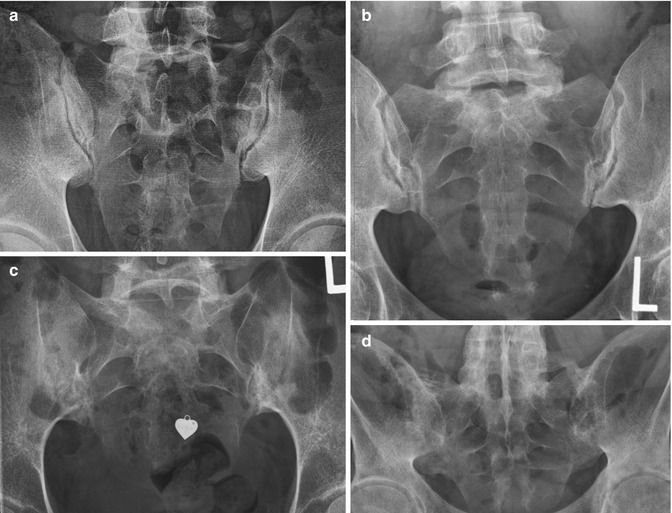
Fig. 6.5
New York modified grading criteria for radiographic sacroiliitis, grade 0 (Fig. 6.2), (a) grade 1 with suspicious changes, possible early erosions of the inferior sacroiliac joints bilaterally, (b) grade 2 in a 36-year-old female with bilateral erosions and maintained joint space, (c) grade 3 in an 18-year-old female with bilateral erosions, joint space loss and partial ankylosis, (d) bilateral SIJ ankylosis
Conventional Tomography and Tomosynthesis
Conventional tomography is associated with a higher radiation burden than plain radiographs and is no longer used. The newer technique of tomosynthesis holds promise, but our initial evaluation demonstrated a higher radiation burden than low-dose CT and is not indicated until further research is performed to evaluate its position in the investigation of sacroiliitis.
Ultrasound
Ultrasound is not currently utilised in clinical practice in the assessment of SII. Ultrasound can evaluate the posterior portions of the sacroiliac joints with Doppler and has shown in some studies increased vascularisation with decreased resistive indices in this portion of sacroiliac joint in patients with active SII. Further research is warranted to assess what role ultrasound will play in SII.
Nuclear Medicine
Scintigraphy had previously been a commonly used modality in the investigation of SII in clinical practice. It is very sensitive in the detection of early articular inflammatory change but is non-specific (Fig. 6.6). Radionuclide normally accumulates at the SIJs, and the differentiation of normal uptake and early SII can be difficult. Quantitative analysis of the SIJs has proven more sensitive in this regard. There are limitations however due to the wide range of variation in quantitative evaluation in the normal population. Other factors including age and prominent first sacral spine may all cause difficulties. Scintigraphy has poor sensitivity when compared with MRI in symptomatic spondyloarthropathy patients. Due to the above limitations and given the significant associated radiation dose, scintigraphy is not part of our diagnostic imaging algorithm.
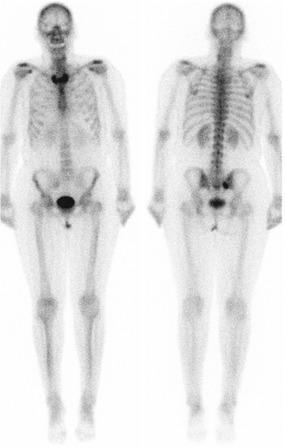
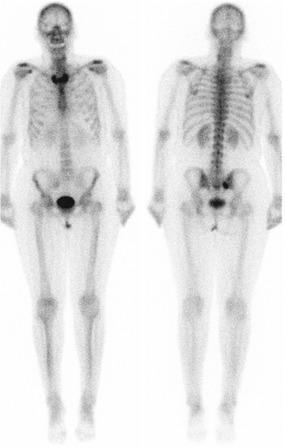
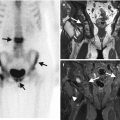
Fig. 6.6
Bone scan in a patient known with asymmetrical sacroiliitis; note increased uptake of the right inferior sacroiliac joint on posterior view. Increased uptake at sternoclavicular joints was related to incidental degenerative disease
CT
CT is excellent in demonstrating the anatomy of the SIJs and allows high-resolution axial acquisition with coronal and sagittal reconstruction (Fig. 6.7). Modern comparative studies between plain radiographs and CT have demonstrated marked advantage of CT in the delineation of chronic changes including erosions, subchondral sclerosis, ankylosis and fat replacement of bone marrow (Fig. 6.8). CT has the advantage that it can also demonstrate new bone formation at entheses. CT does not offer evaluation of acute inflammatory changes, which can be delineated on MRI. In addition CT involves the use of ionising radiation. CT can be useful in delineating alternate pathology, reviewed later in this chapter.
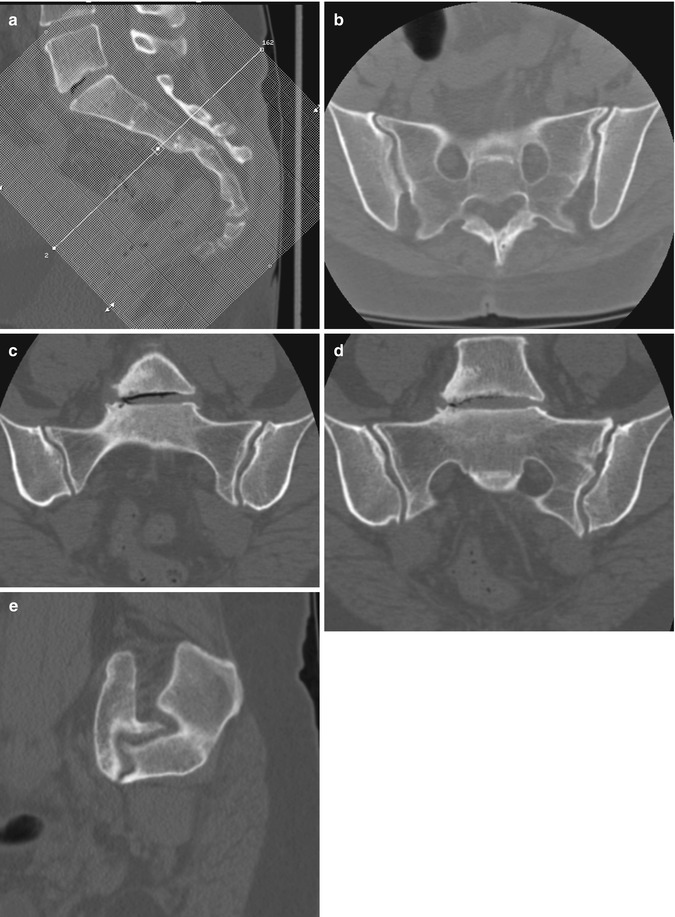
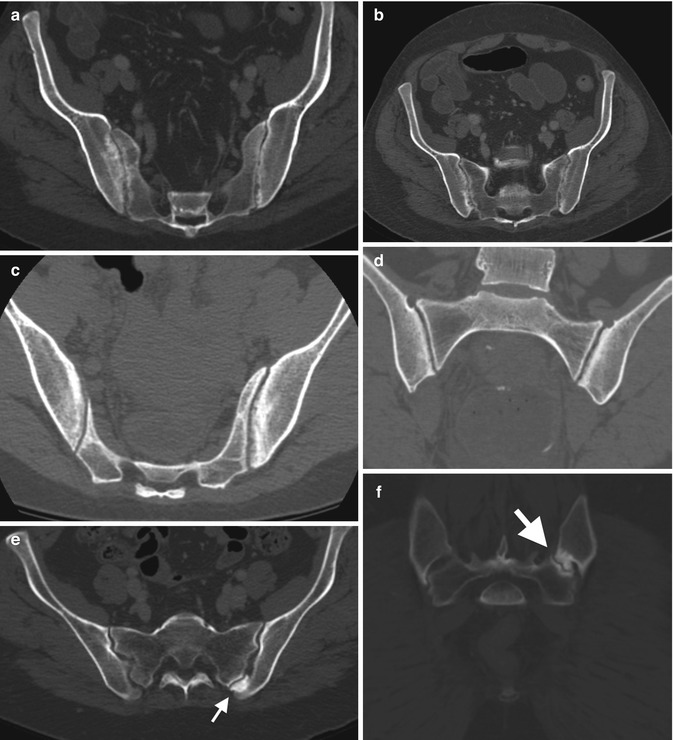
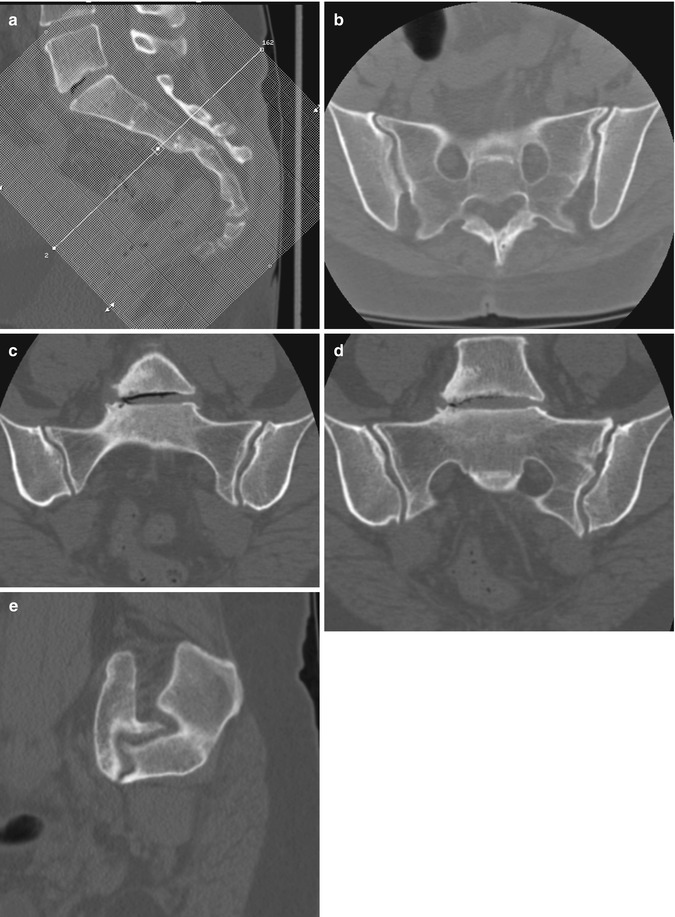
Fig. 6.7
CT of the sacrum and sacroiliac joints, (a) localiser image of the sacrum, the scan planes are acquired from this image, the axial line transversing the image is in the true axial plane sacrum. Figs. (b–d) are true coronal through the sacroiliac joints and (e) is a sagittal reconstruction (usually not required for sacroiliac disease but may be beneficial for other pathology including fracture assessment)
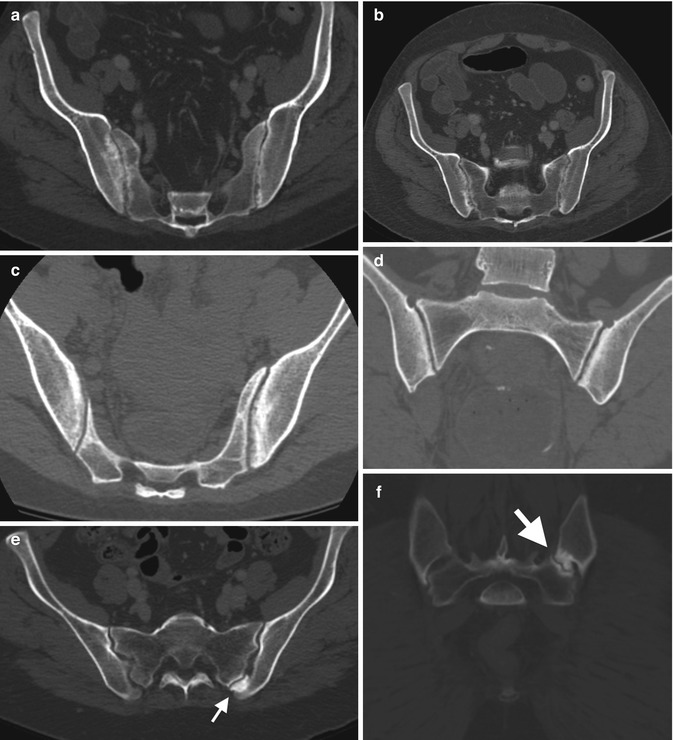
Fig. 6.8
(a) A 31-year-old male with ulcerative colitis (UC). CT of the pelvis, bone windows, demonstrates bilateral sacroiliac joint space loss, erosions and mild subchondral sclerosis. CT performed for assessment obstruction (b) demonstrates dilated small bowel loops secondary to distal obstruction. (c) A different patient, also with UC, demonstrates similar bilateral disease with coronal reformats (d). Incidental left accessory facet joint (arrow) in another patient on axial (e, f) coronal reformat CT
Magnetic Resonance Imaging (MRI)
MRI is the imaging gold standard for sacroiliitis. MRI is nonionising and provides excellent anatomical detail and delineation of both acute and chronic changes of sacroiliitis. We will briefly review the anatomy of the sacroiliac joints on MRI prior to reviewing pathological changes. On MRI, cartilage is well visualised as a zone of intermediate signal intensity on both T1 and T2 weighting bounded on either side by low signal intensity intact cortex of the underlying sacrum or ilium (Fig. 6.9). The combined cartilage has a maximum thickness of 4–5 mm and is slightly thinner anteriorly and inferiorly. It is not possible to differentiate hyaline and fibrous cartilage by signal intensity. On T1FS the cartilage is of intermediate to high signal intensity, and the altered greyscale of the T1FS sequence improves visualisation of the cartilage and adjacent cortical bone. Standard T1 sequences are, however, invaluable in assessing the subchondral bone marrow and, in particular, in differentiating between subchondral sclerosis and fat that may both appear as low signal on T1FS. In general, the subchondral bone marrow has homogeneous intermediate signal intensity on T1. In adults, the subchondral bone may be of heterogeneous signal due to the non-uniform haemopoietic marrow. Assessing the marrow signal intensity at the level of the sacral foramina can serve as baseline for the normal appearance of marrow in individual patients.
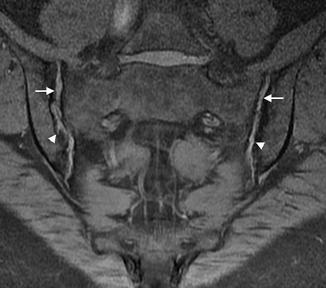
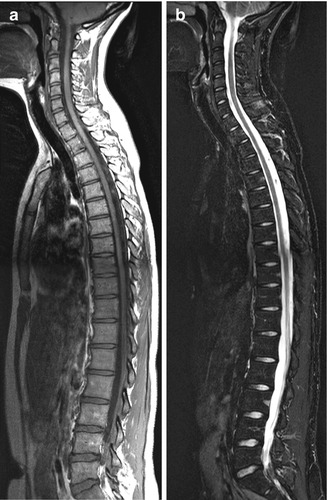
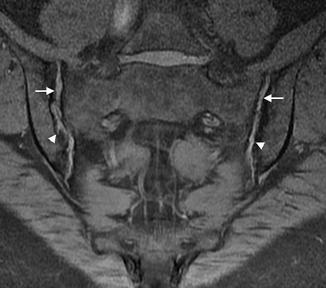
Fig. 6.9
Cor T1FS demonstrates intermediate SI articular cartilage (arrows) and early erosive disease (arrowheads)
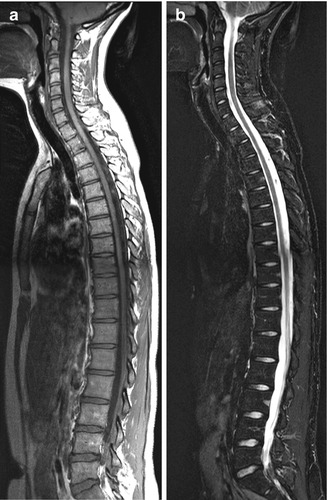
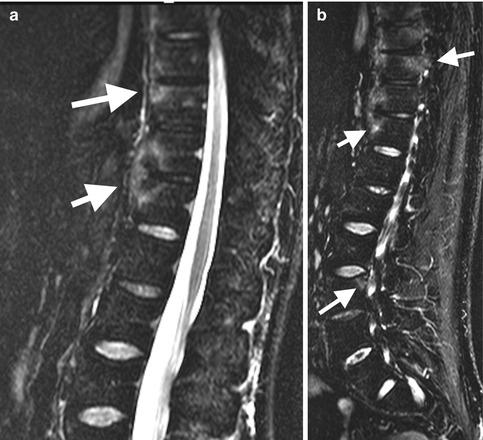
Fig. 6.10
Normal MRI, spondylitis protocol with normal bone marrow signal intensity, (a) Sag T1 and (b) Sag STIR of the whole spine
The referring clinician needs to be aware of certain contraindications to MRI. These include cardiac pacemakers, cochlear implants and ferromagnetic intracranial or intraorbital surgical clips or foreign bodies. Certain types of hardware elsewhere also are contraindicated. It is best to discuss possible contraindications with your MRI centre. With the advent of short bore MR scanners, claustrophobia is less of a problem but appropriate sedation is still required in some patients.
In the first description of MRI in sacroiliitis, Ahlstrom et al. found striking changes in the subchondral bone marrow. They emphasised the unique ability of MRI to demonstrate abnormalities in subchondral bone and periarticular bone marrow. They concluded that the early inflammatory changes in sacroiliitis are likely to occur in the subchondral structures of the SIJ. This study opened the door for the potential use of MRI in the investigation of SII, and thereafter a multitude of studies confirmed their initial finding and supported the development of MRI in the diagnosis and management of patients with SII. Research on the use of MRI in SII has proliferated with the advent of anti-TNF treatment. Early research concentrated on the quantification of active disease involving the sacroiliac joints with the use of contrast enhancement and dynamic contrast enhancement. STIR imaging was found to be almost as sensitive as the enhanced examination and was less expensive and time consuming and has become a major imaging sequence for the assessment of active disease. Enhanced studies are now rarely acquired in our clinical practice except in those cases where alternate pathology such as infection or tumour is suspected.
Imaging
Spinal
Spinal changes of SpA usually commence and are most pronounced within the thoracic spine. Spinal disease usually occurs with or after the onset of sacroiliitis, but in a minority of patients, spinal changes are the initial imaging finding on MRI. Spinal changes include spondylitis, Romanus lesions, syndesmophytes, spondylodiscitis, enthesitis and facet and costovertebral arthritis (Figs. 6.10 and 6.11) (Table 6.2).
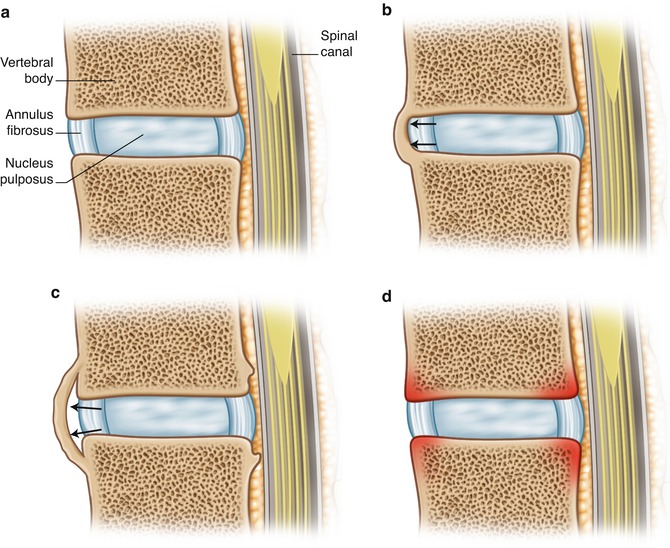
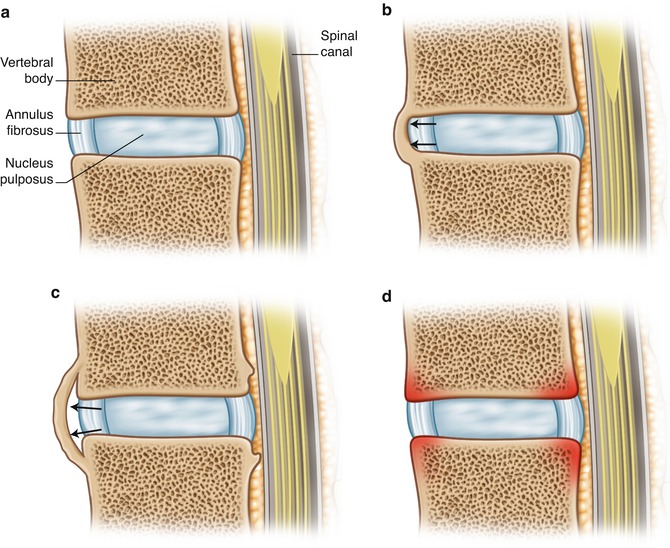
Fig. 6.11
Spinal changes SpA, (a) normal, (b) syndesmophyte formation in ankylosing spondylitis and (c) in psoriasis and Reiter’s (d) vertebral osteitis (outlined in red)
Table 6.2
Spinal changes in spondylitis
Spinal pathology | Radiograph | MRI |
|---|---|---|
Romanus lesion | Anterior vertebral body corner erosion. May heal with sclerosis, the shiny corner | Focal osteitis, high SI on STIR, low T1, anterior corners of the vertebral body. Chronic lesions are depicted as foci of fat signal intensity, high on T1 and T2 |
Andersson lesion/spondylodiscitis | Types 1, 2 and 3. Localised or generalised discovertebral destruction with surrounding ill-defined sclerosis. Fractured posterior elements in type 3 | Irregularity to frank erosion of cortical endplate, adjacent osteitis of increased SI on STIR vertebral body, low SI disc and sclerosis deep to osteitis. Assess for posterior element fracture |
Spondylitis | Anterior (Romanus) or posterior vertebral body corner erosion. May heal with sclerosis, the shiny corner | Corner or non-corner osteitis vertebral body, high SI STIR, low on T1. Chronic lesions are depicted as foci of fat signal intensity, high on T1 and T2 |
Facet joint arthritis | Erosions, subchondral sclerosis and eventually joint ankylosis | Erosions, osteitis pedicles, subchondral sclerosis and eventually joint ankylosis |
Costovertebral arthritis | Erosions, sclerosis and fusion. Difficult to detect on radiographs | Erosions, subchondral osteitis, subchondral sclerosis and eventually joint ankylosis, involves costotransverse and costovertebral joints |
Enthesitis | May be normal or erosion and osteopenia, reactive sclerosis | High SI within ligament and osteitis at bony attachment, may develop erosion and sclerosis, commonly seen in posterior element involvement |
Syndesmophytes | New bone formation within the outer fibres of the annulus fibrosis of the intervertebral disc commencing at the juncture with the vertebral body, eventually bridging between vertebral bodies | May be difficult to identify on MRI, radiographs are more sensitive. Non-bridging bone following marrow SI on all imaging sequences |
Ankylosis | Bony fusion, partial or complete, across a joint space | Bony fusion, partial or complete, across a joint space. May have bone marrow SI (easier to identify on MRI) or be sclerotic and low SI on all sequences |
A Romanus lesion, initially described on radiographs as an early spinal change in AS, is an erosion of a vertebral corner at the discovertebral junction (Fig. 6.12). Erosions heal with the development of corner sclerosis, ‘shiny corners’, occurring at the anterior superior or inferior corners of the vertebral body. This is secondary to new bone formation at the site of prior inflammation and may represent an altered healing response that occurs in AS. With MRI, inflammatory changes can be identified prior to any radiographic change. MRI can demonstrate focal osteitis, high SI on STIR, low on T1, at the anterior corners of the vertebral body in the acute stage (Fig. 6.13). This is also termed a corner inflammatory lesion. These may occur anteriorly or posteriorly. Non-corner inflammatory lesions are identified as osteitis parallel to the endplate centrally. When osteitis involves the more lateral margins of the vertebral body, at the level pedicles and beyond, it is termed a lateral inflammatory lesion. Osteitis at the costovertebral and costotransverse articulations may occur and is thought to be a more sensitive indication of SpA (Figs. 6.14). Inflammation may also involve the posterior elements of the vertebra including the facet joints (including capsule, facets and perifacet soft tissues), posterior ligaments and related enthesis (Fig. 6.15). When the acute osteitis resolves, the normal haemopoietic tissue within the marrow is no longer present, and the marrow is predominantly of fat signal intensity. These post-inflammatory fat accentuation (PIFA) foci appear as high SI on both T1 and T2 sequences (Fig. 6.16). Spondylitis is inflammation of the vertebral body. It encompasses corner osteitis both anterior, the Romanus lesion, and posterior, non-corner osteitis and posterior element involvement. Squaring of the vertebra is loss of the normal anterior concavity due to vertebral corner erosion (Fig. 6.17).
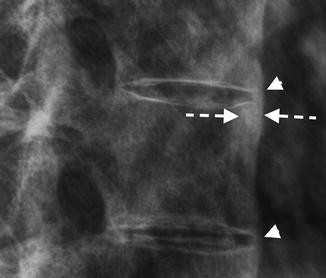
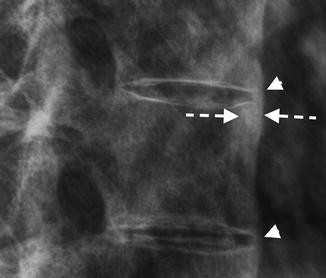
Fig. 6.12
Magnified lateral lower thoracic spine radiograph with anterosuperior corner vertebral sclerosis (dashed arrow) in keeping with a healed Romanus lesion. Note syndesmophytes (arrowheads) and early squaring of the anterior vertebral body