Fig. 1 a–d.
Subacromial bursitis. Coronal oblique (a) and axial (b) sonograms show the subacromial synovial bursa presenting a thick hypervascularized wall and some fluid content (asterisk). c MSUS-guided intrabursal injection. Note the needle (black arrowheads) correctly positioned under the real-time guidance of ultrasound. The tip of the needle (small black arrowhead) lies inside the bursa. d After injection of a small amount of steroid-lidocaine, note the drug (white arrowheads) filling the bursa. No injection into the surrounding tissues is noted. Hum humerus, GT greater tuberosity of the humeral head (for color reproduction see p 302)
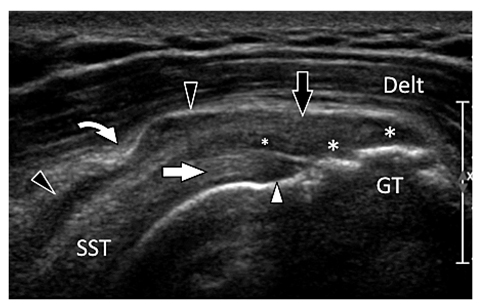
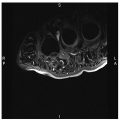
Fig. 2
Supraspinatus tendon partial tear. Coronal oblique sonogram obtained over the axis of the supraspinatus tendon (SST) at the anterior third. Sonogram shows an avulsion (asterisks) of the bursal two-thirds (black arrow) of the supraspinatus tendon associated with a horizontal tear (small asterisk). The deep third of the tendon (white arrow) is continuous. Note the hypoechoic appearance of its preinsertional part (white arrowhead) due to anisotropy. The subacromial synovial bursa (black arrowheads) presents an internal fluid effusion. Note the coracoacromial ligament (curved arrow). Delt deltoid muscle, GT greater tuberosity of the humeral head
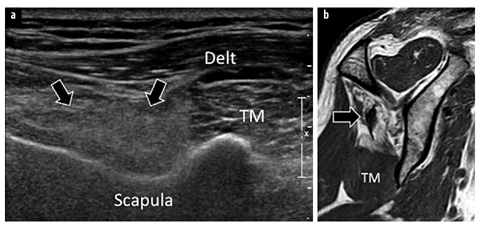
Fig. 3 a, b.
Infraspinatus muscle fat degeneration due to chronic tendon tear. a Sagittal oblique sonogram obtained over the posterior aspect of the scapula. b Corresponding sagittal oblique T1-weighted magnetic resonance image. The hypotrophic infraspinatus muscle (arrows) shows a hyperechogenic appearance due to fat infiltration. Note the slightly hypertrophic teres minor muscle (TM) presenting a normal echogenicity. Delt deltoid muscle
MSUS plays only a minor role in the assessment of glenohumeral instability, because it cannot assess accurately the glenoid labrum because of its deep location. MSUS can detect a Hill-Sachs fracture and evaluate its size. In posterior shoulder dislocation, which can go undiagnosed at radiography in nearly 50% of cases, MSUS can detect the posterior displacement of the humeral head in relation to the glenoid in axial sonograms, obtained over either the anterior or the posterior aspect of the joint. MSUS-guided injection of the acromioclavicular joint can be performed if pain persists after joint instability.
Spinoglenoid and supraglenoid notch ganglia, caused by degeneration or trauma of the glenoid labrum, can be associated with sports that use a repetitive overhead action. As a result of their location, they can compress the suprascapular nerve and lead to ill-defined shoulder pain and muscle fat degeneration and atrophy. They appear on MSUS as well-marginated hypoanechoic masses with no internal flow signals at color Doppler. The relation with the nerve can seldom be demonstrated because of the small size of the nerve. Sometimes, a labrum tear can be visualized at MSUS. Muscle edema, the first manifestation of nerve denervation, cannot be assessed by MSUS. Hypotrophy is detected as a decrease of the size of the muscle and is usually more visible in axial sonograms. Fat infiltration starts at the myotendinous junction and presents as an increased echogenicity of the muscle.
MSUS can accurately assess the extra-articular portion of the long head of the biceps tendon (LHBT). Most tears of LHBT are easily diagnosed clinically in the presence of a local post-traumatic pain and lump in the anterior aspect of the lower arm corresponding to the displaced muscle belly. MSUS is only indicated when the clinical findings are not diagnostic, such as in obese patients in whom the palpation of the retracted muscle can be difficult. MSUS shows absence of the tendon inside the humeral sulcus with concomitant inferior muscle retraction. The injured tendon and muscle can be surrounded by a hematoma in acute cases. MSUS can accurately show fat infiltrations of the muscle by comparing it with the normal short head of the biceps in axial images. LHBT instability is associated with rotator cuff interval or subscapularis tears. Its recognition can be difficult clinically. MSUS easily demonstrates the medial displacement of the tendon in axial images. In subluxation, the tendon is located over the anterior aspect of the lesser tuberosity, while in tendon dislocation it lies completely outside the sulcus. A careful scanning technique is necessary to detect the intra-articular displacement of the LHBT (Fig. 4).
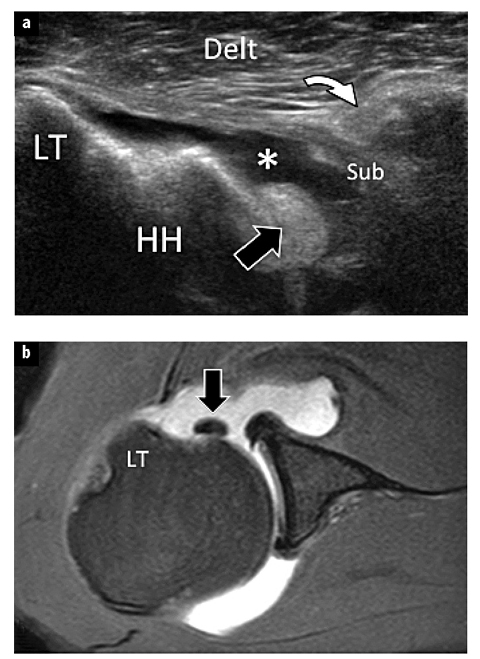
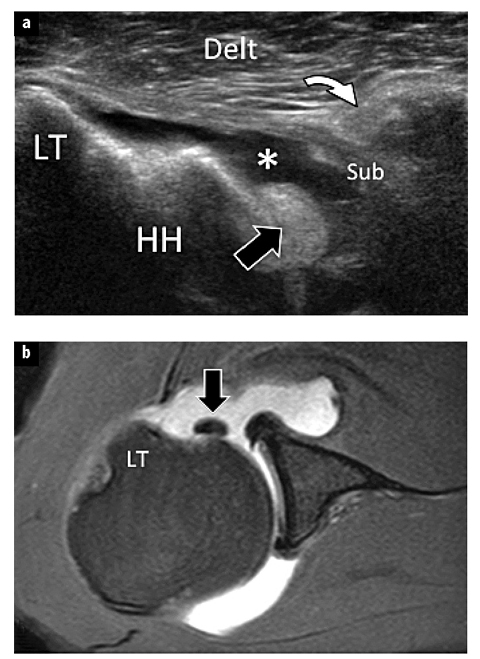
Fig. 4 a,b
Dislocation of the long head of the biceps tendon. a Axial sonogram obtained over the anterior aspect of the humeral head (HH). b Corresponding axial T1-weighted fat-saturated image after intra-articular injection of gadolinium contrast. The sonogram shows a full-thickness avulsion of the subscapularis tendon (Sub) that is retracted at the level of the short head of the biceps muscle (curved arrow). A reactive joint fluid effusion (asterisk) is evident. The long head of the biceps tendon (black arrow) is dislocated inside the glenohumeral joint. LT lesser tuberosity, Delt deltoid muscle
MSUS allows accurate, safe and quick injections of subacromial bursa, glenohumeral and acromioclavicular joints [5, 6]. The main advantage of MSUS guidance during corticosteroid injection is the ability to identify vascular structures, nerves and tendons near to the needle path, in order to avoid them. Also, it confirms the appropriate location for the injection (Fig. 1). When the injection is carried out by an experienced sonologist, the procedure is virtually painless and performed within a few minutes. Percutaneous treatment of rotator cuff tendon calcifications can be efficiently guided by MSUS using a single- or double-needle technique, facilitating prompt shoulder function recovery and pain relief [7].
Elbow
Tendinopathy, and partial and complete tears of the triceps are not uncommon in athletes, particularly weightlifters. MSUS can diagnose tears and accurately differentiate partial tears from complete tears. Partial tears typically affect the superficial layer of the tendon, arising from the fusion of the long and lateral heads of the tendons, and they are frequently associated with bony avulsion [8 (Fig. 5).
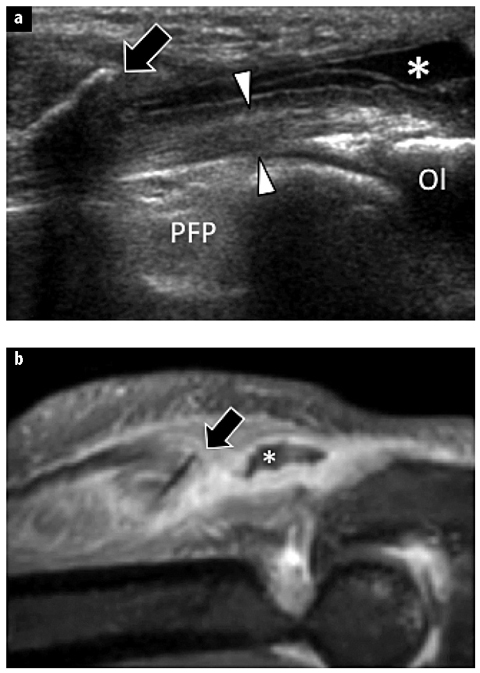
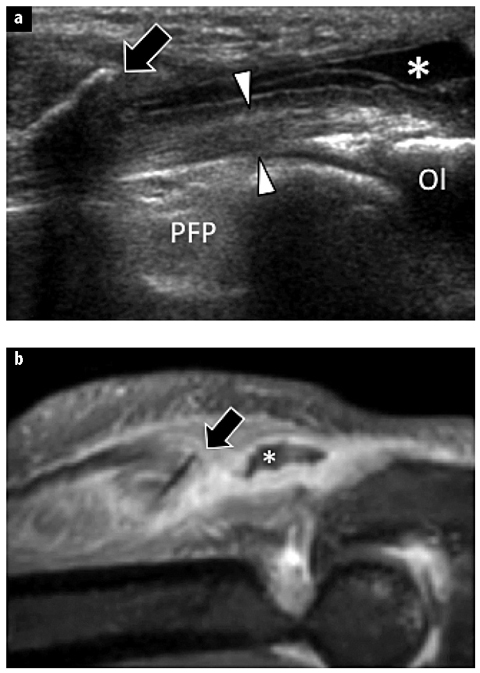
Fig. 5 a, b.
Partial tear of the triceps tendon at the elbow. a Sagittal sonogram obtained over the distal triceps tendon. b Corresponding sagittal T1-weighted fat-saturated image after intravenous injection of gadolinium contrast. The sonogram shows a partial-thickness avulsion of the triceps tendon with presence of an avulsed osseous fragment (arrow) retracted proximally. A reactive local fluid effusion (asterisk) is evident. The deep portion (arrowheads) of the tendon is continuous. Note absence of articular effusion. Ol olecranon, PFP posterior fat pad of the elbow joint
Distal biceps tendonitis is usually caused by chronic overuse. MSUS can show a hypoechoic swelling and irregular fibrillar pattern of the tendon. Differentiating a chronic tendinopathy from a partial tear is difficult because their sonographic appearances can be very similar. In these situations, correlation of the MSUS data with clinical findings is very helpful. Clinical signs and symptoms of complete tears are acute antecubital pain, elbow supination and flexion weakness, and proximal retraction of the muscle from its insertion at the radial tuberosity. A local ecchymosis is usually present. These tears typically result from a powerful eccentric contraction of the biceps. The amount of muscle retraction depends mainly on the integrity of the lacertus fibrosus, the integrity of which needs to be substantially altered to cause a significant retraction. On MSUS, complete tears appear as complete interruption of the tendon usually by an avulsion from the radial tuberosity. If the lacertus fibrosus remains continuous, there is usually a 1–2 cm tendon retraction. In a significant tear of the lacertus fibrosus, the tendon can retract as far as the distal 1/3 of the arm and is often surrounded by a hematoma. Bicipitoradial bursitis lesions are caused by overuse, and they present as hypoechoic fluid collections located between the distal biceps tendon and the radius. In severe cases, the tendon can be surrounded by fluid, mimicking tenosynovitis [9].
The common extensor tendinopathy at the lateral epicondyle (tennis elbow), and the common flexor tendino – pathy at the medial epicondyle (golfer’s elbow,) are frequent and related to local repeated mechanical trauma. In both cases, MSUS can show the thickened and irregularly hypoechoic tendon. Presence of intratendinous calcifications (hyperechoic spots), their size and exact location can also be accurately determined. Color Doppler can show the presence of neovascularization of the tendon (Fig. 6). Small tears are usually horizontal and located in the middle third of the tendon. Severe full-thickness tears affect mainly the anterior third of the tendon and are more common in patients treated previously by local steroid injections [10]. Dry needling and/or therapeutic local injections can, when needed, be effectively guided by MSUS.
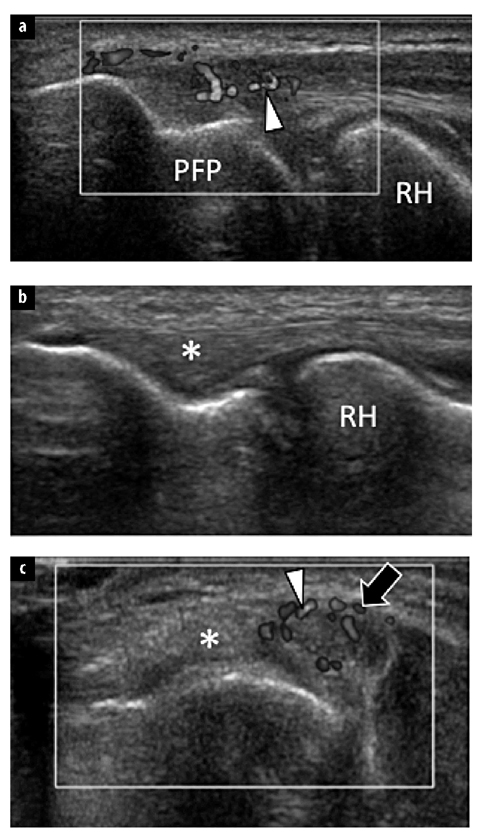
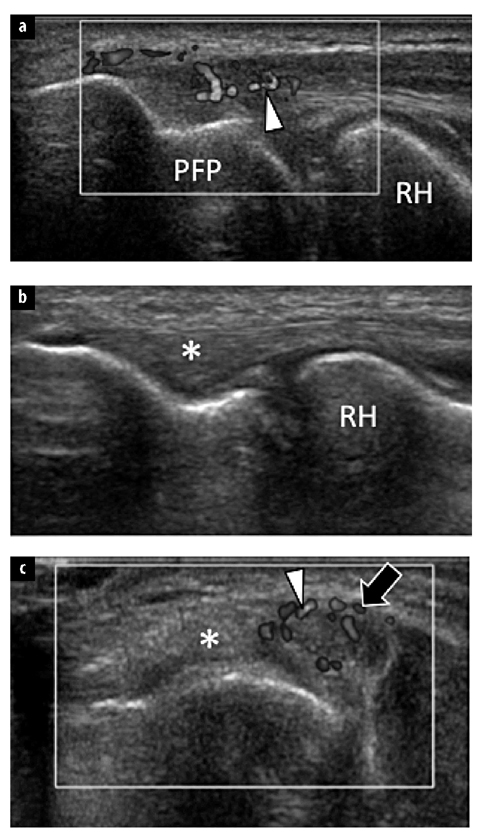
Fig. 6 a–c.
Tendinopathy of the common extensor tendon at the elbow. All sonograms were obtained over the common extensor tendon. a Coronal color Doppler sonogram obtained over the anterior part of extensor. b Coronal sonogram obtained over the posterior part of the tendon. c Axial color Doppler sonogram. Note swelling, irregular hypoechoic appearance and hypervascular changes (arrowheads) limited to the anterior part (arrow) of the common extensor tendon. The posterior part (asterisk) of the tendon is normal. RH radial head, PFP posterior fat pad of the elbow joint (for color reproduction see p 303)
Wrist and Hand
A wide variety of tendinopathies at the wrist and hand can affect the sportsman, and they are usually caused by repetitive microtrauma. On the posterolateral side of the wrist, the tendinopathy of the extensor carpi ulnaris (ECU) can cause chronic pain in sportsmen, particularly tennis players [11]. A predisposing factor of this pathology may be recurrent subluxation of the ECU tendon. Clinical findings are usually not specific and may mimic disorders of the distal radioulnar joint. MSUS can determine the presence of tendinopathy and/or tenosynovitis by showing the ECU tendon size, identifying the presence of irregular hypoechoic changes, detecting intrasubstance longitudinal splits commonly related to its instability, and by showing synovial hypertrophy, sheath effusion or local hypervascularization. Associated retinaculum tears are not infrequent and can cause instability of the tendon. Tears usually follow acute traumas, such as powerful pronation from a supinated position when playing tennis. This causes the ECU to dislocate anteriorly. Dynamic ultrasound scanning performed during pronationsupination movements is ideal to depict this condition.
Detection of some wrist fractures can be difficult by plain radiographs because of the superposition bony structures, and, because of its tomographic capabilities, MSUS can aid in their diagnosis. MSUS can help in identifying the scaphoid and hook of hamate fractures. It can also detect dorsal avulsion of the triquetrum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree