Recent technologic advances including multidetector CT, dynamic CT angiography, high-field MR imaging, four-dimensional MR angiography, and physiologic studies, such as perfusion imaging, have revolutionized the imaging work-up of head, neck, and skull base lesions. These techniques not only provide accurate diagnostic information, but also help plan endovascular therapy. The future holds great promise for interventional neuroradiologists because excellent imaging tools are becoming available that are capable of providing morphologic, hemodynamic, and physiologic information. Furthermore, availability of faster, real-time guidance systems and hybrid systems improves the ability to perform procedures not only in a rapid and safe manner but also with great precision.
Image-guided interventions have undergone a rapid evolution in the last two decades. As compared with open surgical procedures, image-guided techniques offer minimally invasive diagnostic and therapeutic alternatives for various vascular and nonvascular head and neck pathologies. Recent advances in noninvasive imaging not only provide faster and dynamic images but also greater anatomic coverage and improved resolution. Physiologic imaging techniques, such as tissue perfusion, spectroscopy, and thermal mapping, are finding increased use in the management of various head and neck disorders.
Head and neck interventions can be performed by percutaneous, endovascular, or a combination of these approaches. Percutaneous procedures include biopsies, aspirations, sclerotherapy, and newer radiofrequency and cryoablation techniques. Transarterial endovascular approach forms the mainstay of treatment for head and neck bleeding, as well as intra-arterial targeted chemotherapy of neoplasms. Combined percutaneous and endovascular approaches can be useful in the treatment of craniofacial vascular malformations and highly vascular tumors.
Cross-sectional imaging modalities including CT, CT angiography (CTA), MR imaging, MR angiography (MRA), and positron emission tomography (PET) have become an integral part of initial work-up of various head and neck disorders. CT and MR imaging can also provide image guidance during the percutaneous procedures. Latest multidetector CT (MDCT) scanners allow the imaging of larger volumes at much faster speed while maintaining excellent resolution and image quality. CT fluoroscopy and various hybrid imaging systems are tremendous assets in performing various head and neck procedures with greater safety and accuracy. Recently introduced dynamic CTA and four-dimensional MRA techniques can provide hemodynamic information of both the arterial and venous systems in the head and neck. These techniques are helpful in noninvasive evaluation of vascular abnormalities, such as arteriovenous malformations, arteriovenous fistulae, steno-occlusive lesions, and hypervascular masses.
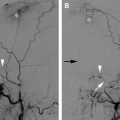
The role of perfusion imaging is expected to grow in the management of head and neck vascular pathologies ( Fig. 1 ). Perfusion imaging, whether performed with CT or MR imaging, evaluates dynamic microscopic blood flow changes through a region of interest. Changes in tissue signal intensity (MR imaging) or attenuation (CT) are measured during a dynamic contrast infusion. Recent literature suggests that perfusion techniques could play an important role in determining which patients with head and neck carcinomas would benefit from medical treatment as opposed to surgical treatment. New developments in thermal imaging are helping to optimize thermal ablations by providing better control at the tumor margins. Continuously evolving imaging techniques play an increasingly important role in the overall care of patients with various head and neck disorders and assist the interventional neuroradiologist in performing safer and effective interventions in the head and neck.
CT
The advent of CT in the late 1970s enabled direct visualization of the soft tissues and its pathology for the first time because of its high contrast resolution. With further development, spiral CT scanners offered faster imaging algorithms and the possibility to image entire anatomic regions relatively quickly. Introduction of slip-ring technology allows the scanner gantry to rotate continuously with concurrent patient table movement. At that speed, most patients are able to hold their breath for the entire imaging session. This improves image quality by eliminating artifacts related to patient motion and breathing. The continuous image acquisition without gaps between slices obtained through helical scanning provides volumetric data that can be reconstructed to produce three-dimensional images. Displaying the entire volume of organs and vessels increases the likelihood of detecting very small lesions.
MDCT systems have been a revolutionary advancement in CT technology. They provide greater anatomic coverage, higher spatial resolution, faster acquisition times, and improved image quality. These faster scanning techniques improve temporal resolution, resulting in dynamic images of the arterial and venous systems. The ability to obtain isotropic volumetric data with superior spatial resolution enables high-quality three-dimensional picture displays of the curved vascular structures. This is specifically advantageous in evaluation of head and neck vascular pathologies, such as atherosclerosis, dissections, traumatic injury, and pseudoaneurysms. Today’s state-of-the-art postprocessing software helps delineate pathology with multiplanar imaging, and gathers important information for planning challenging endovascular procedures.
MDCT technology has witnessed rapid development from 1 row of detectors to 4, 16, and 64 rows followed by dual-source CT scanning. The advent of dual-source CT scanners is a significant shift in the further evolution of CT machines. Designed with two X-ray tubes and two detector arrays, the dual-source scanner can capture data nearly twice as fast as previous scanners. The main difference is that the dual-source CT has two X-ray sources and two 64-slice detector arrays as compared with the previous generation of CT scanners, which had a single X-ray source and single 64-row detector.
Recently, a 320-slice CT scanner with five times greater detector coverage than 64-slice CT scanners has been introduced. Using this new scanner, 16-cm (or 6.3-in) Z-axis coverage is now possible in less than 1 second and just one rotation of its gantry. In comparison, a 64-slice CT scanner images only 1.3 inches at a time, leading to relatively longer scan times. One of the major benefits of this scanner is reduced radiation exposure and contrast dose to the patient. The 320-slice CT scanner is extremely fast, taking just one revolution (0.35 seconds) to scan the entire brain. It also has the capability to scan a region repetitively, providing extremely fast and precise information on the functionality of an organ. For example, comprehensive imaging of patients presenting with acute stroke symptoms can be accomplished within 60 seconds. At The Johns Hopkins Hospital, the stroke protocol on 320-slice scanner provides a noncontrast head CT, dynamic (four-dimensional) CT angiogram of the entire brain, and whole-brain perfusion CT using only 50 mL of contrast and the scanning can be accomplished in less than 1 minute. This information is key to rapid assessment and treatment of acute stroke and other neurovascular disorders.
CT angiography
CTA is a rapid, noninvasive imaging technique that can produce high-quality angiographic projections of the cervical and cerebral vasculature after intravenous injection of radiographic contrast media. Although it has been in use since the early 1980s, marked improvements in this technique and postprocessing algorithms have occurred with the advent of helical and multislice CT scanners.
Using commercially available software, one can generate two-dimensional and three-dimensional images of vessels from the raw data. These reconstructed images can be viewed from any angle and with varied window settings. Shaded surface displays and maximum intensity projection are the most popular algorithms. It is also possible to view the inner surface of the vessel wall and navigate along the vessel lumen (intra-arterial endoscopy).
In addition to becoming a first-line imaging tool for the assessment of cervicocranial atherosclerotic disease, the role of CTA is also expanding in the assessment of anatomic variations, vascular injuries, dissections, and head and neck masses. CTA not only provides useful information on the vascular anatomy and pathology in the neck, but also helps evaluate the patency of circle of Willis. The information gained from CTA allows the head and neck interventionalist to perform more focused angiographic evaluation, thereby limiting the contrast and radiation dose from complex endovascular procedures. Additionally, CTA of head and neck can be easily combined with CT perfusion of the brain. This combined CTA–CT perfusion survey study provides comprehensive imaging assessment of the vascular pathology and its effect on the brain perfusion (see Fig. 1 ).
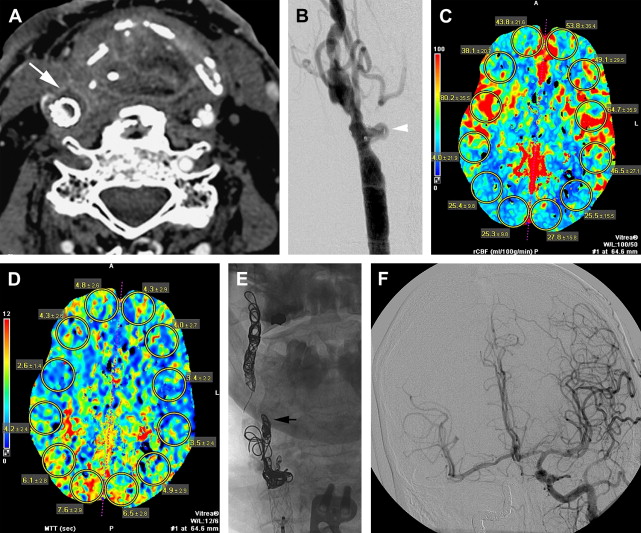
CTA is extremely useful in the evaluation of patients with head and neck cancer presenting with acute hemorrhage. Although digital subtraction angiography (DSA) is often performed in these patients and still considered gold standard, its interpretation can be confusing. In such patients, often with advanced head and neck carcinomas, postsurgical or postradiation changes commonly result in luminal irregularities or deformities in multiple arterial vessels making it difficult to pinpoint the exact source of hemorrhage. CTA can offer information that is complementary to DSA. It may provide increased sensitivity in detecting slow-filling pseudoaneurysms because of prolonged injection of contrast versus the rapid and transient injection during DSA ( Fig. 2 ). CTA can assess the vessel wall directly and provides information regarding the proximity of arterial structures to tumors or the aerodigestive tract. The authors almost always obtain a CTA in patients with suspected carotid blowouts. The information obtained on CTA helps in localization of the bleeding vessel and endovascular treatment planning (see Fig. 2 ).
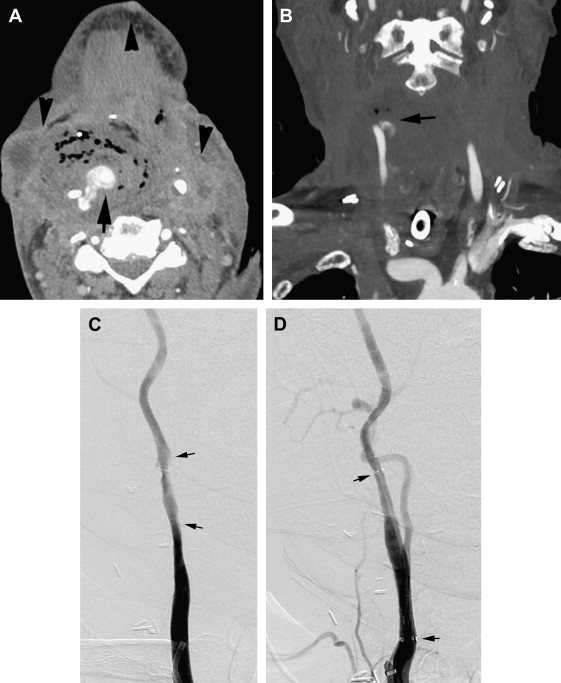
Several MDCT scanners now allow acquisition of dynamic scans with a wider scan range and faster acquisition times. Dynamic CTA techniques can provide both morphologic and blood flow hemodynamic information of various vascular lesions. In cases of complex arteriovenous malformations and fistulas, dynamic CTA allows identification of feeding arteries, nidus, and draining vessels and enhances the preoperative anatomic assessment of such vascular lesions ( Fig. 3 ).
CT angiography
CTA is a rapid, noninvasive imaging technique that can produce high-quality angiographic projections of the cervical and cerebral vasculature after intravenous injection of radiographic contrast media. Although it has been in use since the early 1980s, marked improvements in this technique and postprocessing algorithms have occurred with the advent of helical and multislice CT scanners.
Using commercially available software, one can generate two-dimensional and three-dimensional images of vessels from the raw data. These reconstructed images can be viewed from any angle and with varied window settings. Shaded surface displays and maximum intensity projection are the most popular algorithms. It is also possible to view the inner surface of the vessel wall and navigate along the vessel lumen (intra-arterial endoscopy).
In addition to becoming a first-line imaging tool for the assessment of cervicocranial atherosclerotic disease, the role of CTA is also expanding in the assessment of anatomic variations, vascular injuries, dissections, and head and neck masses. CTA not only provides useful information on the vascular anatomy and pathology in the neck, but also helps evaluate the patency of circle of Willis. The information gained from CTA allows the head and neck interventionalist to perform more focused angiographic evaluation, thereby limiting the contrast and radiation dose from complex endovascular procedures. Additionally, CTA of head and neck can be easily combined with CT perfusion of the brain. This combined CTA–CT perfusion survey study provides comprehensive imaging assessment of the vascular pathology and its effect on the brain perfusion (see Fig. 1 ).
CTA is extremely useful in the evaluation of patients with head and neck cancer presenting with acute hemorrhage. Although digital subtraction angiography (DSA) is often performed in these patients and still considered gold standard, its interpretation can be confusing. In such patients, often with advanced head and neck carcinomas, postsurgical or postradiation changes commonly result in luminal irregularities or deformities in multiple arterial vessels making it difficult to pinpoint the exact source of hemorrhage. CTA can offer information that is complementary to DSA. It may provide increased sensitivity in detecting slow-filling pseudoaneurysms because of prolonged injection of contrast versus the rapid and transient injection during DSA ( Fig. 2 ). CTA can assess the vessel wall directly and provides information regarding the proximity of arterial structures to tumors or the aerodigestive tract. The authors almost always obtain a CTA in patients with suspected carotid blowouts. The information obtained on CTA helps in localization of the bleeding vessel and endovascular treatment planning (see Fig. 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree