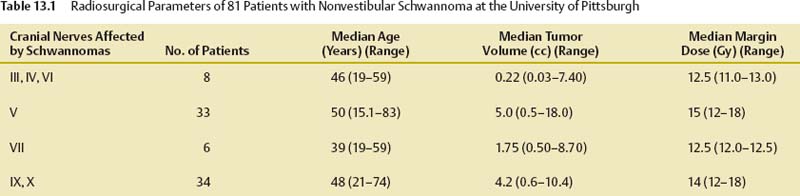
13 Nonvestibular schwannomas are rare tumors of the brain, comprising < 0.5% of all intracranial tumors. Like vestibular schwannomas, most are histologically benign, and patients typically present with symptoms related to the affected cranial nerve. Accurate preoperative diagnosis is possible because of their characteristic features on magnetic resonance imaging (MRI).1,2 Among nonvestibular schwannomas of the brain, trigeminal nerve schwannomas are the most common, comprising 0.8 to 8.0% of all intracranial schwannomas.3–5 Other nonvestibular schwannomas of the brain are rare. Schwannomas originating from oculomotor,6,7 trochlear,8–10 and abducens nerves11–13 are extremely rare even when associated with neurofibromatosis. The majority of patients present with isolated cranial nerve (CN) deficits of the nerve harboring the tumor or symptoms of brainstem compression or hydrocephalus. When these tumors are localized to the cavernous sinus, they present with either cavernous sinus symptoms or an orbital apex syndrome (multiple deficits of CN III–VI). As of February 2008, only two case reports described the use of stereotactic radiosurgery (SRS) for trochlear and abducens schwannomas.14,15 Facial sensory dysfunction is the most common presenting symptom, although some patients present with trigeminal neuralgia. Despite advances in skull base surgery techniques, complete resection of trigeminal schwannomas remains a challenge for neurosurgeons. Surgical removal has been associated with a significant risk of new neurologic deficits and is not complete in most cases.4,13,16–19 Based on its favorable response for other nerve sheath neoplasms, SRS has been applied to the management of trigeminal schwannomas to improve patient outcomes. Facial nerve schwannomas arise from any segment of the nerve, from the cerebellopontine angle to the extracranial peripheral portion of the nerve. Facial weakness and hearing disturbances are the two principal symptoms of facial nerve schwannoma. Patients occasionally present with facial muscle spasms preceding the onset of facial weakness. Because facial palsy is a common sequela after attempted surgical resection, SRS was applied as a strategy to improve preservation of facial function. Glossopharyngeal nerve schwannomas are the most common schwannomas in the region of the jugular bulb, followed by schwannomas of CN X, XI, and, rarely, XII. Tumors originating and expanding the jugular bulb result in progressive lower cranial nerve disorders. Larger jugular region tumors may extend from the intracranial to the extracranial compartment, leading to a dumbbell shape. Tumors expanding in the posterior fossa primarily present with deafness, vertigo, and ataxia, thereby mimicking vestibular schwannomas; involvement of lower cranial nerves is uncommon or late. Tumors arising in the jugular foramen and expanding extracranially present with hoarseness, a diminished gag reflex, and shoulder weakness, that is, a typical jugular foramen syndrome. Hypoglossal nerve schwannomas can be completely intracranial, intracranial/extracranial, or completely extracranial. Symptoms differ, depending on the location of the tumor. Tongue wasting is present for the majority of patients at the time of presentation. Suboccipital headaches, exacerbated by neck movements, are early symptoms of intracranial tumors. Patients with intracranial tumors may also exhibit jugular foramen cranial neuropathies or symptoms of brainstem compression. Between August 1987 and June 2007, 81 patients with nonvestibular schwannomas underwent Gamma Knife (Elekta Instruments AB, Stockholm, Sweden) SRS at our institution, the Center for Image-Guided Neurosurgery at the University of Pittsburgh Medical Center Presbyterian (Table 13.1). Radiosurgery was performed with the model U, B, C, or 4-C Leksell Gamma Knife. Our radiosurgical technique has been described in detail in previous reports.20 The procedure began with application of a model G Leksell stereotactic frame under conscious sedation and local scalp anesthesia, except in younger children, who underwent general anesthesia. After attaching a fiducial system to the frame, all patients underwent high-resolution MRI. A three-dimensional (3D) localizer sequence, which included axial, coronal, and sagittal images, was performed first. The tumor was then imaged using 3D gradient recalled sequence images. T2-weighted MRI using fast spin echo technique also was acquired to assess any suggestion of regional tumor infiltration. The images were exported to a computer workstation via the hospital Ethernet for dose planning. In all tumors the radiosurgery treatment volume was defined by the enhancing tumor volume. All patients received an intravenous dose of 20 to 40 mg of methylprednisolone after radiosurgery, and all were discharged from the hospital within 24 hours. After SRS, the patients were instructed to have clinical and imaging follow-up every 6 months during the first year, then yearly for 2 years. If tumor growth was halted, additional imaging evaluations were requested at 4, 6, 8, and 12 years. If a new symptom or any existing cranial nerve function worsened, the patient was evaluated for tumor progression or an adverse radiation effect (ARE). A new MR image was then obtained to assess tumor status and the effect of SRS. From March 2000 to October 2007, eight patients with schwannomas originating from oculomotor nerves (n = 2), trochlear nerves, (n = 5), or abducens nerves (n = 1) underwent SRS. The mean age of the patients was 46.1 years (range 19 to 59). Two patients had a medical history of neurofibromatosis: one had an oculomotor schwannoma, which recurred after surgery, and the other patient had a trochlear schwannoma. This latter patient also had a small vestibular schwannoma in the ipsilateral cerebellopontine angle. Both tumors underwent SRS at the same procedure. One patient (oculomotor schwannoma) underwent adjuvant radiosurgery for recurrence after prior surgery. For seven patients with tumors, SRS was used as a primary treatment. The diagnosis in these patients was based on (1) the individual patient’s neuro-opthalmological signs that were compatible with the specific cranial nerve and (2) MRI findings of the tumors that confirmed a tumor with typical imaging characteristic of a schwannoma. The patients’ chief complaints at the time of Gamma Knife radiosurgery were diplopia (n = 5), ptosis (n = 1), complete third nerve palsy (n = 1), and headache (n = 1). In patients with trochlear schwannomas, diplopia was due to impaired function of the ipsilateral superior oblique muscle. The symptom duration of diplopia ranged from 6 months to 4 years. Two patients had oculomotor schwannomas; one had complete ptosis after initial resection was attempted. The other patient exhibited periodic episodes of third nerve palsy and headache. The patient with abducens nerve schwannoma reported periodic headache. The median and mean tumor volumes were 0.22 and 1.32 cc, respectively (range 0.03 to 7.40). A median margin dose of 12.5 Gy (range 11.0 to 13.0) was prescribed to the tumor margin. We evaluated 33 patients with trigeminal schwannoma who had a minimum of 1-year follow-up. There were 17 men and 16 women, with a median age of 49.5 years (range 15.1–82.5 years). Eleven patients (33%) had undergone attempted resection, and one had prior stereotactic biopsy. Twenty-two patients (67%) underwent SRS as the primary procedure. The tumors were classified into root type (tumor predominantly located in the posterior fossa), ganglion type (tumor predominantly located in the middle fossa), and dumbbell type (tumor involving both the middle and posterior fossa).21 The median tumor volume was 5.0 cc (range 0.5–18.0 cc). The median prescription dose delivered to the margins of the tumor was 15 Gy (range 12–22 Gy), and the maximum dose was 30 Gy (range 24 to 40 Gy). Six patients had radiosurgery for facial nerve schwannomas and were eligible for evaluation at a minimum of 26 months (range 12–64 months). The mean patient age was 39 years (range 19–59 years). Four patients were male, and two were female. No patient had neurofibromatosis. No patient received prior fractionated radiation therapy. Three had a prior resection, and in three the diagnosis was made based on imaging and clinical criteria. All patients had facial nerve symptoms (five with weakness and one with muscle twitching). Headache was noted by one patient. In the three patients with a prior resection, two had a reduction in hearing before surgery (speech discrimination scores of 80% and 30%). After surgery (and before SRS), two had a significant hearing decline to deafness on that side, and the other patient had a slight reduction from 80 to 72% speech discrimination at 85 dB. At the time of radiosurgery, House–Brackmann facial function grades were I (n = 1), II (n = 3), III (n = 1), and VI (N = 1). The radiosurgery margin dose was 12.0 to 12.5 Gy. The mean tumor volume was 1.75 mL. Five of six tumors had volumes < 1 mL, and one tumor was 8.7 mL. After radiosurgery, patients were evaluated with serial imaging and clinical assessments.
Stereotactic Radiosurgery for Nonvestibular Schwannomas
Ajay Niranjan, Hideyuki Kano, In-Young Kim, Douglas Kondziolka, and L. Dade Lunsford
 Materials and Methods
Materials and Methods
Oculomotor, Trochlear, and Abducens Schwannomas
Trigeminal Schwannomas
Facial Nerve Schwannomas
Jugular Foramen Schwannomas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree