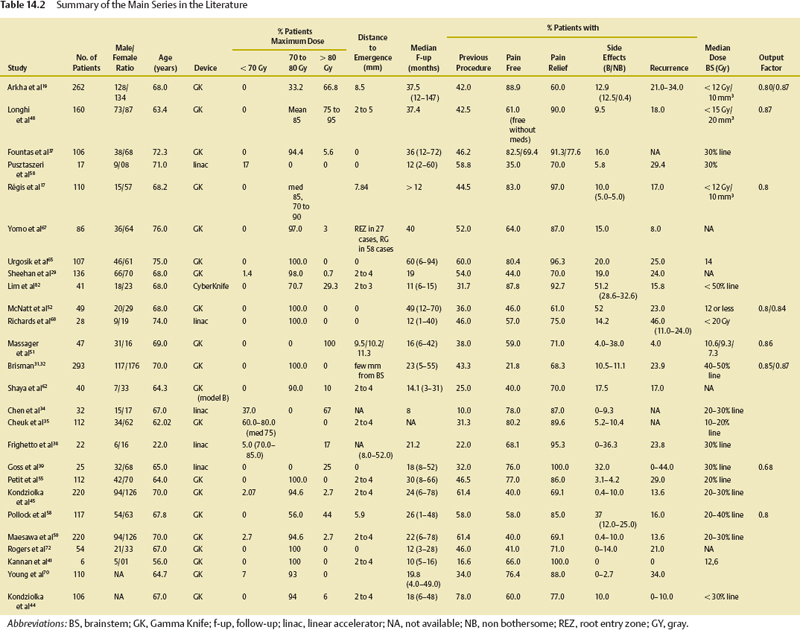
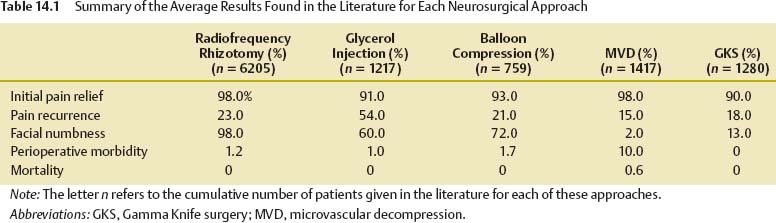
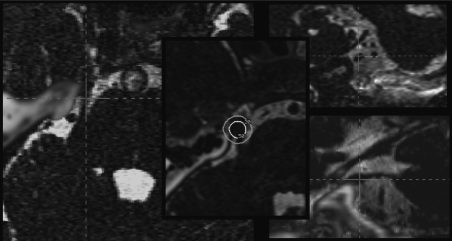
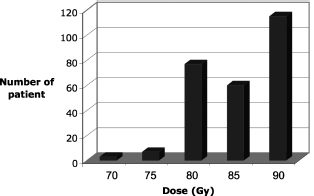
14 Trigeminal neuralgia, also known as tic douloureux, is a serious health problem, with a prevalence rate of 4 to 5 per 100,000 people.1 Patients typically describe a severe and sudden pain in the face, like an electric shock.2 There is growing evidence that, in most patients, one of the causal factors is compression of the trigeminal nerve root, close to its entry into the pons, by an aberrant arterial or venous loop.3 Microvascular decompression (MVD), first described in the 1950s by Taarnhoj,4 treats the putative cause by separating the loop from the trigeminal nerve. The pain may be effectively treated by a series of percutaneous techniques (thermocoagulation, microcompression, and glycerol injection) that produce a partial lesion of the trigeminal nerve.5–12 The concept of stereotactic radiosurgery was introduced by Lars Leksell, who, in 1951, first began performing clinical radiosurgery with a stereotactic x-ray beam on patients suffering from essential trigeminal neuralgia.13–15 The use of the Gamma Knife (Elekta Instruments AB, Stockholm, Sweden) with 201-source cobalt 60 was finally adopted in 1968. However, because of the efficacy of this tool in the treatment of other diseases, the introduction of the glycerol technique and later of effective drugs for the treatment of trigeminal neuralgia, and, primarily, the absence of high-quality neuroimaging for targeting, at this time the Gamma Knife was temporarily abandoned for this indication. The availability of high-quality three-dimensional magnetic resonance imaging (MRI) for precise targeting of normal structures and evidence of certain limitations of other techniques prompted a reappraisal of Gamma Knife surgery for trigeminal neuralgia in the 1990s.16 The evidence for safety and efficacy is based on retrospective case studies and one recent prospective trial.17 The evidence supporting the use of other modalities of surgical treatment for trigeminal neuralgia is based only on retrospective case studies.1 Additionally, the numerous studies published to date have not used uniform outcome measures, making a comparison between techniques difficult.18 It must be acknowledged that none of the currently available techniques are perfect (Table 14.1), thus explaining the continuing effort of neurosurgeons to develop new treatment methods. All these treatments must be rigorously evaluated to know how best to help these patients. Table 14.2 compares published studies according to the device used, either Gamma Knife, CyberKnife, Novalis, or adapted linear accelerator (linac); the percentage of patients treated, with the maximum dose <70 Gy, between 70 and 80 Gy, and >80 Gy; the distance between the center of the shot and the emergence of the nerve; the median follow-up and extreme values of follow-up (given in parentheses); the percentage of patients previously operated (for ipsilateral trigeminal neuralgia); the percentage of patients pain free at the time of the last follow-up; the percentage of patients with pain relief and side effects (B/NB bothersome vs non bothersome); the dose delivered to the brainstem (evaluated differently by the different authors); and the output factor used for the 4 mm helmet. Note that the worst results in terms of pain control are seen in the study using the lowest dose as the maximum (<70 Gy). The highest rates of toxicity are seen in those studies using the more posterior shot with a very short distance between the center of the shot and the emergence of the nerve, especially when high doses are used. The heterogeneity of clinical results after radiosurgery is suggestive of the strong impact of pre- and perioperative parameters. To better define the role of Gamma Knife surgery in the treatment of drug-resistant trigeminal neuralgia, a clear understanding of the impact of these parameters is mandatory. In 2006, we published the only prospective trial in line with the strict criteria proposed by Zackrzewska and Lopez18 and with a minimum follow-up of 1 year.17 More recently, we analyzed the long-term outcome in our overall experience.19 In this chapter, we will critically analyze these results and those from the literature. Since 1993 our trigeminal neuralgia radiosurgery cases have been evaluated prospectively, with the primary objective to investigate if single Gamma Knife surgery treatment of the cisternal part of the trigeminal nerve root for trigeminal neuralgia resulted in a decrease and/or cessation of pain attacks for each patient compared with before Gamma Knife surgery. The secondary objectives were to estimate changes in the intensity of pain attacks per day, the mean number of pain attacks, and the neurologic examination and search for the influence of the pre- and perioperative parameters on the safety efficacy variables. The diagnosis of trigeminal neuralgia was made according to the International Headache Society definition; its definitions of primary or secondary cases and typical versus atypical were also employed.2 Prior to treatment, each patient underwent the same routine diagnostic procedures, including MRI. We included patients with a clear clinical profile corresponding to trigeminal neuralgia2 and with a persistent pain level during the previous month of mean intensity superior to 5/10 on the visual analogue scale (VAS), despite optimized drug therapy (or drug therapy limited by dose-related side effects). None of the patients had a lesion adjacent to the trigeminal pathways, as shown using MRI.2 We excluded those patients who were pregnant and women who were breastfeeding. The procedure on the day of Gamma Knife surgery treatment was started with application of the Lek-sell stereotactic frame (Elekta) to the patient’s head, under local anesthesia. After the frame fixation, MRI and computed tomography (CT) were used for the dose planning with the Leksell GammaPlan (Elekta). The MR images were calibrated before examination and verified by comparison to the CT images to minimize magnetic distortion errors. One single exposure with the 4 mm collimator was placed on the anterior part of the cisternal portion of the trigeminal nerve (Fig. 14.1). The theoretical aim was to deliver a dose of 90 Gy as the maximum. However, the maximum dose was determined integrating the measured dose to the brainstem and the age of the patient. Multiple sclerosis was also considered to necessitate a lower dosage (Fig. 14.2). Leksell Gamma Knife (Model B, Elekta) treatment proceeded according to routines of the department, and the patients were discharged within 12 hours after radiosurgery. All the procedures were performed by the same neurosurgeon (JR). Clinical examination was performed before and > 1 year after Gamma Knife surgery, including corneal reflex, eye examination, skin examination, pinprick test, and sensitivity examination (search for hypoesthesia). MRI was systematically performed in all patients before radiosurgery but was not routinely repeated during the follow-up. Fig. 14.1 Dose planning displayed in axial view. On high-resolution stereotactic magnetic resonance imaging (MRI; constructive interference steady state [CISS] sequence, Siemens 1.5 T) fused with the bony window of the high-resolution computed tomography (CT) scan, a single 4 mm isocenter is positioned on the anterior portion of the nerve around 7.5 mm from its emergence at the level of the brainstem. Note the spatial relationship between the trigeminal incisura of the petrous bone apex and the plexus triangularis of the trigeminal nerve. Based on this landmark visible on a nonenhanced CT scan, radiosurgery can be performed safely and efficiently in a patient presenting with a pacemaker, contraindicating MR examination. Outcome measures used here are defined as follows:17 A recurrence was defined as the change from class I to a lower outcome class. Thus, the situation of a patient who had been pain free without medication (class I) and who then restarted taking specific drugs but who remained pain free on medication (class II) was considered as a “recurrence.” A minor recurrence was defined as well tolerated by the patient (lower frequency and intensity of pain) and not requiring the proposal of a new surgical therapy. A major recurrence was defined as requiring consideration of a further surgical procedure. Included in the study were 334 patients, 262 of whom were assessable for more than 1 year of follow-up.2 The median follow-up was 37.5 months (range 12–147 months). Our published results and those from the main literature series are summarized in Table 14.2. Two hundred and sixty-two patients were treated (128 males and 134 females), with an age range from 29 to 90 years (median age 68 years). The median duration of the disease was 74 months (mean 111.7 months; range 10–529 months). The side affected was the left in 128 cases and the right in 134. Twenty-one patients had multiple sclerosis. Eighty-one of 110 patients (73.6%) reported severe side effects from the drug therapy. A vascular conflict with the trigeminal nerve was clearly demonstrated by preoperative MRI in 167 patients (64%). Before radiosurgery, 110 patients had already been operated, with thermocoagulation (1–3 times) in 64 patients, balloon microcompression (1–3 times) in 53, surgical MVD in 27, glycerol rhizolysis in 7, pars major microsurgical partial section in 1, and Gamma Knife surgery in 1. Gamma Knife surgery was performed as the first surgical operation in 152 patients. The median maximum dose was 85.0 Gy (minimum 70.0 Gy; maximum 90.0 Gy). The median dose rate was 1.45 Gy (range 1.25–1.65 Gy). The output factor for dose calculation at this time was 0.80. The median of the distance between the center of the isocenter and the emergence was 8.5 mm. The median of the maximum dose to the brainstem (calculated as the point of the dose–volume histogram corresponding to the 10 mm3 receiving the highest dose; in other words, the maximum dose received by > 10 mm3 of the brainstem) was 10.8 Gy (0–16 Gy). No technical failure was encountered. Initial pain relief occurred in 88.9% of the patients after a median delay of 15 days (range 0–72 weeks) after Gamma Knife surgery (Table 14.2). Ninety patients (34%) reported pain recurrence 1 to 72 months after initial relief (Fig. 14.2), with a median delay of 10 months. An actuarial curve describing the pain-free probability according to time19 demonstrates a plateau at 5 years with a rate of pain freedom of 60%. Due to treatment failure or insufficient pain relief, 55 patients (21%) received additional surgical treatment, namely, a microcompression in 9 patients and a thermocoagulation in 11 patients, including 4 who received both. One patient underwent MVD. All these patients have been followed for > 1 year after this new surgery. Seven of these 17 patients (42%) had received surgical treatment between 1 and 4 times prior to inclusion in the study.19 Not infrequently, patients who were pain free were reluctant to stop their medication completely, due to anxiety about the risk of recurrence. A new functional disturbance of the V nerve was reported in 34 patients (12.9%) in the long term, with a median onset delay of 12 months.2–64 This disturbance was described as not disabling in 8 patients (3.05%), a minor discomfort in 21 (8%), bothersome in 5 (1.9%), and very bothersome in 1 (0.4%). The median delay for hypoesthesia onset was 10 months (range 1–72 months). An actuarial curve describing the hypoesthesia-free probability according to time19 demonstrates a plateau at 5 years with a rate of hypoesthesia freedom of 83%. There was no significant change in corneal reflex, eye examination, or skin examination during the study. None of the patients experienced dry eyes, keratitis, masseter weakness, neuropathic pain, or anesthesia dolorosa. The statistical analysis of our overall series19 demonstrated that a past history of surgical treatment of the trigeminal neuralgia on the same side was a predictor of toxicity in both univariate analyses (p = 0.0026) and multivariate analyses (p = .006). A small diameter of the ipsilateral trigeminal nerve (p = .0201) and a low ratio of diameters reflecting an important difference in size, with an ipsilateral nerve smaller than the contralateral nerve (p = .0218), are predictors of toxicity only in univariate analyses. Positive predictors of success were found to be a higher dose delivered to the plexus triangularis (p = .0498), maximum dose to the brainstem, does delivered to the emergence of the nerve (p = .0016), minimum dose delivered to the nerve (p = .0199), smaller volume of the ipsilateral trigeminal nerve (p = .0073), and smaller distance between the center of the shot and the anatomical emergence of the nerve (p = .049). A history of multiple sclerosis was clearly a predictor of failure. In our prospective trial,17 we found that the probability of pain freedom at the time of the last follow-up was lower in patients younger than age 60 (66.7% instead of 90.9%; p = .01) or with a “trigeminal cistern surface” >39 mm2 (72.0% instead of 89.5%; p = .05. There was an almost significant (p = .059) difference in the change in the number of attacks when patients with previous surgical treatment were compared with those without. The rate of failure at the last follow-up was 11.7% in patients never operated on as compared with 19.5% in patients previously operated. In the early 1990s, the availability of high-resolution MRI and the discovery of the limits of the other surgical alternatives promoted the reappraisal of Gamma Knife surgery in essential trigeminal neuralgia.20 Rand and colleagues suggested the target shift from the gasserian ganglion to the cisternal nerve.16 Hakanson and Lindquist21 promoted the concept of the dorsal root entry zone (DREZ). In 1993, Alexander and Lindquist21 defined the anatomical DREZ from a dose-planning point of view as follows: “a 4 mm collimator centered on the trigeminal root entry zone treated with a dose of 70 Gy to the center, including the nerve root and the adjacent brainstem within the 50% isodose surface (35 Gy).”21 I met Bob Rand in Paris in 1992, and he told me that, in his experience, the cisternal posterior target was not safe and recommended that high dosages ~90 Gy be used on the anterior cisternal portion. Since this discussion, the custom at the Timone University Hospital in Marseille has been to use a more anterior cisternal target that we call the retrogasserian or plexus triangularis target (Fig. 14.1). The plexus triangularis made sense because of the work of Sindou et al demonstrating that when the tip of the probe in thermocoagulations was located at the level of the plexus, the rate of pain cessation was high and the risk of toxicity much lower.10 Similarly, groups using balloon microcompression have found converging results (when the balloon extends into the posterior fossa, with a strong compression of the plexus triangularis, which displays a pear or diabolo shape).22,23 Finally, retrogasserian sections were historically performed at the location of the plexus triangularis.25 Reviewing our experience, the optimum distance from the emergence of the nerve has in fact turned out to be 7.5 to 8.0 mm.20 In Tokyo, we reported on our first series of trigeminal neuralgia treated with Gamma Knife surgery using 90 Gy and the plexus triangularis target.25 Interestingly, Doug Kondziolka mentioned on this occasion that he quite systematically obtained failures using much lower dosages and proposed to evaluate the impact of the maximum dose on the probability of pain cessation. Kondziolka and colleagues at the University of Pittsburgh,22 later aggregated the first cases from Los Angeles, Marseille, Pittsburgh, Rhode Island, and Seattle. Their study, based on the assumption that the target was the same in all cases, demonstrated that the maximum dose played a major role in the efficacy of the treatment, with no effect on its safety.26 Specifically, patients treated with a maximum dose <70 Gy very rarely experienced pain alleviation. Thus, 70 Gy as the maximum became a standard dose for those using the “Pittsburgh way.” Since this time the position of our team has been to insist on the fact that this pioneering study carried an important bias in the heterogeneity of the anatomical targets used.17,20,27 Thus, we considered that further trials were mandatory to elucidate the best treatment parameters for the best safety/efficacy, before defining the role of Gamma Knife surgery among the other surgical alternatives.17,28–30 Two articles published in the Journal of Neurosurgery in 2005 in the same issue (associated with a negative editorial) reported very poor middle/long-term results of Gamma Knife surgery in trigeminal neuralgia, with 71 and 21% excellent/ good results at 6 months and 2 years, respectively, in Tawk et al30 and 47, 45, and 34% excellent/good results at 1, 2, and 3 years, respectively, in Sheehan et al.29 Importantly, the maximum dose in these series was heterogeneous (50–90 Gy in Sheehan et al30), with a low rate of 9% of facial numbness.28–30 There are huge discrepancies between treatment centers in terms of the results reported (Table 14.2
Stereotactic Radiosurgery for Trigeminal Neuralgia
Jean Régis, Noriko Murata, Shoji Yomo, Yasser Arkha, Philippe Roussel, and Anne Donnet
 Materials and Methods
Materials and Methods
 Results
Results
 Discussion
Discussion
Predictors of Pain Cessation, Pain Recurrence, and Toxicity in Radiosurgery for Trigeminal Neuralgia
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree