Strategic planning is becoming essential to neuroradiology as the health care environment continues to emphasize cost efficiency, teamwork and collaboration. A strategic plan begins with a mission statement and vision of where the neuroradiology division would like to be in the near future. Formalized strategic planning frameworks, such as the strengths, weaknesses, opportunities and threats (SWOT), and the Balanced Scorecard frameworks, can help neuroradiology divisions determine their current position in the marketplace. Communication, delegation, and accountability in neuroradiology is essential in executing an effective strategic plan.
- •
Strategic planning requires an assessment of the current position of a neuroradiology division and a vision of where the neuroradiology would like to be in the near future.
- •
Two commonly used strategic frameworks are the strengths, weaknesses, opportunities, and threats (SWOT) framework and the balanced scorecard framework, which examines an organization from four perspectives: customer, learning and growth, internal business process, and financial.
- •
Implementing a strategic plan requires delegation, deadlines, and accountability among those in the organization tasked with implementation.
Introduction
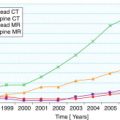
For many years radiology enjoyed a period of tremendous growth. This advancement was largely due to the advent of new technology, which greatly expanded the diagnostic capabilities of imaging. In neuroradiology, pneumoencephalography became obsolete, and the new cross-sectional modalities of CT and MRI vastly increased the diagnostic armamentarium neuroradiologists use to diagnose central nervous system disorders. New nonimaging medical and surgical technologies also increased patient life expectancies, contributing to higher imaging volume in radiology in general, and in neuroradiology particularly. Between 1999 and 2004, imaging was the fastest growing physician service, and CT and MRI of the central nervous system grew proportionately with other imaging services.
Although the rapid rate of imaging growth dramatically expanded the role of neuroradiology in clinical practice, the expensive nature of neuroimaging was problematic from an economic and strategic planning viewpoint. Technologically sophisticated medical and imaging technologies are cost-intensive, and recently it has become evident that health care expenditures in the United States have increased to the point of potentially being unsustainable. United States health care spending was nearly $2.6 trillion in 2010, over 10 times the amount spent in 1980. To maintain United States competitiveness, increasing attention has been devoted to curbing the growth rate of health care expenditures, with a particular focus on imaging. These economic constraints make effective strategic planning for neuroradiologists essential.
Strategic planning for neuroradiology
Strategic planning for any organization can be loosely defined as envisioning a future for an organization and working backward to determine a plan of action designed to reach the desired goal. To do so requires several steps that can be conceptualized as vision, assessment, plan of action, and execution of the plan to achieve the desired goals. Although this methodology intuitively seems straightforward, the strategic planning process is, in fact, difficult. One of the primary reasons is that a desired future cannot be envisioned or achieved in a vacuum; organizations must take stock of the external forces continually influencing them, and at the same time accurately assess their own positive and negative attributes and their willingness and ability to respond to environmental change. Strategic planning also requires prediction and assessment of trends. In radiology in general, and in neuroradiology in particular, this is highly challenging. Commoditization, teleradiology, declining reimbursement, utilization management, political shifts, and technological uncertainty all make the construction of long-standing predictions in neuroradiology problematic ( Box 1 ). Not surprisingly, the rapidly evolving health care environment only reinforces the need for neuroradiology leadership organizations to have a cohesive and ongoing strategic planning framework in place.
Commoditization: a commodity is defined as a good or service that is only differentiated in the customer’s mind by price. If patients see all neuroradiologists as equal in every fashion, they will look toward price as a differentiator.
Teleradiology: teleradiology uses digital picture archiving and communications systems to transport neuroradiology images to an off-site location to be interpreted. When interpretations are moved off-site, other aspects of the role of the neuroradiologist, such as guiding the selection of an appropriate imaging examination, may be overlooked at the primary site.
Declining reimbursement: declining reimbursement can be defined as an overall decrease in payments for radiologic services. Usually this practice is put into place by payors to cut costs.
Utilization management: utilization management in radiology refers to the overseeing of the ordering patterns of radiologic studies by referring physicians through the use of certain criteria that are in some cases proprietary to the utilization manager. Utilization management most often has the effect of decreasing the overall amount of radiology procedures requested.
Political shifts: different political leaders enact policies that influence the overall health care system in a variety of ways, and many policies impact the practice of neuroradiology.
Technological obsolescence: technology is constantly evolving, making some procedures in neuroradiology, such as routine skull examinations, not as clinically useful as other procedures, such as MRI. Shifting technology can influence neuroradiology strategic planning and capital budgeting.
Strategic planning for neuroradiology
Strategic planning for any organization can be loosely defined as envisioning a future for an organization and working backward to determine a plan of action designed to reach the desired goal. To do so requires several steps that can be conceptualized as vision, assessment, plan of action, and execution of the plan to achieve the desired goals. Although this methodology intuitively seems straightforward, the strategic planning process is, in fact, difficult. One of the primary reasons is that a desired future cannot be envisioned or achieved in a vacuum; organizations must take stock of the external forces continually influencing them, and at the same time accurately assess their own positive and negative attributes and their willingness and ability to respond to environmental change. Strategic planning also requires prediction and assessment of trends. In radiology in general, and in neuroradiology in particular, this is highly challenging. Commoditization, teleradiology, declining reimbursement, utilization management, political shifts, and technological uncertainty all make the construction of long-standing predictions in neuroradiology problematic ( Box 1 ). Not surprisingly, the rapidly evolving health care environment only reinforces the need for neuroradiology leadership organizations to have a cohesive and ongoing strategic planning framework in place.
Commoditization: a commodity is defined as a good or service that is only differentiated in the customer’s mind by price. If patients see all neuroradiologists as equal in every fashion, they will look toward price as a differentiator.
Teleradiology: teleradiology uses digital picture archiving and communications systems to transport neuroradiology images to an off-site location to be interpreted. When interpretations are moved off-site, other aspects of the role of the neuroradiologist, such as guiding the selection of an appropriate imaging examination, may be overlooked at the primary site.
Declining reimbursement: declining reimbursement can be defined as an overall decrease in payments for radiologic services. Usually this practice is put into place by payors to cut costs.
Utilization management: utilization management in radiology refers to the overseeing of the ordering patterns of radiologic studies by referring physicians through the use of certain criteria that are in some cases proprietary to the utilization manager. Utilization management most often has the effect of decreasing the overall amount of radiology procedures requested.
Political shifts: different political leaders enact policies that influence the overall health care system in a variety of ways, and many policies impact the practice of neuroradiology.
Technological obsolescence: technology is constantly evolving, making some procedures in neuroradiology, such as routine skull examinations, not as clinically useful as other procedures, such as MRI. Shifting technology can influence neuroradiology strategic planning and capital budgeting.
Vision and mission statement
A neuroradiology division cannot develop a strategic plan without a vision and mission statement. The vision can be defined as a view of where the neuroradiology division would like to position itself both internally and in the external environment in the present and near future. The mission statement is a written expression of the vision. A good mission statement should be coherent, concise, and timeless, and should elucidate the purpose of the neuroradiology division and its priorities. The mission statement should be familiar to all employees of the neuroradiology division. Superficially, the priorities of a neuroradiology division may seem straightforward: to preserve human life through neuroimaging. However, a deeper examination of the neuroradiology division priorities suggests a more complicated picture, with varying levels of prioritization for the various neuroradiology practice settings. For example, an academic neuroradiology department that relies on a large number of research grants for its financial health may value cutting edge research and peer reviewed publications in addition to, and occasionally more than, a high volume of clinical work. Other less grant-funded academic neuroradiology divisions may place teaching ahead of research, and still other community practice neuroradiology divisions may prioritize clinical output over teaching and research. Box 2 provides examples of two different mission statements. Obviously, no correct and uniform set of goals exists for neuroradiology departments, but priorities of any particular neuroradiology division must be integrated into the mission statement of the neuroradiology department so that strategic decisions align with the overall goals of the neuroradiology section.
Sample Mission Statement One: Our neuroradiology division strives to be a world leader in patient-oriented practice and neuroradiologic technological advancement, including image-based neuroscience and image-guided minimally invasive therapeutics. Our division also strives to provide a state-of-the-art training experience for future neuroradiology leaders.
Comment: With its emphasis on world leadership and teaching, this sample mission statement is probably more typical of an academic neuroradiology division.
Sample Mission Statement Two: Through state-of-the-art technology and clinical excellence, our neuroradiology division strives to provide our patients with the finest neuroradiologic experience in the region.
Comment: With its emphasis on regional dominance and patient experience and clinical excellence, this sample mission statement is probably more typical of a primarily clinical neuroradiology division.
A poorly constructed or ambiguous mission statement can contribute to ineffective decisions that do not align with a neuroradiology group’s strategic plan. For example, if a neuroradiology division has research as a top priority, taking on a contract to interpret additional off-site neuroimaging studies with the goal of increasing clinical revenue may not be advantageous if it decreases research quality. Conversely, in a community setting, neuroradiologists might be ill-advised to allocate significant capital expenditures to hire a researcher in lieu of updating their MRI equipment if their mission statement specifies that using state-of-the-art MRI technology is their top priority.
Strategic planning frameworks
To plan an appropriate course of action based on a vision requires that organizations take inventory of their own attributes and examine the external environment in which they operate. To help organizations achieve self-awareness, formalized strategic planning frameworks have been developed. Two commonly used strategic planning frameworks are the strengths, weaknesses, opportunities, and threats (SWOT) framework, developed at Harvard University in the late fifties, and the Balanced Scorecard framework, also developed at Harvard in the early nineties. Both strategic planning frameworks are helpful in providing an overall structure to conceptualize strategic planning, yet both have some limitations. The strategic planning frameworks are not mutually exclusive and can be used to complement each other.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree