SUBMANDIBULAR GLAND AND SPACE: INFECTIOUS AND NONINFECTIOUS INFLAMMATORY DISEASES
KEY POINTS
- Imaging, especially computed tomography, sometimes provides critical information in the management of submandibular gland/submandibular space infections and other inflammatory diseases.
- Imaging is key in determining whether a related abscess is present.
- Imaging can establish the source of a submandibular space or submandibular space region inflammatory process when it may not be clear clinically.
- Computed tomography and magnetic resonance imaging may identify changes suggestive of autoimmune sialoadenitis before that diagnosis is established clinically.
Many submandibular gland (SMG) and submandibular space (SMS) inflammatory conditions do not come to imaging. A significant proportion of these are dental infections (discussed in detail in Chapter 97). Imaging may be used to help in medical decision making when the source of inflammation is in question or if an abscess might be a complicating feature. Clinical examination of an acutely infected SMG/SMS may be limited by severe pain and toughness of the cervical fascia attachment to the mandible as well as the mandible itself. Sometimes, low-grade, chronic infections can mimic tumor and present predominantly as an SMG/SMS mass. Occasionally, in chronic infections, imaging will help to confirm the diagnosis and etiology and decide whether surgery should be part of the management plan.
Imaging in patients with chronic SMG/SMS region complaints may be the first indication of a salivary gland disease being related to a systemic condition—most often a manifestation of autoimmune disease and less commonly other systemic inflammatory disease as common as sarcoidosis and as rare as Kimura disease. Sometimes the distinction between infectious disease and noninfectious inflammatory disease and neoplasm (Chapter 179) is blurred, as with SMG manifestations associated with human immunodeficiency virus (HIV) infection and rheumatoid arthritis.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The important anatomic relationships that impact medical decision making in inflammatory diseases of the SMG/SMS are presented in Chapter 175 and include the following:
- Its relationships to the structures that bound the SMS, including the mandible, mylohyoid muscle and superficial fascia or platysma, and the lower parapharyngeal and masticator spaces
- Anatomy of the SMG main duct and intraglandular ductal system
- Course of the mandibular branch of the facial nerve and the lingual branch of V3
- Level 1 lymph nodes and their drainage patterns (Chapters 149 and 157)
IMAGING APPROACH
Techniques and Relevant Aspects
Computed Tomography
Specific computed tomography (CT) protocols for various indications appear in Appendix A and are discussed in more detail in Chapter 175. Theoretically, calcification might be masked by contrast use, but this does not justify the cost or radiation burden of routine pre- and postcontrast studies.
Magnetic Resonance Imaging
Specific magnetic resonance (MR) protocols for various indications appear in Appendix B. A steady state image may be included that allows for MR depiction of the ductal system, sometimes referred to as MR sialography.
Radionuclide Studies
Radionuclide studies are not used routinely for the evaluation of SMG masses. Those using technetium, iodine, and fluorine-18 2-fluoro-2-deoxy-D-glucose (FDG) are used in highly selected circumstances.
Ultrasound
Standard high-resolution scanning techniques as described in Chapter 4 are used. Ultrasound (US) and conventional sialography can be used as an adjunct to sialoendoscopy.
Conventional Sialography
Conventional sialography has been used very selectively since the 1980s, most recently in conjunction with endoscopic treatment of main duct pathology.
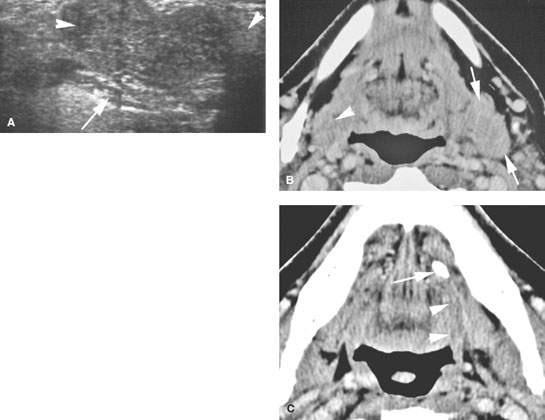
FIGURE 181.1. An adult presenting with a left submandibular region mass. A: Ultrasound (US) showing a lobulated mass in the submandibular gland (SMG) (arrows) deep to the mylohyoid muscle without evidence of ductal dilatation. No stone in the duct could be demonstrated with certainty. The examination was somewhat limited by the anatomy of the mandible in a patient who was somewhat short necked and had a fairly substantial-sized mandible. B, C: Images from a contrast-enhanced computed tomography study showing the left SMG to be enlarged but not obviously enhancing (arrows) compared to the right (arrowhead). In (C), the cause of the glandular changes was a stone impacted in the distal submandibular duct (arrow) with perhaps some periductal inflammatory changes that are of low grade (arrowheads) compared to the normal appearance of the posterior sublingual space on the opposite side. (NOTE: This case illustrates how chronic sialoadenitis can mimic a mass lesion and to some extent points out limitations of US in evaluation of a mass in this region, although sometimes US can be definitive with regard to medical decision making.)
Pros and Cons
General Approach
Magnetic Resonance and Computed Tomography
MR and CT are the most-used imaging studies to evaluate an acute SMG/SMS region infection. CT is preferred for its simplicity and to avoid the insensitivity of magnetic resonance imaging (MRI) to stones both within the ductal system and parenchyma (Figs. 181.1–181.7). The dimension of ductal system visualization added by MR sialography is typically not of enough critical value in cases of acute inflammation to supplant CT. In chronic inflammatory conditions, MR might be a first choice. Both CT and MRI might be deferred in favor of US and sialoendoscopy in the hands of experienced groups when main duct pathology is believed to be the most likely contributing factor (Fig. 181.8).
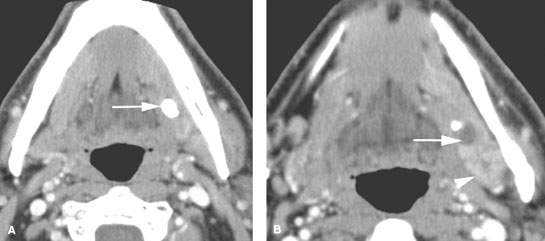
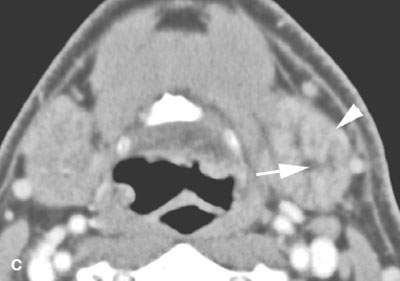
FIGURE 181.2. A patient with sialolithiasis and sialoadenitis. The patient presented with pain and tenderness in the submandibular region. A–C: Contrast-enhanced computed tomography study in (A) a stone impacted in the mid submandibular duct. In (B), the stone is seen to lie at the point where the main submandibular duct curves around the posterior edge of the mylohyoid muscle; proximal duct obstruction at that point is present (arrow). In (C), the submandibular gland is enlarged and enhancing abnormally compared to the normal opposite side, and its proximal intraglandular ductal system obviously is distended.
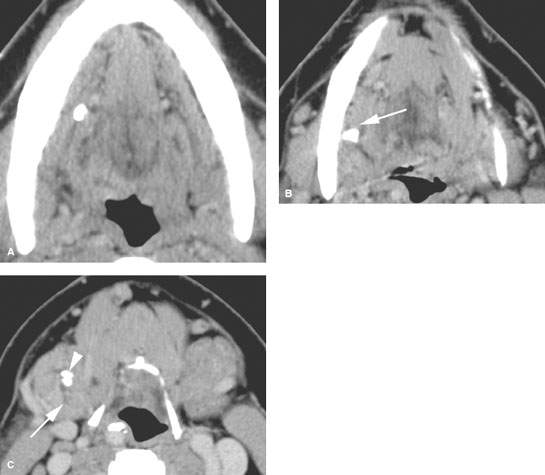
FIGURE 181.3. A patient with pain and tenderness in the right submandibular region. The contrast-enhanced computed tomography (CT) study shows this to be due to sialolithiasis and sialoadenitis. A: There is a stone impacted in the mid submandibular duct and a second stone impacted at the position where the duct crosses over the posterior edge of the mylohyoid muscle (arrow in B). C: A third stone is present in the more proximal ductal system at the point where the main duct branches into the even more proximal intraglandular ductal system (arrowhead), and there is dilatation of the branching ducts within the gland (arrow). (NOTE: This study indicates how CT imaging can be definitive with regard to the nature and extent of inflammatory submandibular gland disease, especially with regard to the presence and position of stones and the status of the gland itself. For the most part, imaging with CT has replaced sialography in the evaluation of such patients.
Ultrasound and Conventional Positive Contrast Sialography
US may be used to determine whether there is ductal dilatation or stones or an abscess. US alone may be enough imaging for triage to appropriate care in selected cases in the hands of experienced sonographers. This is especially true where teams that triage with US for potential follow-up sialoendoscopy are in place. Sialography may also fit well into such a triage scheme for main duct disease, possibly following a nondefinitive US in the diagnostic hierarchy (Fig. 181.1). However, contrast should be placed in the parotid duct with great caution if there is evidence of active inflammation and especially if the infectious agent may be a pyogenic bacterium.
The US parenchymal changes seen in noninfectious inflammatory diseases are nonspecific. Moreover, all of the major salivary glands are not studied and other regional anatomy including the cervical lymph nodes and lacrimal glands are not as simply studied as in a comprehensive head and neck imaging examination than with CT and MRI.
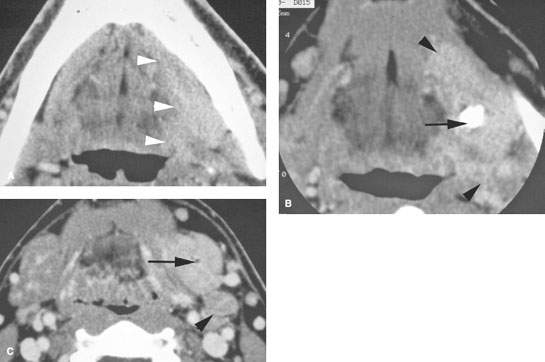
FIGURE 181.4. A patient with severe left submandibular region pain that could be due to an inflammatory process possibly of dental origin. Contrast-enhanced computed tomography was done. A: There is an intense cellulitis throughout the floor of the mouth along the mandible (arrowheads). B: Cellulitis is still noted (arrowheads) and seen to be due to inflammatory sialoadenitis related to obstruction by a stone. The study excluded a drainable fluid collection. The patient was treated with antibiotics, and the gland subsequently was removed. C: Enlargement and enhancement of the submandibular gland is obvious compared to the normal opposite side, and there is dilatation of the glandular ductal system (arrow) and reactive possibly early suppurative adenitis at level 2 (arrowhead).
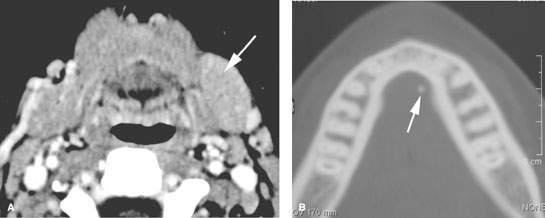
FIGURE 181.5. A patient presenting with chronic vague pain in the region of the left submandibular gland. Contrast-enhanced computed tomography in (A) shows enlargement and slight increased enhancement of the left submandibular duct compared to the right (arrow). In (B), there is a tiny stone within the submandibular duct near the region of the punctum. The stone was removed, and the patient’s symptoms resolved.
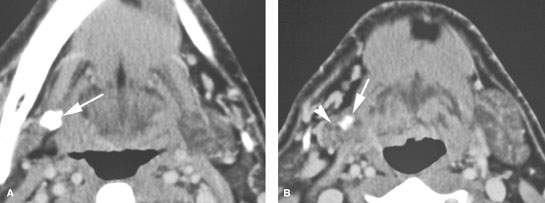
FIGURE 181.6. The chronic effects of sialolithiasis are illustrated in this patient who had contrast-enhanced computed tomography because of chronic pain at the angle of the mandible. The etiology was uncertain. A: A large stone is impacted in one of the more common areas where the main submandibular duct curves over the posterior edge of the mylohyoid muscle (arrow). B: The stone is still present, and a second stone is impacted within the ductal system (arrow). This has led to atrophy of the right submandibular gland, being much smaller than the normal gland (arrowhead) and showing some low-grade enhancement. Involutional changes such as these may be a manifestation of atrophy in the entire gland.
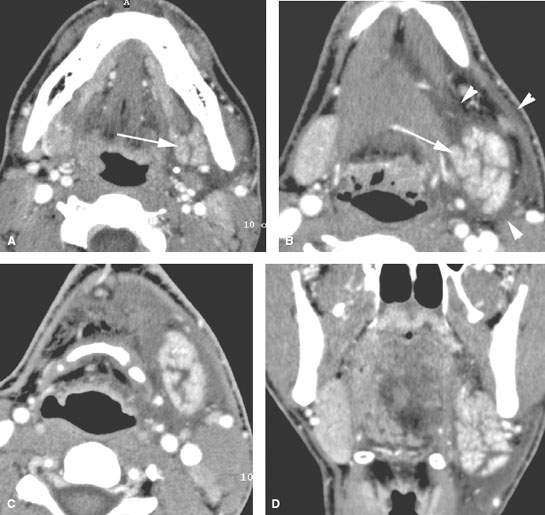
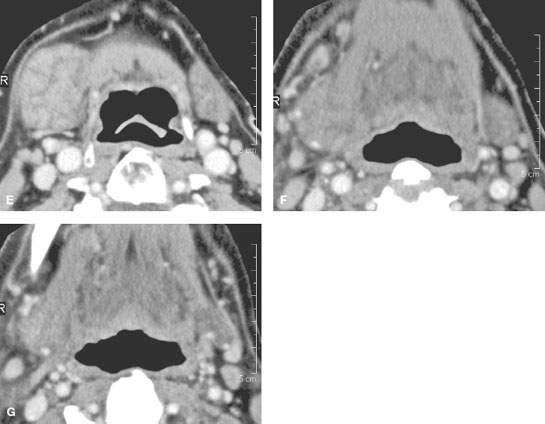
FIGURE 181.7. A–D: Patient 1 presenting with acute submandibular region pain and swelling. It was uncertain whether this was due to dental disease or disease within the submandibular gland (SMG). Contrast-enhanced computed tomography (CT) in (A) and (B) show marked enhancement of the SMG (arrows) and very extensive edema around the gland (arrowheads). In the axial section in (C) and coronal reformations in (D), there are glandular parenchymal changes and intense surrounding edema due to acute pyogenic infectious sialoadenitis. (NOTE: The patient’s symptoms resolved on antibiotics.) E–G: Patient 2 presenting with chronic pain and tenderness in the right submandibular region of uncertain etiology. Contrast-enhanced CT study in (A) shows low-grade enhancement and an obviously swollen right SMG without ductal dilatation or stones. The same findings are present in the remainder of the glands and along the sublingual space and floor of the mouth, as seen in (F) and (G).
Radionuclide Studies
Radionuclide studies are not used routinely for the evaluation of SMG/SMS infections.
Specific Indications
Specific indications for SMG/SMS infections include the following:
- Define the origin and extent of an SMG/SMS region infection. Does the infection arise from within the SMG (Figs. 181.1–181.9) or is it from an extrinsic source (Figs. 181.10 and 181.11)?
- Define whether the processes are likely of noninfectious or infectious cause (Figs. 181.12–181.16).
- Define the presence and extent of any abscess, whether related to the gland or arising extrinsic to the gland and its surrounding structures and spaces outside the SMG/SMS (Figs. 181.4 and 181.9).
- Identify ductal changes or sialolithiasis that might contribute to diagnosis and treatment plans (Figs. 181.1–181.9).
- Establish whether the changes may be part of generalized major salivary gland condition and/or possibly related to a systemic inflammatory process (Figs. 181.12–181.17).
Controversies
US may be promoted as a starting point in the evaluation of SMG/SMS inflammatory disease; however, the sonographic evaluation of the gland and space is limited to some extent by the bony confines of the mandible. Using US as a starting point is a very good approach, but only in experienced hands. Outside of that context, US becomes potentially cost additive and nondefinitive.
MR sialography has been promoted as a screening tool for Sjögren disease in the past. There are more cost-efficient and reliable means of establishing such a diagnosis. Sjögren disease is primarily a clinical diagnosis that is confirmed by serologic studies. In serologically negative patients with highly suspicious findings of dry eyes and mouth, imaging may aid in medical decision making. Unless there is a risk of significant reaction to iodinated contrast, MRI should defer to CT if an advanced imaging technique is necessary for medical decision making.
The value of using a combination of sialography and endoscopic treatment of ductal pathology is becoming more widespread. This is not controversial but does require a careful coordinated effort between the sialendocopist and the imaging team.
Acute and Subacute Pyogenic Bacterial Infections, Viral Infections, and Chronic Infections
Etiology
Viral infections are common in the parotid gland, but few SMG infections are attributed to that source. The most well known virus that may present as primarily SMG problems might be a manifestation of HIV infection, although those changes are usually seen in the context of obvious, usually bilateral, parotid disease (Fig. 181.16).
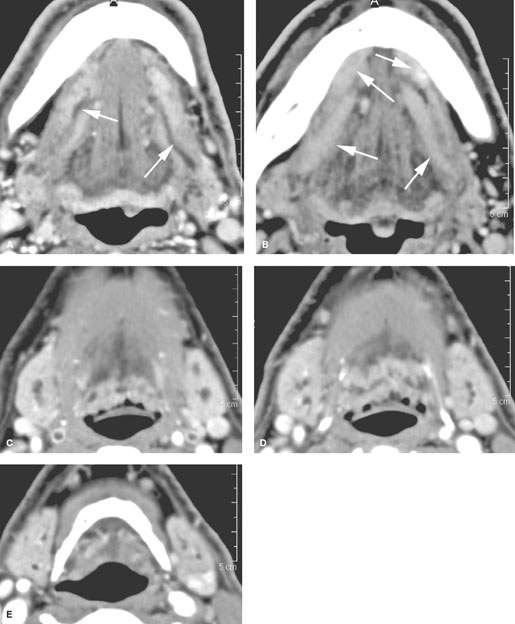
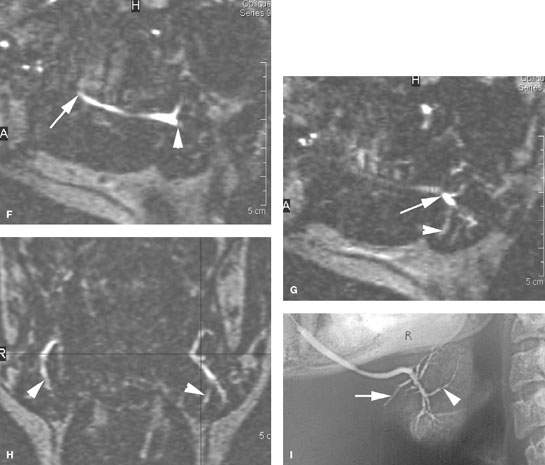
FIGURE 181.8. Three patients and three different imaging techniques to evaluate ductal pathology. A–E: Patient 1. A study to demonstrate the appearance of inflamed obstructed submandibular ducts. This patient had a very small cancer of the anterior floor of the mouth not visible on computed tomography (CT) and covering the puncta of both submandibular ducts. In (A), this results in dilatation of both main submandibular ducts (arrows) and some enhancements along the ductal systems, which secondarily affects the sublingual glands. In (B), the enhancement of the sublingual glandular tissue and periductal soft tissues is very extensive. In (C) through (E), the dilatation of the ductal system within both glands and abnormal enhancement of both glands reflects the bilateral obstructive sialoadenitis. F–H: Magnetic resonance (MR) sialography in Patient 2 to demonstrate the appearance of dilated ductal systems as seen on that examination. Steady state images were used to reconstruct those images seen in (F) through (H). In (F), an oblique sagittal plane shows the main submandibular duct from its punctum (arrow) to its area of entry into the submandibular duct as it crosses over the posterior edge of the mylohyoid muscle (arrowhead). The sagittal image in (G) shows the branch point of the main parotid duct into the ramifying ductal system within the gland (arrowheads). A coronal reformation in (H) shows the bilateral dilated ductal systems (arrowheads). (NOTE: While this so-called technique of MR sialography is capable of producing images of the dilated ductal system, it provides relatively limited detail of the ducts. MR in general will not be as satisfactory as CT for the demonstration of stones or the evaluation of structures in and around the submandibular space (SMS) that might be other sources of pathology that mimics SMS-origin pathology.) I: Patient 3. A sialogram showing relatively subtle changes in the ducts ramifying within the substance of the submandibular gland manifest by some degree of cutoff of the ductal system (arrow) and areas of structuring, narrowing, and irregularity (arrowheads). Such detail is not possible with MR sialography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








