Superior Vena Cava Obstruction
R. Brooke Jeffrey, MD
Key Facts
Imaging
Mediastinal nodes or masses, nonvisualization of SVC, multiple venous collaterals on CECT
Multiplanar reformations (maximum-intensity projection) to display venous collaterals
Opacification of portions of liver parenchyma through intra- and perihepatic collateral veins
“Hot quadrate” (medial segment) on sulfur colloid scan
Top Differential Diagnoses
Fibrosing mediastinitis
Aortic aneurysm or dissection
Pathology
Etiology
40% due to malignancy; bronchogenic carcinoma and lymphoma most common causes
Infectious processes, such as adenopathy, from histoplasmosis, tuberculosis, coccidiomycosis
Thrombosis due to hypercoagulable state, long-term indwelling SVC catheter, or pacemaker
Clinical Issues
Treatment
Steroids and diuretics for acute cerebral edema
Endovascular stenting for non-Hodgkin lymphoma
Emergent radiation therapy for lymphoma
Thrombolysis for acute SVC thrombosis
Surgical bypass for chronic benign obstruction
Diagnostic Checklist
Consider mediastinal fibrosis or tuberculosis if calcified nodal mass
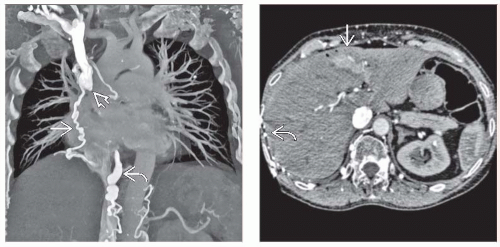 (Left) Coronal CECT in an elderly woman who presented with a puffy face demonstrates obstruction of the superior vena cava
Get Clinical Tree app for offline access
 , with collateral flow through an enlarged azygous vein , with collateral flow through an enlarged azygous vein  as well as various mediastinal collateral veins as well as various mediastinal collateral veins  . (Right) Axial CECT in the same patient again illustrates collateral veins . (Right) Axial CECT in the same patient again illustrates collateral veins  along the surface of the liver, with opacification of a portion of the medial segment along the surface of the liver, with opacification of a portion of the medial segment
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|