| SKULL BASE REGION | Suprasellar |
| HISTOPATHOLOGY | Metastasis, non–small cell lung carcinoma |
| PRIOR SURGICAL RESECTION | No – only biopsy |
| PERTINENT LABORATORY FINDINGS | N/A |
Case description
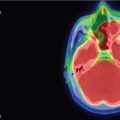
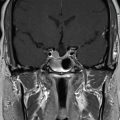
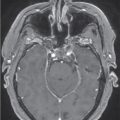
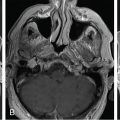
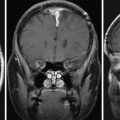
The patient is a 79-year-old woman with a 3-year history of non–small cell lung carcinoma, status post right upper lung lobectomy. She presented with episodes of progressive nausea and vomiting and was found to have diabetes insipidus. Imaging revealed a 1-cm enhancing lesion in the suprasellar region, adjacent to the optic chiasm and hypothalamus ( Figure 4.19.1 ). A stereotactic biopsy ( Figure 4.19.2 ) confirmed the diagnosis of a non–small cell lung metastasis, and the patient elected for stereotactic radiosurgery (SRS) ( Figure 4.19.3 ).
| Radiosurgery Machine | CyberKnife |
| Radiosurgery Dose (Gy) | 25, at the 71% isodose line |
| Number of Fractions | 5 |



| Critical Structure | Dose Tolerance |
|---|---|
| Optic nerve/chiasm | <5 Gy maximum point dose |
| Brainstem |
|
| Cranial nerves in cavernous sinus |
|
| Cavernous carotid artery |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree