Fig. 7.1
Various sizes of applicators are available which can be used according to the size of the surgical cavity after WLE
7.1 Obtaining Informed Consent
During the consent process, it is important to mention some important facts about IORT based on the evidence obtained from the randomised controlled trial. In the pre-pathology group, in around 15 % of cases, it may be necessary to recommend external beam radiotherapy (EBRT) to patients who had received IORT due to untoward histological features in the primary tumour or the lymph nodes, as outlined previously. This point needs to be mentioned to patients during pre-operative counselling. Patients should also be informed about the possibility of some hardening/induration of breast tissue around the area that receives IORT. This usually settles after 18–24 months. There is also a higher incidence of postoperative development of a seroma in the IORT group as compared with the EBRT group, although it is relatively uncommon in both treatments.
7.2 Scheduling
As IORT is a multidisciplinary procedure, it requires close collaboration between members of the team. The radiotherapy and the physics team need to be informed well in advance to ensure that they are available in theatre without affecting the routine activity of the department.
It is preferable to schedule the IORT cases earlier on the operating list in order to avoid keeping the whole extended team in the hospital out of hours. Routinely scheduling IORT on certain days of the week (e.g. every Tuesday morning) also helps all staff to plan their time.
7.3 Choice of Operating Theatre
During the commissioning process, it is important to choose an operating room with sufficient space to manoeuvre the INTRABEAM hydraulic arm in order to avoid risk of accidental damage to the electron drift tube. After it has been connected to the INTRABEAM, the protective guard for the electron drift tube should be maintained at all times and the hydraulic arm is kept in the “parking position” while the INTRABEAM is not in use in order to avoid accidental damage (Fig. 7.2).


Fig. 7.2
(a) A protective guard should be inserted before use to minimize accidental damage to the drift tube. (b) The hydraulic arm is maintained in the “parking position” at all times while the INTRABEAM is not in use in order to avoid accidental damage
7.4 Applicator Availability/Sterilisation
It is good practice to sterilise the applicators individually so that the appropriate size is chosen and used without opening other applicators. This approach will allow scheduling more than one case on the operating list, and other sterile applicators can be available for other scheduled cases. This also avoids repeated sterilisation of unused applicators.
7.5 Step-by-Step Description of the Procedure
7.5.1 Standard Wide Local/Segmental Excision and Mobilisation
After standard wide local excision (WLE) of the primary tumour, the remaining breast tissue is mobilised by dissecting the breast tissue from the overlying skin and subcutaneous tissue, as shown in Fig. 7.3.
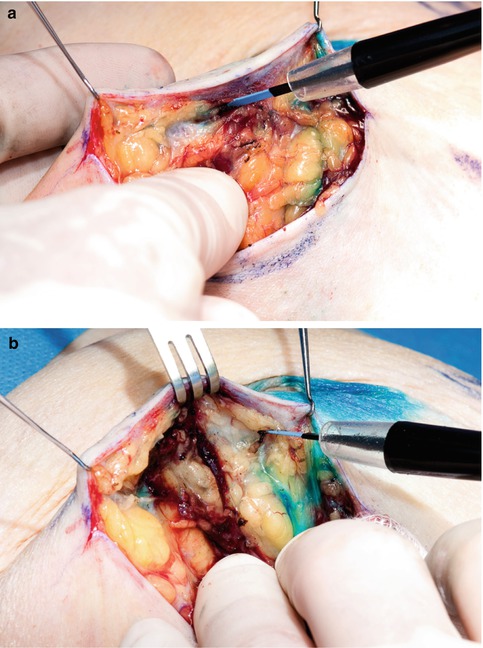
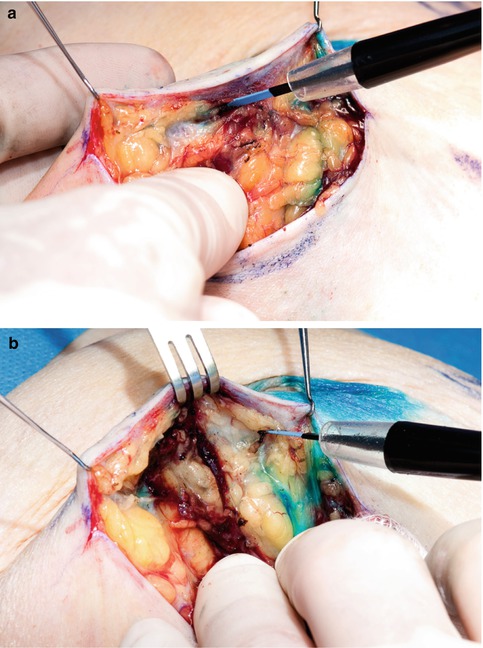
Fig. 7.3
(a, b) Gentle mobilisation of breast tissue from the overlying skin
Gentle mobilisation of the breast tissue avoids application of tension to the tissue during pulling of the purse-string suture. It will also ensure that after application of the purse-string suture, the skin is not drawn in close to the applicator, thereby avoiding the risk of radiation-induced skin necrosis. One needs to ensure that the skin is kept at a minimum distance of 5 mm from the applicator surface, otherwise skin necrosis may result.
Use of broad-spectrum intravenous antibiotics is recommended during the perioperative period.
7.5.2 Application of the Purse-String Suture
After adequate mobilisation of the breast tissue, a purse-string suture is applied to the breast tissue at the tumour bed, around 5 mm away from the edge, at 10-mm intervals until the whole circumference has been covered. It is important to place the applicator and perform a test run before inserting it onto the INTRABEAM in order to ensure that it fits properly and that the purse-string suture draws all the tissue within the tumour bed and conforms the target tissue adequately to the surface of the applicator. When applying the purse-string suture to a fatty breast, special care must be exercised to take good full thickness bites in order to avoid cutting through (“cheese wiring”) the tissue when the purse-string suture is pulled. We recommend using a monofilament material (1/0 prolene) suture with an adequately sized needle. It is preferable to use a blunt needle (Ethiguard blunt point needles) to minimise risk of needle stick injury (Fig. 7.4).
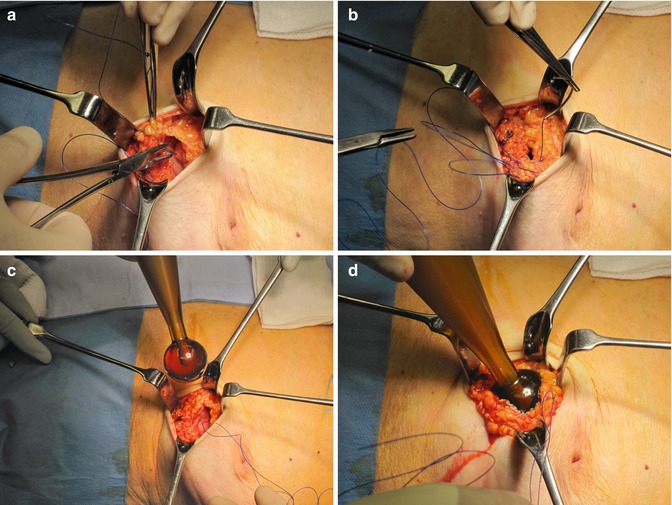
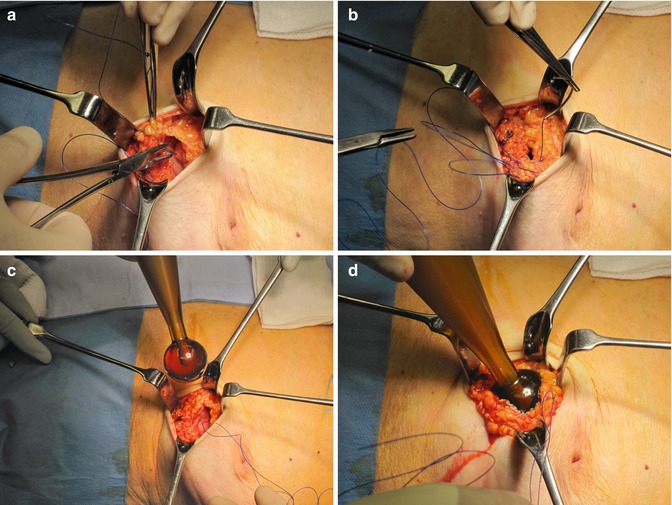
Fig. 7.4
(a–d) Application of the purse string using 1/0 prolene suture. The purse string is tested before the applicator is inserted
7.5.3 Choice of an Appropriately Sized Applicator
After removal of the primary tumour, the WLE specimen and the resultant cavity are measured in three dimensions to guide the choice of applicator size (Fig. 7.5). The applicator should not be too tight, since for radiotherapy to be effective, adequate tissue oxygenation is required. On the other hand, the applicator should not be too loose as the breast tissue needs to be in direct contact with the applicator without any dead space to ensure that an adequate radiation dose is delivered to the tumour bed. If intraoperative ultrasound is available, proximity of the breast tissue to the applicator can be checked during surgery.
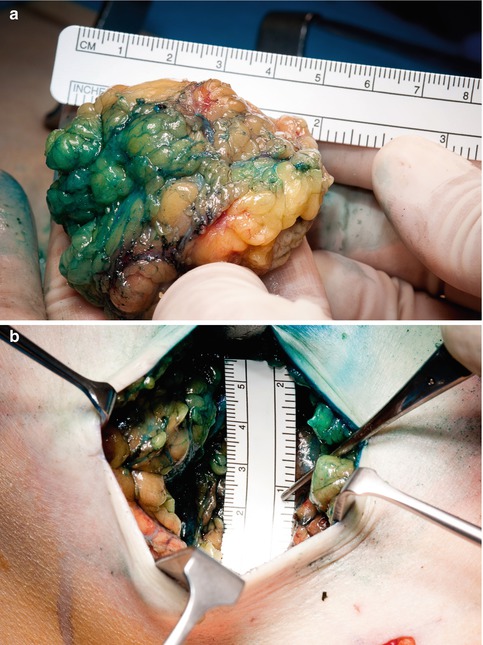

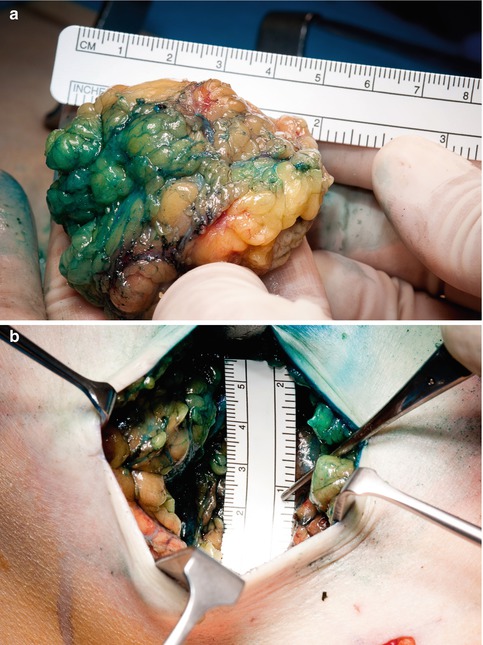

Fig. 7.5




(a–c) Measurement of the specimen and the cavity after WLE to assist in choice of the applicator size
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree